Correlation analysis of lung cancer and urban spatial factor: based on survey in Shanghai
Introduction
Today lung cancer has become a major cause of death for human being, displaying the highest morbidity among all types of cancers (1). While a total of 1.8 million lung cancer patients increased all around the world and it caused 59 million deaths within the year of 2012, China counts about one third in both mortality and morbidity (2). It is not a surprise when air pollution in Chinese cities, especially the concentration of particulate matter (PM), has become severe, which caused increasing incidence of respiratory disorders, including lung cancer. Under the urgent circumstance, this interdisciplinary study attempt to identify significant factors in urban built environment to respiratory disease.
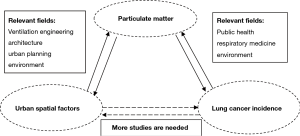
The theoretic framework of this study is built on an interdisciplinary approach, which includes literatures focusing on three types of correlations (Figure 1). The first correlation lies between the PM concentration and the morbidity and mortality of lung cancer. Recent epidemiologic studies in many continents observe negative effects of long-term exposure to particulate air pollution including decreased lung function and increased risk of all-cause, cardiopulmonary, and lung cancer mortality. These respiratory effects of PMs are commonly found in researches regarding U.S. Cities, including cities where the PM concentration at levels below current USA National Ambient Air Quality Stand for particulate pollution (3). For instance, a cohort study through 1982 to 1998 enrolled approximately 500,000 adults proves that long-term exposure to fine particulate air pollution is an important environmental risk factor for lung cancer mortality*. With the controlling of individual risk factors including age, sex, race, weight, height, smoking history, education, marital status, diet, alcohol consumption, and occupational exposures, the study finds that each 10 µg/m3 increase of PM2.5 is associated with approximately a 4%, 6%, and 8% increased risk of all-cause, cardiopulmonary, and lung cancer mortality, respectively (4).
Similar effects are also reported from Europe and Japan. The European Study of Cohorts for Air Pollution Effects has used data from 17 cohort studies based in nine European countries. The meta-analyses show that risk for lung cancer is statistically significant associated with PM10 [hazard ratio (HR) =1.22 (95% CI: 1.03–1.45) per 10 µg/m3] and PM2.5 [HR =1.18 (0.96–1.46) per 5 µg/m3], even at levels below the European Union limit values (5,6). Based on data acquired between 1970 and 1990 for 47 Japanese prefectures, the age-adjusted lung cancer death rates are higher in the southern geographical block of Japan (approximately 1.2-fold in males and 1.1-fold in females) and in the northern block (approximately 1.2-fold in males) than in the central block, which is explained by nitrogen dioxide and temperature (7). As in China, some epidemiologic studies measure the fine particulate matter concentration in specific areas and cities and find its mutagenicity and carcinogenicity (8,9).
The second correlation lies between urban built environment and PM concentration. Empirical studies have conducted to identify significant factors of built environment that influence PM concentration in cities, such as Hong Kong, Beijing, Shanghai, Guangzhou, Qingdao and Ningbo. It has demonstrated that the mass concentrations of total suspended particulate (TSP), PM10 and PM 2.5 vary in different areas within a same city (10-13). Researches particularly prove the significant influences of land use types (14-18) and building density (19-21), green space (10), water body (22), location of highway entrance (23), traffic patterns (24,25) and street scale (26,27) upon particulate matter concentration and distribution.
The third correlation focuses on the morbidity of respiratory disease and urban built environment, in addition to inherent physiological determinants and lifestyle such as cigarette consuming, cooking oil fumes, etc. There are emerging studies about the implication of built environment in explain in explaining health outcomes (28-31), especially neighborhood environment (32,33). Empirical researches have provided evidence about how household quality, ventilation condition, indoor humidity, and street congestion are linked to respiratory diseases (34-36). Specific land use types are also found correlated to respiratory health. For instance, residences near industrial areas are significantly associated with various disease incidences including lung cancer (37-39); green spaces have a positive impact on health, including decreasing respiratory disease mortality (40-42), while the impact may not always significant in certain areas (43). Meanwhile, since high traffic volume increases incidence rate of pulmonary adenoma (44,45), living within 100 m from highways has a negative impact on respiratory health for both children (46,47) and adults (48). Current studies have respectively explored the indoor and outdoor factors on respiratory diseases. More comprehensive spatial factors need to be analyzed to understand the cumulative effect of built environment upon respiratory diseases and identify the possible causation.
