Recurrent laryngeal nerve lymph node dissection may not be suitable for all early stage esophageal squamous cell carcinoma patients: an 8-year experience
Introduction
Esophageal carcinoma is the sixth leading cause of cancer-related mortality and the eighth most common cancer worldwide, for which the 5-year survival rate is only 15–25% (1,2). Almost half of the total reported cases have occurred in China, which also has the highest mortality rate (2). Thus far, radical resection remains an important therapy for resectable esophageal squamous cell carcinoma (ESCC). Lymph node dissection plays an important role in esophageal cancer radical resection (3,4). Lymph node metastasis ratios and lymph node metastasis rates are independent risk factors for ESCC prognosis (5,6). The recurrent laryngeal nerve lymph node (RLNLN) is the most common metastatic site in ESCC, and the rates of RLNLN metastases in upper thoracic ESCC are even as high as 43.3% (7,8). The RLNLN metastases are considered as independent predictors of cervical lymph node metastases (LNM) (9-11). In addition, some scholars believe that regular RLNLN dissection is necessary for accurate staging and radical resection, particularly for middle and upper thoracic esophageal carcinomas (12). Therefore, RLNLN dissection is of great significance for ESCC radical resection.
However, RLNLN dissection has increased the rates of postoperative complications. Recurrent laryngeal nerve (RLN) injury is one of the most frequent postoperative complications of ESCC radical resection, with an incidence of 3.5–24% (13-15). National Comprehensive Cancer Network guidelines (Version 2.2013) recommend that the total number of lymph nodes dissected should be greater than 15 to determine accurate staging, but it does not explicitly recommend for regular RLNLN dissection. Left-sided RLN paralysis is encountered more frequently than right-sided paralysis, commonly attributed to the longer length of the RLN on the left side providing more opportunities for injury (16). Injury may generate hoarseness and breathy voice. The patient’s cough is weak and pulmonary complications, including aspiration, may occur (17). Hence, surgical complications may be reduced for ESCC patients if unnecessary lymph node dissection is reduced.
Thus far, there is no scoring system that can predict RLNLN metastases. Therefore, our objective was to devise a simple flexible scoring system to accurately predict RLNLN metastases in patients with early stage ESCC using statistical methods. Furthermore, we explored the indications for selective RLNLN dissection in early stage ESCC patients from three aspects: survival rate, postoperative complications and RLNLN metastases rate.
Methods
Study population
In this retrospective study, a total of 1,466 patients underwent resection for esophageal carcinoma at the Affiliated Union Hospital of Fujian Medical University between January 2006 and December 2014. The postoperative pathological diagnoses of all the patients included were ESCC. All the patients underwent preoperative examinations to exclude undetected metastatic lesions and enlarged lymph nodes by chest and abdomen computed tomography (CT), barium esophagography, electronic gastroscopy, cervical and abdomen ultrasound, and endoscopic ultrasound, or whole-body positron emission tomography CT (PET-CT). Because of the high price for patients, PET-CT hasn’t been routinely performed to evaluate nodal metastases and distant metastases. In addition, the postoperative pathological T stage of the patient tumors included was T1–2. Excluding patients according to the following criteria: (I) patients who received preoperative chemoradiotherapy or patients whose esophageal cancer pathological characteristics were not ESCC; (II) patients without the extent of lymph node dissection records and patients with definite distant metastasis; (III) patients with cervical ESCC and patients with clinically node positive; (IV) patients with hoarseness. According to the above conditions, 311 patients with thoracic ESCC were selected for this study, including 204 patients who underwent esophagectomy with common bilateral RLNLN dissection which constituted the dissection group and 107 patients who underwent esophagectomy without common RLNLN dissection which constituted the control group. The Institutional Review Board of the Affiliated Union Hospital of Fujian Medical University approved this study (No. 2016KY022) and granted a waiver of the informed consent process.
