Effectiveness of lung ultrasonography for diagnosis of pneumonia in adults: a systematic review and meta-analysis
Introduction
Pneumonia has been documented as a forgotten killer for human health. According to the data released by World Health Organization, lower respiratory tract infection is the leading cause of infectious disease related mortality worldwide and refers to the top ranking death reason in low-income countries (1). Despite the rapid advances of therapeutic strategy, community acquired pneumonia (CAP), hospital-acquired pneumonia (HAP) and ventilator-associated pneumonia (VAP) remain dramatic clinical burden. It has been well-documented that timely administration of antibiotics to patients admitted with pneumonia improves prognostic outcome. However, appropriate intervention must be based on swift and accurate recognition. The signs and symptoms localizing to the respiratory system, commonly referring as dyspnea, cough and fever, laboratory alterations (leukocytosis and increased c-reactive protein/procalcitonin) in conjunction with radiographic pulmonary infiltrate, point to convincing diagnosis of pneumonia. Imaging evaluation approaches recommended on current guidelines are chest radiograph and chest computerized tomography (CT) (2,3). However, limitations for their use exist (4). Surprisingly, a recent study compared CXR to chest CT scan for suspected CAP. They found up to 30% false positive and false negative rate of CXR in emergency department (ED), which doubted the value of CXR on pneumonia diagnosis (5). Thus, it’s reasonable to figure out the alternative way to provide promising imaging evidence of pneumonia.
Ultrasonography is gaining more attention in critical care and emergency medicine. A good body of studies has proven that ultrasonography is highly effective in evaluating multiple pulmonary diseases, such as metastatic lymph node of lung cancer, pleural effusions, pneumonia and pneumothorax (6-9). The pilot study by Benci and colleagues reported that the diagnostic sensitivity of the ultrasound (US) on pneumonia was comparable to that of conventional radiology (10). Although accumulated evidence from other independent groups also showed the superiority in favor of US over chest radiography (11), US remained underused. To date, guidelines is still too conservative to introduce lung US (LUS) as an alternative to chest X-ray (CXR) and chest CT for rapid diagnosis of pneumonia (2,3,12).
Hence, we sought to comprehensively summarize the data from current available literature. Seven publications which were not analyzed before were taken into consideration, and studies with unspecific diagnosis were excluded. We aim to undertake an accurate meta-analysis to clarify the role of LUS in the diagnosis of pneumonia in adults.
Methods
Study design and data sources
We conducted a systematic search to identify original articles in English in PubMed and EMBASE up to the end of May 2016, using the combinations of the following key words: (“ultrasound” or “sonography” or “ultrasonography”) and (“pneumonia”) and (“sensitivity”) and (“specificity”), limited to clinical/observational trials. All eligible studies were retrieved. Bibliographies of retrieved articles were searched independently and confirmed in case of additional articles to ensure the completeness and quality of the analysis. Trials published solely in abstract form as well as unpublished data were not included.
Study selection
Studies were included according to the criteria as follow: (I) adults with suspected pneumonia; (II) original articles assessing the diagnostic power of LUS for pneumonia; (III) comparison of LUS findings with composite standard based on chest CT scan, clinical presentation, CXR or microbiology where applicable; (IV) detailed values at least containing true-positive, true-negative, false-positive, and false-negative results that allows reconstruction of the original data; (V) clarification of the imaging alterations on LUS indicating pneumonia in clear details; (VI) meeting study quality standards in accordance with the revised Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool (13). Two independent investigators reviewed the articles to exclude irrelevant and overlapping studies, with disagreements resolved via consensus. Compared with previous meta-analysis on the same topic, seven publications which were not analyzed before were taken into consideration, and studies with unspecific diagnosis were excluded.
Quality of study reports
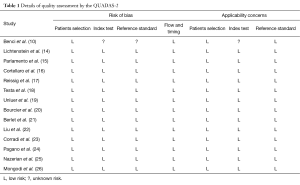
Methodological quality of studies was scored by QUASAS-2 system. Seven items listed in Table 1 may be categorized into low, high and unclear in terms of risk bias and study generalizability. Two independent investigators were assigned to perform the assessment. Disagreements were resolved by discussions.