This paper, therefore, investigate the correlation between lung cancer morbidity and both indoor and outdoor factors of urban built environment in a comprehensive approach. We hypothesize that the broad range of urban spatial factors affect lung cancer incidence not only by patterning particulate matter distribution but also in other ways. Indoor and outdoor factors are selected to test the hypothesis after adjusting individual level factors. The study aims to reducing the morbidity of respiratory disease through the adjustment of external factors on the one hand, on the other hand providing new clues for lung cancer screening of high-risk individuals.
Methods
Data collection
The study is a hospital-based case-control study conducted at the Renji Hospital affiliated to Shanghai Jiao Tong University School of Medicine. All samples/patients have been informed about the content of this study for the publication of this article. A structured questionnaire has been adopted in the survey started in March 2014 and ended in May 2015. Data are collected from the total of 472 participants, including 202 incident cases of lung cancer and 270 controls. Controls are selected among normal people attending the hospital for physical examinations who are unrelated to respiratory disorders. Both cases and controls are required to reside within the center city of Shanghai for more than 5 years. The central city of Shanghai, defined by the outer circle of highway of Shanghai, covers a total area of 660 square kilometers. Mostly of the central city of Shanghai presents relevant high density of buildings, which provides the study site with rich spatial factors. We randomly select cases and controls with the entire data to conduct a frequency matched case-control study by age (±7.5 years) and gender. The final study population comprises a total of 312 samples with 156 matched pairs.
The collected data cover both socioeconomic features of individual and spatial factors of built environment of their residences. Certain spatial factors are identified and measured through satellite maps and the software of geographic information system (GIS) with the addresses of surveyed individuals.
Variable definitions
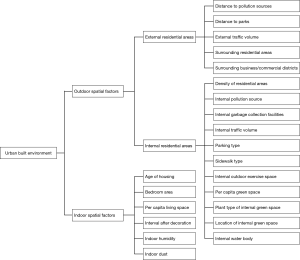
In the models for correlation analysis, we identify the lung cancer incidence as the dependent variable, individual level factors including socio-economic status and lifestyle as the control variables. The independent variables cover both indoor and outdoor factors to conduct a more comprehensive exploration of the built environment (Figure 2).
Dependent variable: lung cancer incidence
The main health outcome we focus on is lung cancer incidence based on confirmed clinical diagnosis.
Control variables: individual level factors
Individual level factors as the control variables attempt to capture the socio-economic status and lifestyle of surveyed residents that influence their health outcome. Age, gender, working environment, tobacco consumption (smoking history and family/colleague smoking status), cooking fume exposure, outdoor exercise duration, and chronic medical history are identified according to the individual level risk factors for lung cancer listed in the National Comprehensive Cancer Network (NCCN) guideline in the US for lung screening and relevant studies (49).
Among all these factors, we collect information about occupation, working environment and duration of the job and then focus on jobs for a minimum duration of 6 months or longer. Occupations are categorized into high-risk or non-high-risk for lung cancer, and then participants in the survey are classified into three groups accordingly, including unexposed individual that have never worked in a high-risk job, individual that have worked <35 years in a high-risk job, and individual that have worked ≥35 years in a high-risk job. This 35-year breaking point is identified based on the statistic of the control group, in which 75% (three quarter) individuals working in a high-risk environment have lasted for less than 35 years.
As for tobacco consumption, surveyed individuals are categorized based on their smoking history and family/colleague smoking status. Smoking history is divided into two groups: non-smokers, defined as subject who has not smoked in the entire lifetimes; and former and current smokers, defined as regular smokers who has smoked for at least 1 year. Family/colleague smoking status describes whether or not subject were exposed to second-hand smoke.
For Chinese family, exposure to cooking fume is traced as one of the risk for lung cancer (50-52). It is categorized according cooking habit of the surveyed individual into four degrees, including never cook (subject who do not cook daily); steam preferred (adopting steam as main cooking method), stir-fry preferred and fry preferred.
Furthermore, outdoor exercise duration, as an important indicator for lifestyle, is defined as the average outdoor excise time per day for the surveyed individual. We also include the chronic medical history as a two-level factor (0 vs. 1) that is confirmed by clinical diagnosis.