Risk factors
Age, sex, the time of swallowing dysfunction, smoking history, carcinoembryonic antigen (CEA), cyfra21-1, history of other tumor, macroscopic tumor type, T stage, tumor differentiation, lymphovascular invasion (LVI), tumor length and tumor location were chosen as potential factors predictive of RLNLN metastases in ESCC patients who underwent thoracic esophagectomy with common bilateral RLNLN dissection based on previous studies of risk factors for esophageal cancer LNM (11,18,19). Staging was performed as per the American Joint Committee on Cancer 7th edition TNM staging system for ESCC. The age, sex, smoking history, the time of swallowing dysfunction, history of other tumor, cyfra21-1 and CEA of patients were collected from medical records, and the T stage, tumor differentiation and LVI were obtained from final surgical pathology reports. The last time that patient difficulty ate solid food was defined as the time of swallowing dysfunction before the operation. According to Japanese Classification of Esophageal Cancer (10th), macroscopic tumor type was divided into superficial type and advanced type by radiological and endoscopic findings (20). The tumor length was defined as the largest measurement in any dimension measured preoperatively by endoscopy and CT. Tumor location was determined by the upper pole of tumor [(I) upper thoracic esophagus: from the sternal notch to the tracheal bifurcation; (II) middle thoracic esophagus: the proximal half of the two equal portions between the tracheal bifurcation and the esophagogastric junction; (III) lower thoracic esophagus: the thoracic part of the distal half of the two equal portions between the tracheal bifurcation and the esophagogastric junction]. LNM was defined as pathologic lymph node involvement upon hematoxylin and eosin staining of the final surgical specimen. LVI was defined as the presence of neoplastic cells within peritumoral lymphovascular structures (i.e., this definition does not include true LNM). Patient and operative characteristics were collected from medical records, and all pathologic characteristics were obtained from the final pathology reports completed by two professional pathologists. All clinical information about variables potentially predicting RLNLN metastases were from original records. Finally, 204 patients, who underwent RLN LN dissection, were divided into those with RLNLN metastases upon final pathology and those without.
Postoperative complications
Postoperative complications of RLN injury were confirmed with the following tests. A regular fiberoptic bronchoscopy or laryngoscope was conducted in the 2nd and 4th postoperative weeks. RLN injury was determined by the dysmotility of the vocal cords. When postoperative fevers were higher than 38.5 degrees Celsius, pneumonia was indicated by conventional chest X-ray or CT, and bacterial infection was identified by sputum culture. Pleural effusion was determined by chest X-ray or CT. Anastomotic fistula was diagnosed by esophagography with 76% meglumine diatrizoate.
Postoperative follow-up
Follow-up by telephone or outpatient service after discharge was conducted by a professional thoracic surgery doctor. After operation, patients were reviewed every 3 months in the first 2 years, every half-year in years 2–5 and every year after 5 years. The exams reviewed included serum tumor markers (such as CEA, cyfra21-1), thoracic CT, abdominal ultrasonography or CT and whole-body radionuclide bone scanning. Gastroscopy should be added if dysphagia occurs. Follow-up data were recorded until June 2015 or death. Follow-up results were classified as death, survival or withdraw. The loss rate for follow-up was 12.2% (38/311). The date of death was confirmed with the register of the Department of Civil Affairs of China even for patients who were lost during clinical follow-up. Four courses of paclitaxel plus cisplatin was administered postoperatively in patients with positive lymph node metastasis
Statistics
In the dissection group, the relationship between RLNLN metastases in ESCC and metastases-related variables was compared by univariate analysis, which could filter out variables with statistically significant differences (P<0.05). Stepwise multivariate logistic regression was used to develop a model for predicting RLNLN metastases (the dependent variable was RLNLN metastases). This logistic model was evaluated by the Hosmer-Lemeshow goodness of fit test and a receiver operating characteristic (ROC) curve by comparing risk factors for RLNLN metastases with the results observed. Finally, a novel multivariate scoring system was developed based on beta coefficients from a confounding factors binary logistic model.