Full table
Data extraction
We collected the following information from the included studies: first author’s surname, year of publication, sample size, gender proportion, mean age, LUS technique, evaluating positions, LUS alterations identified for pneumonia, expertise of operator, as well as the values of true-positive, true-negative, false-positive, and false-negative. Any disagreement was resolved by consensus via discussions or with a third reviewer when necessary.
Data analysis
Meta-DiSc (version 1.4, Ramony Cajal Hospital, Madrid, Spain) and MedCalc Statistical Software version 16.2.1 (MedCalc Software bvba, Ostend, Belgium) were employed into our analysis. Pooled sensitivity and specificity with corresponding 95% confidence intervals were computed by Mantel-Haenszel method of the random-effect model, and pooled diagnostic odd ratio (DOR) was calculated by the DerSimonian-Laird method (27). The Spearman correlation coefficient between the logit of sensitivity and 1-specificity was calculated to test the threshold/cutoff effect. Heterogeneity assumptions were quantified by inconsistency index (I2). I2 values of 25%, 50% and 75% represented low, moderate and high degree of heterogeneity, respectively (28). Funnel plot and Egger’s regression asymmetry test were used to anticipate the publication bias of literature. A P value of <0.05 was considered to be statistically significant.
Results
Literature search
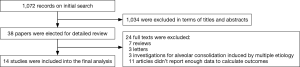
A flow chart of the trial selection process was shown in Figure 1. We initially identified 1,072 studies by title and abstract screening according to our search strategy. However, 1,034 were excluded as they were seldom relevant to our analysis, leaving 38 articles for further estimation. After evaluating the full texts of these potentially relevant studies, we excluded two studies about LUS examinations on radiologically confirmed pneumonia as the control group was missing (patients who were clinically suspected with pneumonia but were finally excluded by the gold standard) (29,30), and three studies investigating the diagnostic efficiency of LUS for alveolar consolidation induced by multiple etiology, such as pulmonary embolism, acute respiratory distress syndrome (ARDS), multiple trauma, pneumothorax, lung cancer and others (31-33). Eventually, 14 eligible studies involving a total of 1,911 patients were included into the final analysis.
Characteristics of selected studies
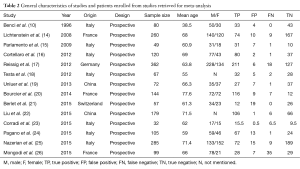
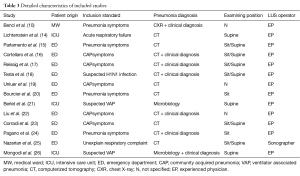
Among all 14 studies, 11 were carried out in emergency department (ED) or medical wards (10,15-20,22-25), and 3 were conducted in intensive care unit (ICU) (14,21,26). Hemithorax was used as the study unit for result interpretation in one study (23), while others counted by patient. To overcome this challenge and maintain study weight estimates intact, we divided the data from this study by 2. The main characteristics of selected studies were shown in Table 2. Briefly, all studies were prospective and blinded design. Twelve were performed in Europe and 2 in China. The mean age of enrolled patients was 66-year-old with approximate 57% male. For the gold standard of pneumonia diagnosis, six set chest CT as the sole criteria, six used clinical presentations together with imaging, and two studies introduced microbiology. Additionally, LUS was performed by experienced physicians in ED or ICU except one study whose ultrasound procedures were done by sonographers (25). Of note, lateral and posterior chest wall examinations were both conducted preferably in the seated position in three studies (20,24,25), while six performed posterior scan in supine or semi-recumbent position, and lateral examination in a sitting position; three studies in ICU used supine or semi-recumbent position for all scans (14,21); two studies did not specify the position (10,22) (Table 3). The details of the quality assessment were shown in Table 1. The eligible studies achieved most of the quality items in QUADAS-2.