Independent variable group 1: outdoor spatial factors
The data of outdoor spatial factors are derived from the individual survey and the estimation of researchers through the software of GIS. We geocode the subjects’ address and measure certain variable in the GIS. Twenty seven variables are identified to describe 15 outdoor spatial factors. The study adopts the residential area as a spatial unit, categorizing the variables into the external and internal factors of the subjects’ residential areas.
The external factors of residential area include measures of distance to pollution sources, distance to parks, external traffic volume and development intensity of the surrounding area of the subjects’ neighborhood. Distance to pollution sources and distance to parks are represented by the distance of the neighborhood to the nearest pollution source and park. Living nearby pollution source such as industrial areas could add risk on lung cancer incidence (34-36), while green spaces on the contrary are assumed having positive impacts on healthy outcome (40-42). External traffic volume, an important pollutant source, is described through a five-category score in the survey. The variable of development intensity of the surrounding area aims to describe the ventilation of the subjects’ neighborhood, which may present negative influence on residents’ respiratory health. It also attempts to capture land use mix and density, which may have a positive influence on health through accessibility and walking opportunity. Because 2 kilometer is a comfortable walking distance for daily life (53), the study adopts 2 kilometer as the radius to define the surrounding area of a neighborhood. We basically categorize the surrounding residential blocks and commercial/business blocks by the average heights, namely low story (1-3F), multi story (4-6F), middle height (7-9F) and high-rise (over 10F). The models we built in the study may provide clues to analyze the controversial factors of development intensity.
The internal factors of residential area describe the built environment within the subjects’ resident areas that may influence respiratory health. It includes measures of building density, presence of internal pollution source, internal traffic volume, parking type, sidewalk type, outdoor exercise space, green space (area per capita/ plant type/ location) and presence of internal water-body. Among these factors, the building density of the neighborhoods, which affects particulate matter diffusion and distribution, is defined as building density and reported by four-category scores. The presence of internal pollution source, outdoor exercise space and internal water-body is represented as a two-level factor in terms of case and non-case. Internal traffic volume, same as the external traffic volume, is reported through five-category scores. Internal pollution source and internal traffic volume may both release particulate matter and other harmful substances. Outdoor exercise space in a neighborhood provides opportunity to exercise but may also add exposure to air pollution. Internal water-body may mitigate air pollution such as particulate matter concentration. Parking type is defined as non-parking (no vehicles parking lot inside a neighborhood), ground parking (vehicles mainly parking on the ground such as roadside); garage parking (parking underground or inside garages). We divided sidewalk type into two categories: shared sidewalk (residents walking along with vehicles on the same road section) and divided sidewalk. The type of parking and sidewalk, as important design elements in residential area planning, provides different degree of residents’ exposure to vehicle and its associated PM. Internal green space is represented through total area per capita, main plant type and location. Main plant type of internal green space is described as lawn, bush and tree, which influence the concentration of PM in different ways. Location of internal green space include scattered (no central green space in a neighborhood), center (large scale green space located at the center of a neighborhood), and near the exit. Similar to green space outside residential area, internal green space can attribute to outdoor exercise while increase the exposure of PM to certain extent.
Independent variable group 2: indoor spatial factor
The data of indoor spatial factors are collected based on individual survey. Six variables are identified to describe 6 indoor spatial factors. The variable titled age of housing aims to represent the duration of housing in usage. Individuals’ bedroom area and total area of living space per capita represents ventilation quality of housing. Interval after decoration represents the time between decoration and move-in, because housing units provided in China are usually unfurnished and need decoration after purchase. It may cause volatile organic emission during and after decoration. Both indoor humidity and indoor dust are reported into three levels according to the observation of surveyed individuals, which related to exposure to harmful substance to the residents.
Statistical methods
Two-level logistic regression models are adopted to evaluate possible impact of urban built environment upon lung cancer. Certain adjustments are made based on matching factors (age and gender) and other socio-demographic and lifestyle factors, such as smoking and work environment. To avoid possible confounding, we test the correlation between each of the independent variables. It is found that bedroom area and per capita living space are significantly correlated with age of housing—bigger area is associated with newer houses, due to the development evolution of house type in China. So bedroom area and per capita living space are not brought into the models.
We select unconditional logistic regression including matching characteristics in the model because it is a standard methodology when conducting a frequency-matched study, especially when matching characteristics provide high opportunity to prepare cases and controls. With age and gender as the matching characteristics in this study, cases and controls have been paired and the corresponding pairs are interchangeable among the same age group and gender.
