Coronary bifurcation lesions: is less more?
Coronary bifurcation lesions are frequent in everyday practise and account for up to 20% of all percutaneous coronary interventions (PCI) (1). The treatment of bifurcation lesions with drug-eluting stents (DES), especially when a double stent technique is used, remains challenging and is associated with a lower procedural success rate and a higher rate of long-term adverse cardiac events such as stent restenosis and thrombosis compared to non-bifurcation PCI (2). The question relating to a one or two stent strategy for bifurcation lesions has been a subject of many debates over recent years and numerous observational and randomized studies (3-6) have supplied data to this important though at times controversial subject.
Recently, Behan et al. (7) presented the 5-year outcome data from a patient-level pooled analysis of coronary bifurcation lesions treated with simple or complex stenting in two pivotal studies (7): more specifically, pooled 5-year results of the NORDIC 1 (8) and the British Bifurcation Coronary Study: Old, New, and Evolving Strategies (BBC ONE) (4), both of similar magnitude and methodology (N=413 and 500, respectively), that compared all-cause mortality and other clinical endpoints after simple single-stent (provisional T stenting) versus complex two-stent (culotte, crush and T-stenting) techniques, using DES.
Before looking at the results in more detail it is important to note that differences in bifurcation anatomy and disease severity are major determinants of treatment approach and remain at the discretion and judgement of the single operator. Several valuable bifurcation classifications have been proposed (9-11), none of them fully encompassing variations in anatomy, including vessel size, bifurcation angle and extent of disease in the side branch. From a practical point of view, the operator is generally speaking faced with one of two situations: in the first scenario, due to the severity of the disease at the bifurcation and extending in to large calibre branches, two stents are required from the outset. This type has typically not been represented (thus giving rise to selection bias) in the randomized studies to date comparing different strategies as operators are not willing to risk randomising these patients to a single-stent strategy. The second type of bifurcation lesion is where one or two stents can be used. For these bifurcation lesions, multiple randomized studies comparing a routine two-stent strategy with a provisional strategy (single stent in the main vessel with additional side branch stent only if indicated) have shown comparable efficacy outcomes (target vessel/target lesion revascularization rates) between the two treatment strategies, although the provisional strategy resulted in lower rates of peri-procedural myocardial infarction (MI), less contrast use, lower X-ray doses and shorter procedural times (3,4,6). There is therefore, for this second type of lesion, a general consensus that it is better to Keep It as Simple and Safe as possible and implant one stent (KISS provisional strategy) and crossover to two stents only if required (12). Further evidence supporting this consensus statement is provided by the recent analysis by Behan et al. of the 5-year clinical outcomes up of the NORDIC 1 and BBC ONE bifurcation studies.
Both these multicenter randomized trials compared simple single-stent (provisional T stenting) versus complex two-stent (culotte, crush and T-stenting) techniques, using DESs. Although there were several differences in terms of trial design, mainly in the criteria for crossover from one-stent to two stent strategy and planned angiographic follow up, overall there were many similarities between the two studies with similar complex bifurcation techniques and similar endpoints being assessed. There are several limitations to the studies as pointed out by the authors and by Colombo and Jabbour (13): (I) both studies were performed with 1st generation DES which have been shown to be inferior to current generation DES, either with regard to the risk for death, MI or repeat revascularization, and/or with regard to stent thrombosis (14-16). Especially the usage of the paclitaxel-eluting stent (Taxus, Boston Scientific Corp, Natick, MA, USA) in the BBC ONE study is a major limitation given the higher rate of stent thrombosis compared with other 1st generation DES (17,18); (II) the techniques employed in the complex bifurcation techniques were suboptimal with the recommended kissing balloon post-dilatation only being performed in ±75% of cases; whilst there is no data regarding the performance of the proximal optimization technique; (III) approximately 28% of lesions were not true bifurcation lesions and therefore not appropriate for a two-stent strategy according to current practice; (IV) dual antiplatelet therapy (DAPT) was only mandated for a minimum of 6 months in the NORDIC patients and 9 months in the BBC ONE patients though there is no data on actual length of DAPT. Furthermore, newer antiplatelet agents would now be considered, especially in the 1/3 of patients who presented with an acute coronary syndrome or not responding to clopidogrel; (V) finally, all-cause mortality was presented rather than cardiac death which only allows one to postulate that the excess deaths in one of the groups were due to associated cardiac events.