Full table
Full table
Statistical outcomes
Overall diagnostic accuracy
Figures 2 showed the pooled sensitivity, specificity, DOR, positive likelihood rate (PLR), negative likelihood rate (NLR) and the summary receiver operative characteristics (sROC) curves for diagnostic efficiency of LUS on pneumonia. Overall pooled sensitivity and specificity for the diagnosis of pneumonia were 90.4% (95% CI, 88.4% to 92.1%; P<0.001) and 88.4% (95% CI, 86.1% to 90.4%; P<0.001), respectively. Overall pooled PLR and NLR were 6.6 (95% CI, 3.7 to 11.7; Cochran Q-statistic =135.32; P<0.001) and 0.08 (95% CI, 0.04 to 0.19; Cochran Q-statistic =196.87, P<0.001), respectively. In addition, sROC area under the curve (AUC) was 0.9611.
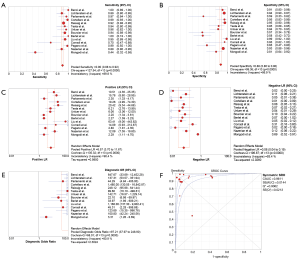
The Spearman correlation coefficient between the log of sensitivity and 1-specificity was 0.222 (P=0.445) for LUS, suggesting that the causes of variations existed other than threshold effect. In extension, we performed the subgroup analysis.
Subgroup analysis by LUS performance
We first analyzed the accuracy of ultrasonography on detecting pneumonia at different medical wards. In studies conducted in ED (n=10), the pooled sensitivity was 93.5% (95% CI, 91.6% to 95.1%), and a pooled specificity was 89.2% (95% CI, 86.4% to 91.5%). In studies that evaluated critically-ill patients in the ICU (n=3), the pooled sensitivity was 72.2% (95% CI, 64.5% to 79.0%), and a pooled specificity was 86.0% (95% CI, 81.2% to 90.0%). Secondly, studies (n=2) that used seated position when LUS performed showed the pooled sensitivity of 95.8% (95% CI, 91.9% to 98.2%) and a pooled specificity of 62.1% (95% CI, 48.4% to 74.5%). However, studies (n=3) that used supine or semi-recumbent position when LUS performed showed the pooled sensitivity of 72.2% (95% CI, 64.5% to 79.0%), and a pooled specificity was 86.0% (95% CI, 81.2% to 90.0%). In studies (n=6) that performed posterior scan in supine or semi-recumbent position, followed by lateral scan in a sitting position, LUS had a pooled sensitivity of 92.2% (95% CI, 89.4% to 94.4%) and a pooled specificity of 91.9% (95% CI, 88.9% to 94.2%).
Subgroup analysis by diagnosing strategy and study origin
In six studies that used chest CT as the sole criteria, LUS exhibited a pooled sensitivity of 90.9% (95% CI, 87.5% to 93.6%) and a pooled specificity of 89.7% (95% CI, 86.7% to 92.3%). In studies (n=6) that employed the combination of chest imaging and clinical criteria as the gold-standard, LUS revealed a pooled sensitivity of 95.0% (95% CI, 92.8% to 96.6%) and a pooled specificity of 91.3% (95% CI, 87.9% to 94.0%). In studies (n=2) that focused on VAP confirmed by microbiology, LUS showed a sensitivity of 53.3% (95% CI, 41.4% to 64.9%) and specificity of 67.9% (95% CI, 56.6% to 77.8%). In studies carried out in Europe, LUS had a pooled sensitivity of 89.6% (95% CI, 87.4% to 91.6%) and a pooled specificity of 87.8% (95% CI, 85.3% to 90.0%). In studies conducted in China, LUS contributed to a pooled sensitivity of 95.0% (95% CI, 90.0% to 98.0%) and a pooled specificity of 92.8% (95% CI, 86.3% to 96.8%).
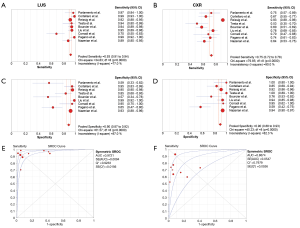
LUS verses CXR for the diagnosis of pneumonia
Of all involved studies, we collected the data from nine studies which supplied sufficient information to compare the diagnostic efficiency of LUS against CRX (Figure 3). This subset included 1,343 subjects, consisting of 782 pneumonias and 561 controls. The calculated pooled sensitivity for LUS and CXR was 92.8% and 75.1% with pooled specificity of 89.7% and 90.5%, respectively. The CXR and LUS modalities could be judged by AUC. We compared the two sROC curves by Z statistic. The AUC for LUS and CR were 0.9721 (SE, 0.0094) and 0.8674 (SE, 0.0547), Z statistic of two sROC curves was 2.31 (P<0.05).