Results
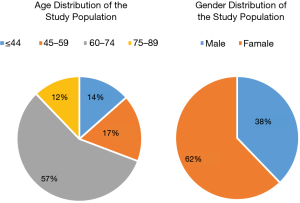
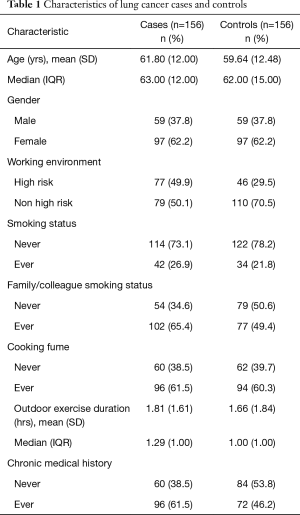
The correlation analysis includes 156 pairs and controls matched by age (±7.5 years) and gender (Figure 3). The discriptive statistics of age, gender, work environment, smoking history, cooking fumes exposure, outdoor exercise duration and chronic medical history are summarized (Table 1). Among these, the work environment, smoking history and chronic medical history are criteria for selecting high-risk individuals for lung cancer screening in the guideline of National Comprehensive Cancer Network of the USA (49). There are more samples working in high-risk environment and suffering chronic disease among cases than among controls (36.6% vs. 19.6%; 61.4% vs. 44.4%), while tobacco consuming presents no obvious difference in the two groups.
Full table
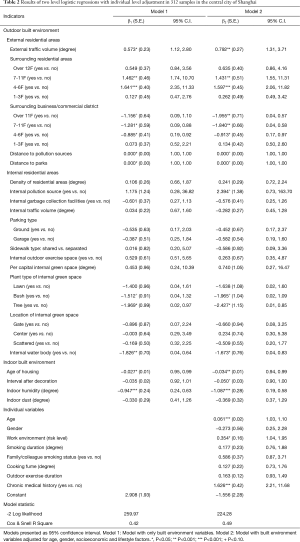
The results of two-level logistic regressions are presented in Table 2. Both outdoor and indoor built environment indicators are included in model 1, and adjustments are made to age, gender as well as lifestyle factors in model 2. Model fit is assessed by -2 Log likelihood and Cox & Snell R Square with larger values indicating better fit. R Square equal to 0.42 and 0.49 in model 1 and model 2 respectively, which are both acceptable.
Full table
In model 1, 9 of the 20 spatial factors measured by 31 variables are significantly associated with lung cancer. Among the external factors of residential area, external traffic plays a significant role in predicting lung cancer incidence. Higher external traffic volume presents a significant association with higher lung cancer incidence (B=0.573, P<0.05). Neighborhoods surrounded with residential blocks (within 2 km radius) are significantly associated with increasing lung cancer incidence (B for 4-6 floors=1.641, P<0.001; B for 7-9 floors=1.462, P<0.01). Surrounded with commercial/business districts is inversely associated with lung cancer prevalence (B for 4-6 floors=−0.885, P<0.05; B for 7-9 floors=-1.281, P<0.05). Shorter distance to pollution source (B=−0.0003, P<0.05) within the defined buffer (4 km radius) is associated with increasing lung cancer incidence. Distance to parks (B=−0.0002, P<0.05) presents negatively correlated to health that is contrary to common sense. In respect of internal residential area, green space covered with trees (B=−1.969, P<0.05) and water body (B=−1.826, P<0.01) inside residential areas are associated with lower lung cancer prevalence. As for indoor environment, elder age of housing is associated with lower lung cancer incidence (B=−0.027, P<0.05). Higher indoor humidity level is associated with lower lung cancer incidence (B=−0.947, P<0.001), which is contrary to previous studies (54). Indoor dust present none significance.
In model 2, further adjustments to match factors (age, gender), socio-demographic and lifestyle factors are made. We find lung cancer significantly correlated with age (B=0.061, P<0.001), work environment (B=0.354, P<0.05) and chronic medical history (B=1.626, P<0.001). Smoking duration, family/colleague smoking status, cooking fume, and outdoor exercise duration present insignificant in the model. The individual variables made no substantial difference to associations between lung cancer and built environment factors. Only two factors significant in model 1 including distance to outside pollution source and park present insignificant in model 2. The rest of significant factors in model 1 keep similar confidence level and +/− correlation.
Discussion
In this study, we investigate the effects of urban built environment both outdoor and indoor on lung cancer in high-density urban area of central Shanghai. The built environment factors identified significantly correlated with lung cancer morbidity include external traffic volume, surrounding land use type, plant type of internal green space, internal water-body, age of housing and indoor humidity.
