A giant pleural poorly differentiated synovial sarcoma (PDSS) in a 64-year-old woman
Introduction
Synovial sarcoma (SS) is an uncommon malignant soft tissue tumor. It most often affects the lower extremities of young adults (1). The tumor does not arise from the synovium of the joints, but from immature mesenchymal elements, which resembles synovial tissue (2,3). They might differentiate into mesenchymal or epithelial structures. They account for 5–14% of all the soft tissue sarcomas (3,4). In 1996, Gaertner et al. reported the first five cases of SS in the pleural cavity (5). Primary sarcomas of the lungs and pleura are exceedingly rare (6).
Case presentation
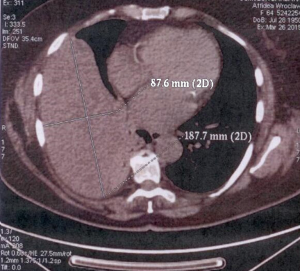
A 64-year-old woman (B.D.), a cigarette smoker (20 pack years of smoking), was admitted to our internal medicine department in February 2015. She complained of the severe pain in the right hypochondriac region increasing on inspiration and body temperature of 37.5 °C. Her past medical history was unremarkable, except for thyroidectomy 14 years ago and arterial hypertension. She was obese as she weighed 105 kg and her BMI was 39 kg/m2. On admission the patient was in good general health. A physical examination revealed an absent vesicular breath sound below the level of the inferior angle of the right scapula (T7). Laboratory studies showed a normal blood morphology and urinalysis. An abdominal USG revealed multiple cholelithiasis. A chest X-ray revealed an extensive opacity in the right middle and lower lung zone. A thoracic CT scan showed a giant mass located in the right hemithorax, measuring 88 mm × 137 mm × 188 mm, and constricting adjacent lung parenchyma (Figure 1). However, a fiberoptic bronchoscopy was in normal limits. A PET scan confirmed the presence of the soft-tissue tumor in the right pleural cavity (max SUV of 2.9), characteristic of a low-grade proliferation process. The patient was transferred to our thoracic surgery department in April 2015 (No 18294/2015). The informed consent was obtained. A right anterolateral thoracotomy was performed under general anesthesia with double lumen endotracheal intubation. After the ligation of the vascular pedicle from diaphragmatic pleura, the pedunculated and well-circumscribed tumor was totally removed (Figure 2). The weight of this lesion was approximately 1.3 kg. Two chest drains were placed. Routine postoperative monitoring was performed. The postoperative recovery was uneventful. The patient was discharged on the 6th postoperative day. The final pathological examination revealed the poorly differentiated synovial sarcoma (PDSS), measuring 70 mm × 140 mm × 170 mm. The resection was R0 with margins histologically free of disease. HE stain showed numerous small round tumor spindle cells with a nuclear pleomorphism (Figure 3A). Immunohistochemistry showed a positive reaction with the monoclonal antibody for CD99 (Figure 3B), wimentin (Figure 3C), and Ki67. But the reactions to LCA, thrombomodulin and cytokeratin CK AE1/AE3 were negative. In July and August 2015 the patient received postoperative adjuvant radiotherapy (60 Gy in 30 fractions over 6 weeks). The patient was healthy on her regular follow-up visits.

Discussion
SS affects the extremities, the head and neck, mediastinum, heart, esophagus, lungs, abdominal wall, mesentery and retroperitoneum. There have been only few cases of primary pleural SS described in the literature so far (1). SS shows no gender predilection (6). Chest pain is the most common complaint, followed by shortness of breath and cough (1). Up to 24% of patients remain asymptomatic (6). Our study confirms that chest pain is the dominant symptom. All patients have large pleural-based intrathoracic masses at presentation (4). The CT scan of SS is characterized as a mass with well-defined margins with no lymph nodes metastasis (3). Pleural SS are usually large (mean size of 13 cm) localized, solid tumors, which grow on a pedicle. Some tumors have a pseudocapsule, so they are well demarcated from the surrounding tissues (7).