Analysis of publication bias
Funnel plot and Egger’s regression asymmetry test were conducted to appraise the publication bias. Distribution of data points failed to illustrate any hint of apparent asymmetry. In concert, the negative result was further confirmed by Egger’s linear regression asymmetry test.
Discussion
Ultrasonography has been well-recognized as a valuable bedside tool of diagnosing pulmonary diseases, providing a user-friendly, inexpensive, noninvasive, and reliable examination. Here, we found that the diagnostic efficiency of LUS for pneumonia in adult was well-satisfied, with the pooled sensitivity of 90.4% and specific of 88.4%. PLR indicated that patients with pneumonia presented 6.6 times higher possibility to appear abnormal LUS results compared to the ones without pneumonia. NLR in line suggested the probability of pneumonia presenting normal LUS reading was as low as 8%. Subgroup analysis indicated that the sensitivity of LUS derived from ICU was lower than that of ED. It could be attributed to most of the pneumonia diagnosed in ED is CAP and in ICU is HAP and VAP. The etiology of the latter is much more complicated and the clinical presentations are usually atypical. Interestingly, combination of supine or semi-recumbent position with sitting position during LUS performance resulted in a potent diagnosis power. This is supposed to be recommended as the standard procedure in all patients if available. The results of the trails conducted in Europe were similar to the data in China, suggesting the diagnosis accuracy is solid and might not be affected by race and region, only if the physicians were well-trained. Once again, our results confirmed LUS was a more powerful tool of rapid pneumonia detection than CXR.
To date, three meta-analyses have summarized the data concerning LUS and pneumonia (4,11,34). In the analysis by Hu and colleagues (34), they studied the patients with pneumonia of all ages. Notably, not only pathogen, clinical presentations and prognosis, but the reference standards are dramatically different between children and adults. It is more reasonable to analyze two sets of patients separately. In the study by Chavez et al. (4), they focused on the adult patients with pneumonia. However, Berlet stated that certain studies (3 out of 10) recruited in their analysis investigated the diagnostic accuracy of LUS for alveolar consolidation of any etiology, including sepsis, ARDS and MODS, which might distract the estimating precision (35). Moreover, at least nine new studies have been published since their meta-analysis conducted. Here, we assessed the quality of recent published nine papers, and 7 of them eventually passed the inclusion criteria and were taken into calculation. We also eliminated the three previous studies for unspecific diagnosis. The analysis by Ye et al. (11) was designed to compare LUS and CXR for pneumonia diagnosis. Their conclusion was consistent with our analysis, but we included additional studies to strengthen the evidence power. We believe that our analysis adds more objective insights to support the applications of LUS for the diagnosis of pneumonia in different clinical settings.
Thoracic CT scan is considered as the gold standard for diagnosis of pneumonia. This technique, however, is unlikely to be always served as the first line due to the radioactive exposure and high cost, especially in critically-ill patients whose conditions usually change sharply and require repeated examinations to guide the interventions. Our analysis confirmed the precise diagnostic accuracy of LUS on the detection of pneumonia. The following four signs are the major abnormalities linking to pneumonia under LUS: interstitial syndrome; abnormal pleural line; alveolar consolidation and pleural effusion. Liu et al. compared different combinations of LUS patterns and found that combining four ultrasonographic signs led to the highest sensitivity (94.6%) for diagnosing CAP (22). Considering it is a bedside, reliable, rapid and noninvasive technique, LUS plays a critical role in the diagnostic work up of pneumonia in ICU and in patients from ED where usually asks for immediate decisions.