Certain spatial factors of built environment that influence particulate matter concentration are significantly related to lung cancer prevalence in the models. Before and after adjustment to individual level socio-demographic and lifestyle confounders, external traffic volume producing PMs presents highly significant correlation with lung cancer incidence. The negative effect of heavy external traffic volume upon lung cancer morbidity is consistent with previous findings that high density of traffic may lead to heavy particulate matter emission (41,42). On the other hand, internal water-body and green space mainly covered with trees are considered as spatial factors that mitigate the concentration of PMs. Water-body and plants may absorb particulate matters and open space could promote particulate matter diffusion (55,56). It proves that the presence of water-body and green space may have positive effect to decrease the lung cancer morbidity. While cross-sectional studies have reported similar results (10), the study provides more detailed comparison among plant types of green space. Trees present significant correlation with lower lung cancer morbidity, while both lawn and bush do not. It may implicate that more trees than lawn and bush in green space within neighborhoods could lead to lower respiratory disease prevalence.
Other factors of built environment that indirectly relevant to particulate matter distribution also exhibit significant association with lung cancer prevalence. Neighborhoods surrounded with residential buildings from 4 to 11 floors (including variables: 4–6 floors, 7−11 floors) present significant correlation with lung cancer morbidity. It can be explained that the emission and concentration of PMs produced by cooking. Comparing to neighborhoods surrounded with business/commercial blocks, it presents contrary effect. It indicates that higher land use mix may be associated with less respiratory disease prevalence. Better land use mix may lead to higher walkability and more physical excise (57). Meanwhile, age of housing is associated with lung cancer. New buildings lead to higher lung cancer morbidity. It indicates that building materials may cause indoor air pollution, which brings risk on lung cancer. Higher level of indoor humidity is associated with less lung cancer morbidity appears contrary to the general understanding that humidity is considered as a poor environment. Because the surveyed individuals instead of field measure report this data, it may be explained that the presence of mildew spots are noticed by who pay more attention to indoor environment quality and then lower the possibility of respiratory disease.
Based on the result of modeling, the study attempts to provide different angle to rethink about screening that can contribute to early detection and therefore improve survival rates. The America National Lung Screening Trial (NLST) has assessed the ability of low-dose computed tomography (LDCT) scans to decrease lung cancer-specific mortality by 20% (58). The current guidance of lung cancer screening for high-risk individuals basically follows the National Comprehensive Cancer Network (NCCN) of the United States. It has been developed in 2011 and updated every year.
The NCCN guideline describes risk factors for lung cancer including smoking history (present or past), radon exposure, occupational exposure, cancer history, disease history (COPD or pulmonary fibrosis), smoking exposure (second-hand smoke) and absence of symptoms or signs of lung cancer etc. It recommends the following two types of individuals need screening: (I) aged 55 to 74 years; 30 or more pack-year history of smoking tobacco and quit within 15 years; (II) aged 50 years or older, 20 or more pack-year history of smoking tobacco, and one additional risk factor (other than second-hand smoke). It basically focuses on age and smoking exposure. However, other risk factors should be considered, especially in China where has experienced an increasing air pollution. Smoking duration and family/college smoking status, which are regarded as regular causes, present insignificant correlation to lung cancer morbidity based on the modeling of the survey data. External traffic volume, surrounding land uses, presence of green space/water-body and age of housing present their significance. Non-smoking female patients are increasing recently (59,60). It indicates that the causes of lung cancer in China are more complicated than smoking. When external factors of air quality lead to high morbidity of respiratory disease combining with individual factors, it brings clue to rethinking about the screening standards. Certain features of neighborhoods can be listed as additional risk factors for respiratory system. We propose that high-risk individual screening could more consider the following conditions when residents living in a neighborhood within high-density urban area for more than 5 years:
- High traffic volume outside the neighborhood, such as residential areas near highways/elevated highway, highway ramps, arterials, and tunnel exits, especially with frequent congestion;
- Residential as the singular land use surrounding the neighborhood, such as within 2 kilometer radius;
- Absence of green space inside the neighborhood, or absence of leafy plants in green space.
These factors have been identified as risky built environment in this cross disciplinary study. Lung cancer screening need to consider the potential patients living in these neighborhoods, with a combination of their individual variables such as age, working environment and chronic medical history.