The authors of the current analysis were able to collect 5-year follow-up data in 97% of patients. Both simple and complex groups were similar in terms of patient and lesion characteristics. The rate of side branch stenting in the provisional group was similarly low in the Nordic 1 and BBC ONE studies (4.3% vs. 3%, P=0.33). The 5-year mortality rates were reassuringly low in both the simple and complex groups. Interestingly, the overall mortality rate appears to be almost twice as high in the NORDIC I study compared to the BBC ONE study despite the fact that the NORDIC I study employed the superior sirolimus-eluting stent (Cypher, Cordis, Johnson and Johnson, Bridgewater, NJ, USA). The main finding of this analysis is that 5-year mortality was lower among patients who underwent a simple strategy rather than a complex strategy [17 patients (3.8%) vs. 31 patients (7.0%); P=0.04]. Interestingly, the Kaplan-Meyer curves appear to separate after 2 years suggesting that the complex strategy yields elevated risk of events beyond the time at which technical procedure-related factors play a role. The authors suggest that the higher mortality rates following complex strategies may be due to a higher incidence of very late stent thrombosis. Although there is data supporting the theory that a double stent strategy may increase the risk of stent thrombosis (2), this study can only postulate that there may be excess death in the complex group given the important limitation that the investigators only reported all-cause mortality and not cardiovascular death. Furthermore, as Colombo and Jabbour rightly point out, a “play of chance” cannot be ruled out.
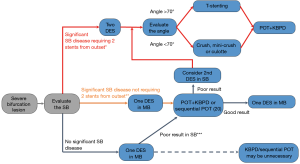
Nevertheless, this study adds further weight to the case that a provisional stent strategy should be used as the default approach for the treatment of coronary bifurcation lesions when there is a possibility of using one stent from the outset. It of course remains a challenge to distinguish the more complex bifurcation lesions which are likely to require complex stenting procedures with multiple stents or dedicated bifurcation stents (19) from the more “simple” bifurcation lesions which are likely to be adequately treated with the provisional strategy. A proposed contemporary approach to the treatment of severe bifurcation lesion is summarized in Figure 1. Use of contemporary DES, optimal stenting techniques, and newer antiplatelet agents will further improve the clinical outcomes by reducing the incidence of long-term adverse cardiac events such as stent restenosis and thrombosis.
Acknowledgements
None.
Footnote
Provenance: This is an invited Editorial commissioned by the Section Editor Feng Zhang (Department of Cardiology, Zhongshan Hospital of Fudan University, Shanghai, China).
Conflicts of Interest: Johan Bennett is holder of a research grant from Abbott Vascular and Biotronik. Christophe Dubois is holder of a research grant from Abbott Vascular and Boston Scientific.