A total of 204 patients were divided into high-, moderate- and low-risk subgroups using the multivariate scoring system. Subsequently, we explored the necessity of RLNLN dissection by comparing the survival rate and postoperative complications between the dissection group and the control group. The RLNLN metastases rates among high-, moderate- and low-risk subgroups were also considered as an evidence for selective RLNLN dissection. All statistical analyses were performed using SPSS 19.0 software.
Results
A total of 311 patients who underwent thoracic esophagectomy were included for analysis. In this study, the patients were divided into the dissection group (n=204) and the control group (n=107). The baseline characteristics of the patients are listed in Table 1 with no missing values. All variables of two groups were comparable, as there were no statistically significant differences. There were 148 males (72.55%) and 56 females (27.45%) in the dissection group and 79 males (73.83%) and 28 females (26.17%) in the control group. Besides, the average ages of the dissection group and the control group were 57.60 and 57.50 years old, respectively. The number of male patients of the dissection group and the control group were 148 and 71, respectively. The overall incidence of RLNLN metastases was 14.22% (29/204) in the dissection group. According to the maximum Youden index, the optimal critical value of age was 56 years and tumor length 4.45 cm for estimating RLNLN metastases in the dissection group.
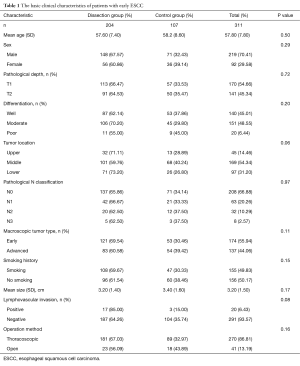
Full table
Univariate analysis
According to univariate analysis, age (P<0.01), tumor length (P<0.01), tumor location (P<0.01), macroscopic tumor type (P<0.01), T stage (P<0.01), tumor differentiation (P=0.02) were statistically significant differences. RLNLN metastases were more inclined to occur in the condition of upper thoracic tumors, age (<56 years), tumor length (>4.45 cm), advanced macroscopic tumor type, T2 and poor tumor differentiation (Table 2).
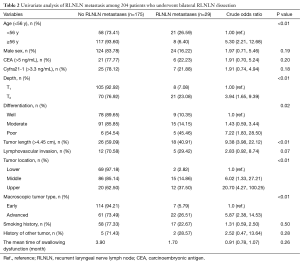
Full table
Multivariate analysis
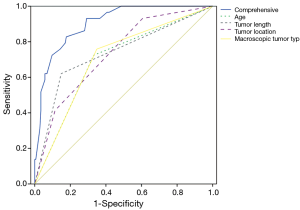
Then, we decided to perform a multivariate analysis to develop a scoring system. The results of the multivariate analysis indicated that age (<56 years), tumor length (>4.45 cm), tumor location and macroscopic tumor type were independent predictors of RLNLN metastases in ESCC (Table 3), and tumor location was the most significant predictor. The value of Hosmer-Lemeshow goodness of fit test was 0.889 and the area under roc curve of the model was 0.905. Compared with the predictive ability of individual risk factors, this comprehensive model demonstrated better predictive power (Figure 1).
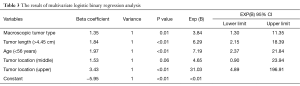
Full table
The scoring system
The weights of the four independent predictors of RLN LN metastasis were different, and the beta coefficients from this multivariate model were rounded to establish a weighted scoring system (Table 4). The 204 patients were divided into low- (0–2 point), moderate- (3–4 points), and high-risk (>4 points) subgroups using the scoring system. The RLNLN metastases rates for the three subgroups were 0% (0/90), 9.8% (6/61) and 43.4% (23/53). A Pearson chi-square test showed that positive rates had statistically significant differences in the three subgroups (P<0.01). Patients with tumors located in the lower thoracic region, tumor length (≤4.45 cm), age (≥56 years) and superficial type of macroscopic tumor type had the lowest rate of RLNLN metastases, which was 0% (0/90).