This study provides detailed assessment of diverse aspects of both outdoor and indoor built environment based on a multi-level modeling. A range of covariates are taken into analysis to reduce the possibility of confounding and reverse causation. Limitations of the study include the assumption that environment conditions have not dramatically changed over the participants’ reported period. Wider range and longitudinal data are required to provide more convincing evidence. Further research shall address complex causal path through which built environment affects health outcome can be drawn. This study initiates the approach to explore the correlation between respiratory disease and spatial factors in order to improve long term public health.
Acknowledgements
Funding: This work was supported by National Nature Science Foundation of China (51578384) and Science and Technology Commission of Shanghai Municipality, China (14411951200).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Tan W. Cancer rates climb. Shanghai Daily. May 28, 2013. Available online: http://www.shanghaidaily.com/feature/Cancer-rates-climb/shdaily.shtml
- McGuire S. World Cancer Report 2014. Geneva, Switzerland: World Health Organization, International Agency for Research on Cancer, WHO Press, 2015. Adv Nutr 2016;7:418-9. [Crossref] [PubMed]
- Pope CA 3rd, Bates DV, Raizenne ME. Health effects of particulate air pollution: time for reassessment? Environ Health Perspect 1995;103:472-80. [Crossref] [PubMed]
- Pope CA 3rd, Burnett RT, Thun MJ, et al. Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 2002;287:1132-41. [Crossref] [PubMed]
- Raaschou-Nielsen O, Andersen ZJ, Beelen R, et al. Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE). Lancet Oncol 2013;14:813-22. [Crossref] [PubMed]
- Beelen R, Raaschou-Nielsen O, Stafoggia M, et al. Effects of long-term exposure to air pollution on natural-cause mortality: an analysis of 22 European cohorts within the multicentre ESCAPE project. Lancet 2014;383:785-95. [Crossref] [PubMed]
- Choi KS, Inoue S, Shinozaki R. Air pollution, temperature, and regional differences in lung cancer mortality in Japan. Arch Environ Health 1997;52:160-8. [Crossref] [PubMed]
- Yu SY, Guan NY, Zhang DS, et al. Mutagenicity and carcinogenicity of indoor particles with different sizes from high prevalence areas of lung cancer in Xuanwei County. Journal of Environment and Health 1993;2:001. Available online: http://www.cnki.com.cn/Article/CJFDTOTAL-HJYJ199302001.htm
- Gao N, Zhang XL, Zhuo JB, et al. Mutagenicity and carcinogenicity of different diameters of air particles in residential areas in Chongqing City [J]. Carcinogenesis, Teratogenesis & Mutagenesis 1995;5.
- Chan LY, Kwok WS, Lee SC, et al. Spatial variation of mass concentration of roadside suspended particulate matter in metropolitan Hong Kong. Atmospheric Environment 2001;35:3167-76. [Crossref]
- Kim KH, Lee HS, Youn YH, et al. Studies of Spatial Variabilities of Airborne Metals Across Four Different Land-Use Types. Water Air and Soil Pollution 2002;138:7-24. [Crossref]
- Yang GL, He ZJ, Han P, et al. Analysis for distribution of suspended particle in Guangzhou resident environment. Optoelectronic Technology & Information 2002;15:9-13.
- Sun Y, Zhuang G, Wang Y, et al. The air-borne particulate pollution in Beijing—concentration, composition, distribution and sources. Atmospheric Environment 2004;38:5991-6004. [Crossref]
- Wang M, Beelen R, Basagana X, et al. Evaluation of land use regression models for NO2 and particulate matter in 20 European study areas: the ESCAPE project. Environ Sci Technol 2013;47:4357-64. [Crossref] [PubMed]
- Boëchat IG, Krüger A, Chaves RC, et al. Land-use impacts on fatty acid profiles of suspended particulate organic matter along a larger tropical river. Sci Total Environ 2014;482-483:62-70. [Crossref] [PubMed]
- Amini H, Taghavi-Shahri SM, Henderson SB, et al. Land use regression models to estimate the annual and seasonal spatial variability of sulfur dioxide and particulate matter in Tehran, Iran. Sci Total Environ 2014;488-489:343-53. [Crossref] [PubMed]
- Hoa CC, Chana CC, Cho CW, et al. Land use regression modeling with vertical distribution measurements for fine particulate matter and elements in an urban area. Atmospheric Environment 2015;104:256-63. [Crossref]
- Xu H, Bi XH, Zheng WW, et al. Particulate matter mass and chemical component concentrations over four Chinese cities along the western Pacific coast. Environ Sci Pollut Res Int 2015;22:1940-53. [Crossref] [PubMed]
- Dannenberg AL, Jackson RJ, Frumkin H, et al. The impact of community design and land-use choices on public health: a scientific research agenda. Am J Public Health 2003;93:1500-8. [Crossref] [PubMed]
- Weng Q, Yang S. Urban air pollution patterns, land use, and thermal landscape: an examination of the linkage using GIS. Environ Monit Assess 2006;117:463-89. [Crossref] [PubMed]
- Schweitzer L, Zhou J. Neighborhood Air Quality, Respiratory Health, and Vulnerable Populations in Compact and Sprawled Regions. Journal of the American Planning Association 2010;76:363-71. [Crossref]
- Furuuchi M, Murase T, Yamashita M, et al. Temperature Distribution and Air Pollution in Phnom Penh, Cambodia - Influence of Land Use and the Mekong and Tonle Sap Rivers. Aerosol and Air Quality Research 2006;6:134-49.