SS consists of two different types of cells: epithelial cells and mesenchymal (spindle) cells. It can be classified to four histologic types: biphasic (I); monophasic fibrous (II); monophasic epithelial (III) and poorly differentiated (PD-IV) (4,6). Poorly differentiated type represents up to 20% of all cases (6). The monophasic fibrous type (II) may resemble fibrosarcoma, leiomyosarcoma, malignant peripheral nerve sheath tumor (MPNST), and hemangiopericytoma (2). Histiocytoma, sarcomatoid carcinoma and mesothelioma can mimic SS as well. It is important to exclude a metastasis from an extrathoracic SS. It is difficult to diagnose SS on the basis of histological appearance. Therefore, the immunohistochemical studies must be performed, showing positive reaction (diffuse or focal) to keratin AE1/AE3, EMA, vimentin, CD99, bcl-2, and actin as well as negative reaction for CD34, SMA (smooth muscle actin) and desmin (2,3).
SS is characterized by a t(X;18)(p11.2;q11.2) chromosomal translocation in >90%. This translocation results in the fusion of the SYT gene on chromosome 18 to either SSX1 or SSX2 genes on chromosome X (1,8). It may be detected by the FISH method. However, cytogenetic analysis is not obligatory for the diagnosis (9). In the present study, the cytogenetic examination was not done.
Treatment of choice of SS is a radical surgical resection. It may be followed by radiation therapy and chemotherapy (8). In general, SSs are chemosensitive to ifosfamide and doxorubicin. Due to the rarity of this tumor, which has not permitted controlled studies, there is no consensus on the role of the chemotherapy (9). A careful follow-up is mandatory. The adequate margins of resection seem to be a vital for prevention of local recurrence (6). In the present case the surgical treatment with adiuvant radiotherapy was applied. On the contrary, sarcomatoid mesotheliomas are chemoresistant.
Prognosis of SS is usually poor. The 5-year survival rates range from 50% to 75% (1,4,6,10). Favored prognostic indicators are: young age <20 years, Her-2 expression, complete resection, response to chemotherapy. Poor prognostic factors are: male gender, tumor size larger than 5 cm, truncal location, poor histological differentiation, local recurrence, the SYT-SSX1 variant. Our patient had several poor prognostic factors (older age, large tumor, poor histological differentiation), but she had also some factors of good prognosis (female gender and complete R0 resection).
Conclusions
Pleural SS is a very rare mesenchymal spindle-cell tumor. Its pleural localization represents a diagnostic challenge. There are no guidelines for its optimal treatment. The prognosis of this type of tumor remains still poor.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ng SB, Ahmed Q, Tien SL, et al. Primary pleural synovial sarcoma. A case report and review of the literature. Arch Pathol Lab Med 2003;127:85-90. [PubMed]
- Braham E, Aloui S, Aouadi S, et al. Synovial sarcoma of the chest wall: a case report and literature review. Ann Transl Med 2013;1:9. [PubMed]
- Sudhakar W, Venkata Rao B, Srinivas A, et al. Huge synovial sarcoma arising from chest wall: a rare case report. Journal of Evidence based Medicine and Healthcare 2015;2:597-601.
- Dennison S, Weppler E, Giacoppe G. Primary pulmonary synovial sarcoma: a case report and review of current diagnostic and therapeutic standards. Oncologist 2004;9:339-42. [Crossref] [PubMed]
- Gaertner E, Zeren EH, Fleming MV, et al. Biphasic synovial sarcomas arising in the pleural cavity. A clinicopathologic study of five cases. Am J Surg Pathol 1996;20:36-45. [Crossref] [PubMed]
- Essary LR, Vargas SO, Fletcher CD. Primary pleuropulmonary synovial sarcoma: reappraisal of a recently described anatomic subset. Cancer 2002;94:459-69. [Crossref] [PubMed]
- Travis WD, Churg A, Aubry MC, et al. Mesenchymal tumors. In: Travis WD, Brambilla E, Muller-Hermelink HK, et al., eds. Pathology and genetics of tumors of the lung, pleura, thymus, and heart. Lyon, France: IARC, 2004:141-4.
- Ouadnouni Y, Smahi M, Bouchikh M, et al. A rare tumor of the chest wall: the synovial sarcoma. Pan Afr Med J 2011;9:2. [PubMed]
- Teng C, Li LI, Shen W, et al. Pleural synovial sarcoma patient treated with combined chemotherapy and Endostar, plus sunitinib maintenance therapy: A case report and review of the literature. Oncol Lett 2015;10:1141-1144. [PubMed]
- Srinivasan LP, Bhat RS, Patil S, et al. A Rare Case of Primary Pleural Synovial Sarcoma. Chest 2010;138:27A. [Crossref]