Full table
The necessity of RLNLN dissection in the dissection group required further analysis. Hence, complications and survival rates were compared between the dissection group and the control group. First, we knew that the major complications of RLN injury included hoarseness, anastomotic fistula and pulmonary complications from previous studies (17,21,22). The number of complications in the dissection group was greater than in the control group, and the differences were statistically significant (Table 5). Second, the dissection group did not improve the survival rate when compared with the control group (Figure 2). The one-year, three-year and five-year survival rates of the dissection group were 86.1%, 60.1% and 45.8%, respectively. On the contrary, the one-year, three-year and five-year survival rate of the control group is 88.8%, 67.1% and 32.9%, respectively. Furthermore, the rate of RLNLN metastases was 0% in the low-risk subgroup of the dissection group.
Full table
Discussion
In present research, we constructed a novel multivariate scoring system that accurately predicted RLNLN metastases in patients with early stage ESCC using statistical methods. Furthermore, we explored the indications for selective RLNLN dissection in early stage ESCC patients from three aspects: survival rate, postoperative complications and RLNLN metastases rate. We proposed that this scoring system had the potential to guide intraoperative RLNLN dissection strategies and to improve the postoperative quality of life for the early stage ESCC patients.
The risk factors for LNM have been explored in previous studies, which indicated that tumor location, tumor length, T stage, macroscopic tumor type, tumor differentiation and LVI were risk factors for LNM in esophageal carcinoma (18,19). However, these studies included patients with both ESCC and esophagus adenocarcinoma, or they did not independently explored the risk factors for RLNLN metastases. RLNLN is one of the most common metastatic sites in esophageal cancer (9,23). Radical esophageal cancer resection, however, may result in postoperative impairment or damage of the RLN (17). Besides, esophagectomy combined with extensive lymphadenectomy along the RLNs has remained technically challenging for thoracic surgeons (24).
RLNLN dissection is important and difficult in ESCC surgery. Some experts consider regular RLNLN dissection necessary for ESCC surgery because RLNLN dissection leads to accurate postoperative pathological staging, which can facilitate patients to obtain more appropriate treatment. Furthermore, RLNLN metastases are risk factors for cervical LNM. RLNLN metastases are one of the most common mediastinal LNMs in ESCC. The rates of RLNLN metastases ranged from 17.11% to 44% in previous reports (10,24), and the rate was 14.2% (29/204) in our center. Hence, RLNLN dissection is necessary for radical resection (9,24).
However, regular RLNLN dissection increases the rate of postoperative RLN injury, which is one of the most common complications during ESCC surgery (25). Damage of RLNs includes resection, blood supply blockage for nerve nutrition, thermal damage, incorrect ligation, contusion and traction. The function of the vocal cords will recover in one year postoperatively, which depends on the extent of the laryngeal recurrent nerve injury (17). The diagnostic process for laryngeal recurrent nerve injury is based on a previous report (26). The rate of laryngeal recurrent nerve injury in our center was 10.3% (32/311). RLN injury could lead to vocal cord paralysis and increase pulmonary complications and anastomotic fistula rates (21,22), for which potential mechanism needed further investigation. Because of the difficulty of RLNLN dissection during ESCC surgery, the requirement for a surgeon’s dissection techniques and experience is high (24). Consequently, we consider that surgeons should adhere to the principle of “precise and accurate RLNLN dissection”. The principle “precise and accurate RLNLN dissection” means that the benefit of RLNLN dissection should be maximizing and the injury of RLN should be minimizing.
Is it suitable for patients with early stage ESCC to regularly undergo RLNLN dissection? To solve this problem, we studied the characteristics of patients with early stage ESCC and developed a novel multivariate scoring system. In this study, the hazard ratios were 31.039 for tumor location (upper thoracic), 7.196 for age (<56 years), 6.299 for tumor length (>4.45 cm) and 3.845 for macroscopic tumor type. Tumor location was considered as the major independent risk factor for RLNLN metastases in the early ESCC patients who underwent esophagectomy (Table 3). According to the scoring system, 204 patients could be divided into low-, moderate- and high-risk subgroups. The RLNLN metastases rates for the three subgroups were, respectively, 0% (0/90), 9.8% (6/61) and 43.4% (23/53). The value of Hosmer-Lemeshow goodness of fit test was over 0.05 (P=0.889). The area under roc curve of the model was more than 0.9 which proved this scoring system had a high accuracy to predict RLNLN metastases.