- Lee HK, Lee B, Jeong E, et al. Analysis of Particulate Concentrations at Highway Areas in Ulsan. IEEE 2006. Available online: http://ieeexplore.ieee.org/document/4107422/
- Levy JI, Bennett DH, Melly SJ, et al. Influence of traffic patterns on particulate matter and polycyclic aromatic hydrocarbon concentrations in Roxbury, Massachusetts. J Expo Anal Environ Epidemiol 2003;13:364-71. [Crossref] [PubMed]
- Kaur S, Nieuwenhuijsen MJ, Colvile RN. Fine particulate matter and carbon monoxide exposure concentrations in urban street transport microenvironments. Atmospheric Environment 2007;41:4781-810. [Crossref]
- Wang JW, Wang W. Space form and pollutant distribution in urban street canyons:a case study of hangzhou zhongshan road. City Planning Review 2010;12:57-63.
- Wang JW, Zhang C, Feng YJ. Research review and response framework in urban planning for air pollution in urban street canyons. Urban Development Studies 2012;5:82-7.
- Barton H, Tsourou C. Health urban planning: A WHO guide to planning for people. London/Copenhagen:Spon/WHO. 2000.
- Hoehner CM, Brennan LK, Brownson RC, et al. Opportunities for integrating public health and urban planning approaches to promote active community environments. Am J Health Promot 2003;18:14-20. [Crossref] [PubMed]
- Galea S, Ahern J, Rudenstine S, et al. Urban built environment and depression: a multilevel analysis. J Epidemiol Community Health 2005;59:822-7. [Crossref] [PubMed]
- Bai X, Nath I, Capon A, et al. Health and wellbeing in the changing urban environment: complex challenges, scientific responses, and the way forward. Current Opinion in Environmental Sustainability 2012;4:465-72. [Crossref]
- Meade MS. Medical Geography. John Wiley & Sons Ltd 1988.
- Qi L, Zhou S, Yan X, et al. Trend and hot topics of medical geography. Progress in Geography 2013;32:1276-85.