References
- Collins N, Seidelin PH, Daly P, et al. Long-term outcomes after percutaneous coronary intervention of bifurcation narrowings. Am J Cardiol 2008;102:404-10. [Crossref] [PubMed]
- Iakovou I, Schmidt T, Bonizzoni E, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA 2005;293:2126-30. [Crossref] [PubMed]
- Colombo A, Bramucci E, Saccà S, et al. Randomized study of the crush technique versus provisional side-branch stenting in true coronary bifurcations: the CACTUS (Coronary Bifurcations: Application of the Crushing Technique Using Sirolimus-Eluting Stents) Study. Circulation 2009;119:71-8. [Crossref] [PubMed]
- Hildick-Smith D, de Belder AJ, Cooter N, et al. Randomized trial of simple versus complex drug-eluting stenting for bifurcation lesions: the British Bifurcation Coronary Study: old, new, and evolving strategies. Circulation 2010;121:1235-43. [Crossref] [PubMed]
- Chen SL, Santoso T, Zhang JJ, et al. A randomized clinical study comparing double kissing crush with provisional stenting for treatment of coronary bifurcation lesions: results from the DKCRUSH-II (Double Kissing Crush versus Provisional Stenting Technique for Treatment of Coronary Bifurcation Lesions) trial. J Am Coll Cardiol 2011;57:914-20. [Crossref] [PubMed]
- Maeng M, Holm NR, Erglis A, et al. Long-term results after simple versus complex stenting of coronary artery bifurcation lesions: Nordic Bifurcation Study 5-year follow-up results. J Am Coll Cardiol 2013;62:30-4. [Crossref] [PubMed]
- Behan MW, Holm NR, de Belder AJ, et al. Coronary bifurcation lesions treated with simple or complex stenting: 5-year survival from patient-level pooled analysis of the Nordic Bifurcation Study and the British Bifurcation Coronary Study. Eur Heart J 2016;37:1923-8. [Crossref] [PubMed]
- Steigen TK, Maeng M, Wiseth R, et al. Randomized study on simple versus complex stenting of coronary artery bifurcation lesions: the Nordic bifurcation study. Circulation 2006;114:1955-61. [Crossref] [PubMed]
- Medina A, Suárez de Lezo J, Pan M. A new classification of coronary bifurcation lesions. Rev Esp Cardiol 2006;59:183. [Crossref] [PubMed]
- Movahed MR. Major limitations of randomized clinical trials involving coronary artery bifurcation interventions: time for redesigning clinical trials by involving only true bifurcation lesions and using appropriate bifurcation classification. J Interv Cardiol 2011;24:295-301. [Crossref] [PubMed]
- Y-Hassan S. Lindroos MC, Sylvén C. A Novel Descriptive, Intelligible and Ordered (DINO) classification of coronary bifurcation lesions. Review of current classifications. Circ J 2011;75:299-305. [Crossref] [PubMed]
- Lassen JF, Holm NR, Banning A, et al. Percutaneous coronary intervention for coronary bifurcation disease: 11th consensus document from the European Bifurcation Club. EuroIntervention 2016;12:38-46. [Crossref] [PubMed]
- Colombo A, Jabbour RJ. Bifurcation lesions: no need to implant two stents when one is sufficient! Eur Heart J 2016;37:1929-31. [Crossref] [PubMed]
- Kedhi E, Joesoef KS, McFadden E, et al. Second-generation everolimus-eluting and paclitaxel-eluting stents in real-life practice (COMPARE): a randomised trial. Lancet 2010;375:201-9. [Crossref] [PubMed]
- Jensen LO, Thayssen P, Hansen HS, et al. Randomized comparison of everolimus-eluting and sirolimus-eluting stents in patients treated with percutaneous coronary intervention: the Scandinavian Organization for Randomized Trials with Clinical Outcome IV (SORT OUT IV). Circulation 2012;125:1246-55. [Crossref] [PubMed]
- Camenzind E, Wijns W, Mauri L, et al. Stent thrombosis and major clinical events at 3 years after zotarolimus-eluting or sirolimus-eluting coronary stent implantation: a randomised, multicentre, open-label, controlled trial. Lancet 2012;380:1396-405. [Crossref] [PubMed]
- Chen S, Zhang J, Ye F, et al. Crush stenting with paclitaxel-eluting or sirolimus-eluting stents for the treatment of coronary bifurcation lesions. Angiology 2008;59:475-83. [Crossref] [PubMed]
- Pan M, Suárez de Lezo J, Medina A, et al. Drug-eluting stents for the treatment of bifurcation lesions: a randomized comparison between paclitaxel and sirolimus stents. Am Heart J 2007;153:15.e1-7. [Crossref] [PubMed]
- Dubois C, Bennett J, Dens J, et al. COmplex coronary Bifurcation lesions: RAndomized comparison of a strategy using a dedicated self-expanding biolimus-eluting stent versus a culotte strategy using everolimus-eluting stents: primary results of the COBRA trial. EuroIntervention 2016;11:1457-67. [Crossref] [PubMed]
- Finet G, Derimay F, Motreff P, et al. Comparative Analysis of Sequential Proximal Optimizing Technique Versus Kissing Balloon Inflation Technique in Provisional Bifurcation Stenting: Fractal Coronary Bifurcation Bench Test. JACC Cardiovasc Interv 2015;8:1308-17. [Crossref] [PubMed]