Execution rapidity, non-invasivity and low cost make LUS a striking approach of evaluating pneumonia on different types of patients. Also, experienced physicians in 13 studies verses sonographers in only one study performed the LUS and they achieved identical results, implying the learning curve of LUS is not steep. However, the training time was extremely varied, ranging from several hours’ course to ten years’ clinical practice. Besides, it is noteworthy to highlight the situations that related to false positive and false negative results. The specificity derived from our analysis was lower than previous studies, which was partly caused by the false-positive conditions on LUS: pleural adhesions, bullous emphysema, fluid bronchogram, past interstitial pathology, neoplasia, pulmonary infarction, sepsis of other origins, main-stem intubation on the contralateral side (17,18,20,24). By contrast, the false negative results usually occurred when the consolidation was located far away from pleura and hided deep in the lung parenchyma. In addition, quantitative LUS (QLUS) was evident to be an impressive approach of pneumonia detection, showing a higher sensitivity and specificity than regular LUS (23). The combination of LUS and microbiological gram stain caused a conclusive increase in the likelihood of pneumonia diagnosis (26).
There are some limitations to our analysis. We did not include articles in languages other than English, and did not try to identify studies that haven’t published in peer reviewed journals; the total number of studies was small and most studies included in our analysis did not have large sample size; there was significant heterogeneity among studies; most were single center studies and were conducted in settings from high-income countries. Despite all of these limitations, this meta-analysis included 1,911 participants and provided promising evidence for the utilization of this diagnostic technique and for the initiation of training programs geared to teach physicians this diagnostic tool.
In conclusion, based on current available evidence, LUS is a valid alternative for the diagnosing pneumonia in adults. This is just a start, a beginning of a new trend and a convenient bedside tool for diagnosis of a common health problem.
Acknowledgements
Funding: This work was supported by Zhejiang Provincial Natural Science Foundation of China (LQ16H010001), National Natural Science Foundation of China (81500012), Medical and Health Technology Program of Zhejiang Province (2015KYB165) to Dr. Y Xia.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Wunderink RG, Waterer GW. Clinical practice. Community-acquired pneumonia. N Engl J Med 2014;370:543-51. [Crossref] [PubMed]
- Eccles S, Pincus C, Higgins B, et al. Diagnosis and management of community and hospital acquired pneumonia in adults: summary of NICE guidance. BMJ 2014;349:g6722. [Crossref] [PubMed]
- American Thoracic Society; Infectious Diseases Society of America. Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 2005;171:388-416. [Crossref] [PubMed]
- Chavez MA, Shams N, Ellington LE, et al. Lung ultrasound for the diagnosis of pneumonia in adults: a systematic review and meta-analysis. Respir Res 2014;15:50. [Crossref] [PubMed]
- Claessens YE, Debray MP, Tubach F, et al. Early Chest Computed Tomography Scan to Assist Diagnosis and Guide Treatment Decision for Suspected Community-acquired Pneumonia. Am J Respir Crit Care Med 2015;192:974-82. [Crossref] [PubMed]
- Ding W, Shen Y, Yang J, et al. Diagnosis of pneumothorax by radiography and ultrasonography: a meta-analysis. Chest 2011;140:859-66. [Crossref] [PubMed]
- Prina E, Ranzani OT, Torres A. Community-acquired pneumonia. Lancet 2015;386:1097-108. [Crossref] [PubMed]
- Xia Y, Ma Y, Arias S, et al. Utilization of the International Association for the Study of Lung Cancer and Wang's nodal map for the identification of mediastinum and hilar lymph nodes. Thorac Cancer 2015;6:464-8. [Crossref] [PubMed]
- Xia Y, Zhang B, Zhang H, et al. Evaluation of lymph node metastasis in lung cancer: who is the chief justice? J Thorac Dis 2015;7:S231-7. [PubMed]
- Benci A, Caremani M, Menchetti D, et al. Sonographic diagnosis of pneumonia and bronchopneumonia. Eur J Ultrasound 1996;4:169-76. [Crossref]
- Ye X, Xiao H, Chen B, et al. Accuracy of Lung Ultrasonography versus Chest Radiography for the Diagnosis of Adult Community-Acquired Pneumonia: Review of the Literature and Meta-Analysis. PLoS One 2015;10:e0130066. [Crossref] [PubMed]
- Kalil AC, Metersky ML, Klompas M, et al. Management of Adults With Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis 2016;63:e61-e111. [Crossref] [PubMed]
- Whiting PF, Rutjes AW, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529-36. [Crossref] [PubMed]
- Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest 2008;134:117-25. [Crossref] [PubMed]
- Parlamento S, Copetti R, Di Bartolomeo S. Evaluation of lung ultrasound for the diagnosis of pneumonia in the ED. Am J Emerg Med 2009;27:379-84. [Crossref] [PubMed]
- Cortellaro F, Colombo S, Coen D, et al. Lung ultrasound is an accurate diagnostic tool for the diagnosis of pneumonia in the emergency department. Emerg Med J 2012;29:19-23. [Crossref] [PubMed]
- Reissig A, Copetti R, Mathis G, et al. Lung ultrasound in the diagnosis and follow-up of community-acquired pneumonia: a prospective, multicenter, diagnostic accuracy study. Chest 2012;142:965-72. [Crossref] [PubMed]
- Testa A, Soldati G, Copetti R, et al. Early recognition of the 2009 pandemic influenza A (H1N1) pneumonia by chest ultrasound. Crit Care 2012;16:R30. [Crossref] [PubMed]
- Unluer E, Karagoz A, Senturk G, et al. Bedside lung ultrasonography for diagnosis of pneumonia. Hong Kong Am J Emerg Med 2013;20:98.