In an overall analysis of our data, we compared the dissection group with the control group and found that the survival rate seems not show a significantly better in the dissection group when compared with the control group. There was no high-level or some low-level evidences showed that RLNLN dissection influenced the prognosis of esophageal carcinoma (27). Many reports have showed that significant postoperative morbidity and mortality are associated with RLNLN dissection (28). In our study, we also found that the complications in the dissection group were significant higher than in the control group. Meanwhile, the further subgroup analysis showed the RLNLN metastases rate in the low-risk subgroup was 0%. Therefore, we propose that common RLNLN dissection is unnecessary for patients in the low-risk subgroup because of very low risk of RLN lymph node metastasis, less complications and may do not affect survival.
The data in our findings were stable and reliable because they were collected by a full-time thoracic surgeon. A total of 12.2% (38/311) patients were lost to follow-up because their telephone number changed. Patients who were lost to follow-up were confirmed through the register of the Department of Civil Affairs of China, and the missing values were analyzed with SPSS 19.0 software. The representation of our findings is good because of sufficient patients and strictly formulated inclusion and exclusion criteria. All independent variables have a definitive source, and all complications have definitive diagnostic criteria.
Our study was the first to develop a multivariate scoring system for predicting RLNLN metastases in early stage ESCC. This simple flexible scoring system provided a more precise and inexpensive predictive method to precisely evaluate the incidence of RLNLN metastases. Our scoring system was very comprehensible and easy convenient to use. All of the involved risk factors were easy to estimate and score, in which tumor length, tumor location and macroscopic tumor type could be evaluated by preoperative electronic gastroscopy and imaging tests.
However, our study had several limitations and shortcomings. For the retrospective design of this single-center study, selection bias was unavoidable and further multi-institutional studies with larger sample size were needed to verify the results. Besides, the selection of RLNLN dissection was dependent on the operative surgeons involved, our study had selection bias. In addition, no patient has received neoadjuvant chemoradiation because the current guidelines of the National Comprehensive Cancer Network haven’t suggested adjuvant treatments for patients with early stage, which might affect lymph node status. Last but not least, we could not compare our results with other reports, because no report has evaluated the incidence of RLNLN metastases.
Conclusions
In summary, we developed a new simple flexible scoring system that accurately estimated the risks of RLNLN metastases for early stage ESCC patients via analysis of age, tumor length, tumor location and macroscopic tumor type. This scoring system is feasible and flexible. Our study suggested that common RLNLN dissection may be safely omitted in esophagectomy for ESCC patients in the low-risk subgroup. In addition, endoscopic ultrasonography and PET for assessing preoperative T stage and N stage are necessary. Accumulation of more data and prospective studies are needed in the future as how to curtail unnecessary LN dissection is still one of the most important issues to be resolved for EC.
Acknowledgements
Funding: This study was supported by Fujian Medical Innovation Fund (2014-CX-15), Fujian Medical University Professor Fund (JS12008), and the Fund of Union Hospital (2015TC-1-048 and 2015-TC-2-004).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of the Affiliated Union Hospital of Fujian Medical University (No. 2016KY022) and a waiver of the informed consent process was granted.