- Krewski D, Lubin JH, Zielinski JM, et al. Residential radon and risk of lung cancer: a combined analysis of 7 North American case-control studies. Epidemiology 2005;16:137-45. [Crossref] [PubMed]
- Miles R, Jacobs DE. Future Directions in Housing and Public Health: Findings From Europe With Broader Implications for Planners. Journal of the American Planning Association 2008;74:77-89. [Crossref]
- Herrin WE, Amaral MM, Balihuta AM. The relationships between housing quality and occupant health in Uganda. Soc Sci Med 2013;81:115-22. [Crossref] [PubMed]
- Benedetti M, Iavarone I, Comba P. Cancer risk associated with residential proximity to industrial sites: a review. Arch Environ Health 2001;56:342-9. [Crossref] [PubMed]
- Cambra K, Martínez-Rueda T, Alonso-Fustel E, et al. Mortality in small geographical areas and proximity to air polluting industries in the Basque Country (Spain). Occup Environ Med 2011;68:140-7. [Crossref] [PubMed]
- López-Cima MF, García-Pérez J, Pérez-Gómez B, et al. Lung cancer risk and pollution in an industrial region of Northern Spain: a hospital-based case-control study. Int J Health Geogr 2011;10:10. [Crossref] [PubMed]
- Richardson EA, Mitchell R. Gender differences in relationships between urban green space and health in the United Kingdom. Soc Sci Med 2010;71:568-75. [Crossref] [PubMed]
- Groenewegen PP, van den Berg AE, Maas J, et al. Is a green residential environment better for health? If so, why? Annals of the Association of American Geographers 2012;102:996-1003. [Crossref]
- Kardan O, Gozdyra P, Misic B, et al. Neighborhood greenspace and health in a large urban center. Sci Rep 2015;5:11610. [Crossref] [PubMed]
- Richardson E, Pearce J, Mitchell R, et al. The association between green space and cause-specific mortality in urban New Zealand: an ecological analysis of green space utility. BMC Public Health 2010;10:240. [Crossref] [PubMed]
- Chen F, Jackson H, Bina WF. Lung adenocarcinoma incidence rates and their relation to motor vehicle density. Cancer Epidemiol Biomarkers Prev 2009;18:760-4. [Crossref] [PubMed]
- Xiang YB, Chen W, Li HL, et al. A cohort study on risk factors of lung cancer among non-smoking women in urban Shanghai. National Epidemiology and Etiology of Cancer Conference Proceedings. 2011. Available online: http://cpfd.cnki.com.cn/Article/CPFDTOTAL-ZGKA201107001017.htm
- van Vliet P, Knape M, de Hartog J, et al. Motor vehicle exhaust and chronic respiratory symptoms in children living near freeways. Environ Res 1997;74:122-32. [Crossref] [PubMed]
- McConnell R, Berhane K, Yao L, et al. Traffic, susceptibility, and childhood asthma. Environ Health Perspect 2006;114:766-72. [Crossref] [PubMed]
- Wallace J, D'silva L, Brannan J, et al. Association between proximity to major roads and sputum cell counts. Can Respir J 2011;18:13-8. [Crossref] [PubMed]
- Wood DE, Kazerooni E, Baum SL, et al. Lung cancer screening, version 1.2015: featured updates to the NCCN guidelines. J Natl Compr Canc Netw 2015;13:23-34. [PubMed]
- Ko YC, Lee CH, Chen MJ, et al. Risk factors for primary lung cancer among non-smoking women in Taiwan. Int J Epidemiol 1997;26:24-31. [Crossref] [PubMed]
- Ko YC, Cheng LS, Lee CH, et al. Chinese food cooking and lung cancer in women nonsmokers. Am J Epidemiol 2000;151:140-7. [Crossref] [PubMed]
- Yu IT, Chiu YL, Au JS, et al. Dose-response relationship between cooking fumes exposures and lung cancer among Chinese nonsmoking women. Cancer Res 2006;66:4961-7. [Crossref] [PubMed]
- Feng HX, Zhang SR. Study on travel efficiency and land use mixing degree based on meta fractal dimension theory: a case study of Yulin airport eco-city. Journal of Xi'an University of Architecture & Technology 2014;6:882-7. (Natural Science Edition).
- Dong B, Ge N, Liu G. Social economical status, behaviors and environment as the risk factors of tuberculosis in Chengdu China. Zhonghua Liu Xing Bing Xue Za Zhi 2001;22:102-4. [PubMed]
- Fu W, Zheng Y, Dong J. Diurnal Change of Air Particulate Concentration in 3 Types of Land in Winter Campus. Journal of Chinese Urban Forestry 2013;6:15-8.
- Jiao L, Xu G, Zhao S, et al. LUR-based simulation of the spatial distribution of PM2.5 of Wuhan. Available online: https://www.researchgate.net/publication/282939480_LUR-based_simulation_of_the_spatial_distribution_of_PM25_of_Wuhan
- Heath GW, Brownson RC, Kruger J, et al. The Effectiveness of Urban Design and Land Use and Transport Policies and Practices to Increase Physical Activity: A Systematic Review. Journal of Physical Activity and Health 2006;3:S55-S76. [Crossref]
- National Lung Screening Trial Research Team, Aberle DR, Adams AM, et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011;365:395-409. [Crossref] [PubMed]
- Samet JM, Avila-Tang E, Boffetta P, et al. Lung cancer in never smokers: clinical epidemiology and environmental risk factors. Clin Cancer Res 2009;15:5626-45. [Crossref] [PubMed]
- Oberg M, Jaakkola MS, Woodward A, et al. Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet 2011;377:139-46. [Crossref] [PubMed]