- Bourcier JE, Paquet J, Seinger M, et al. Performance comparison of lung ultrasound and chest x-ray for the diagnosis of pneumonia in the ED. Am J Emerg Med 2014;32:115-8. [Crossref] [PubMed]
- Berlet T, Etter R, Fehr T, et al. Sonographic patterns of lung consolidation in mechanically ventilated patients with and without ventilator-associated pneumonia: a prospective cohort study. J Crit Care 2015;30:327-33. [Crossref] [PubMed]
- Liu XL, Lian R, Tao YK, et al. Lung ultrasonography: an effective way to diagnose community-acquired pneumonia. Emerg Med J 2015;32:433-8. [Crossref] [PubMed]
- Corradi F, Brusasco C, Garlaschi A, et al. Quantitative analysis of lung ultrasonography for the detection of community-acquired pneumonia: a pilot study. Biomed Res Int 2015;2015:868707.
- Pagano A, Numis FG, Visone G, et al. Lung ultrasound for diagnosis of pneumonia in emergency department. Intern Emerg Med 2015;10:851-4. [Crossref] [PubMed]
- Nazerian P, Volpicelli G, Vanni S, et al. Accuracy of lung ultrasound for the diagnosis of consolidations when compared to chest computed tomography. Am J Emerg Med 2015;33:620-5. [Crossref] [PubMed]
- Mongodi S, Via G, Girard M, et al. Lung Ultrasound for Early Diagnosis of Ventilator-Associated Pneumonia. Chest 2016;149:969-80. [Crossref] [PubMed]
- DerSimonian R, Kacker R. Random-effects model for meta-analysis of clinical trials: an update. Contemp Clin Trials 2007;28:105-14. [Crossref] [PubMed]
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [Crossref] [PubMed]
- El Sheikh H, Rabboh MM. Chest ultrasound in the evaluation of complicated pneumonia in the ICU patients: Can be viable alternative to CT? The Egyptian Journal of Radiology and Nuclear Medicine 2014;45:325-31. [Crossref]
- Alkhayat KF, Alam-Eldeen MH. Value of chest ultrasound in diagnosis of community acquired pneumonia. Egyptian Journal of Chest Diseases and Tuberculosis 2014;63:1047-51. [Crossref]
- Lichtenstein D, Goldstein I, Mourgeon E, et al. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology 2004;100:9-15. [Crossref] [PubMed]
- Lichtenstein DA, Lascols N, Mezière G, et al. Ultrasound diagnosis of alveolar consolidation in the critically ill. Intensive Care Med 2004;30:276-81. [Crossref] [PubMed]
- Xirouchaki N, Magkanas E, Vaporidi K, et al. Lung ultrasound in critically ill patients: comparison with bedside chest radiography. Intensive Care Med 2011;37:1488-93. [Crossref] [PubMed]
- Hu QJ, Shen YC, Jia LQ, et al. Diagnostic performance of lung ultrasound in the diagnosis of pneumonia: a bivariate meta-analysis. Int J Clin Exp Med 2014;7:115-21. [PubMed]
- Berlet T. Thoracic ultrasound for the diagnosis of pneumonia in adults: a meta-analysis. Respir Res 2015;16:89. [Crossref] [PubMed]