References
- Pennathur A, Gibson MK, Jobe BA, et al. Oesophageal carcinoma. Lancet 2013;381:400-12. [Crossref] [PubMed]
- Ma G, Zhang X, Ma Q, et al. A novel multivariate scoring system for determining the prognosis of lymph node-negative esophageal squamous cell carcinoma following surgical therapy: an observational study. Eur J Surg Oncol 2015;41:541-7. [Crossref] [PubMed]
- Jamieson GG, Lamb PJ, Thompson SK. The role of lymphadenectomy in esophageal cancer. Ann Surg 2009;250:206-9. [Crossref] [PubMed]
- Akutsu Y, Matsubara H. Lymph node dissection for esophageal cancer. Gen Thorac Cardiovasc Surg 2013;61:397-401. [Crossref] [PubMed]
- Wu N, Chen Z, Pang L, et al. Prognostic significance of lymph node characteristics on survival in esophageal squamous cell carcinomas. Wien Klin Wochenschr 2013;125:26-33. [Crossref] [PubMed]
- Liu YP, Ma L, Wang SJ, et al. Prognostic value of lymph node metastases and lymph node ratio in esophageal squamous cell carcinoma. Eur J Surg Oncol 2010;36:155-9. [Crossref] [PubMed]
- Jang HJ, Lee HS, Kim MS, et al. Patterns of lymph node metastasis and survival for upper esophageal squamous cell carcinoma. Ann Thorac Surg 2011;92:1091-7. [Crossref] [PubMed]
- Li CL, Zhang FL, Wang YD, et al. Characteristics of recurrence after radical esophagectomy with two-field lymph node dissection for thoracic esophageal cancer. Oncol Lett 2013;5:355-9. [PubMed]
- Taniyama Y, Nakamura T, Mitamura A, et al. A strategy for supraclavicular lymph node dissection using recurrent laryngeal nerve lymph node status in thoracic esophageal squamous cell carcinoma. Ann Thorac Surg 2013;95:1930-7. [Crossref] [PubMed]
- Li H, Yang S, Zhang Y, et al. Thoracic recurrent laryngeal lymph node metastases predict cervical node metastases and benefit from three-field dissection in selected patients with thoracic esophageal squamous cell carcinoma. J Surg Oncol 2012;105:548-52. [Crossref] [PubMed]
- Chen J, Liu S, Pan J, et al. The pattern and prevalence of lymphatic spread in thoracic oesophageal squamous cell carcinoma. Eur J Cardiothorac Surg 2009;36:480-6. [Crossref] [PubMed]
- Udagawa H, Ueno M, Shinohara H, et al. The importance of grouping of lymph node stations and rationale of three-field lymphoadenectomy for thoracic esophageal cancer. J Surg Oncol 2012;106:742-7. [Crossref] [PubMed]
- Natsugoe S, Okumura H, Matsumoto M, et al. Reconstruction of recurrent laryngeal nerve with involvement by metastatic node in esophageal cancer. Ann Thorac Surg 2005;79:1886-9. [Crossref] [PubMed]
- Duda M, Adamčík L, Škrovina M, et al. Complications and risks of the surgery of tumors of the upper digestive tract (Foregut) Part I: Esophagus. Rozhl Chir 2013;92:523-9. [PubMed]
- Colvin H, Dunning J, Khan OA. Transthoracic versus transhiatal esophagectomy for distal esophageal cancer: which is superior? Interact Cardiovasc Thorac Surg 2011;12:265-9. [Crossref] [PubMed]
- Merati AL, Shemirani N, Smith TL, et al. Changing trends in the nature of vocal fold motion impairment. Am J Otolaryngol 2006;27:106-8. [Crossref] [PubMed]
- Gelpke H, Grieder F, Decurtins M, et al. Recurrent laryngeal nerve monitoring during esophagectomy and mediastinal lymph node dissection. World J Surg 2010;34:2379-82. [Crossref] [PubMed]
- Li B, Chen H, Xiang J, et al. Pattern of lymphatic spread in thoracic esophageal squamous cell carcinoma: A single-institution experience. J Thorac Cardiovasc Surg 2012;144:778-85; discussion 785-6. [Crossref] [PubMed]
- Ma H, Li Y, Ding Z, et al. The clinical significance of subcarinal lymph node dissection in the radical resection of oesophageal cancer. Interact Cardiovasc Thorac Surg 2013;16:839-43. [Crossref] [PubMed]
- Kaiyo T, Hiroyasu M, Hiromasa F, et al. Japanese Classification of Esophageal Cancer, tenth edition: part I. Esophagus 2009;6:1-25.
- Mariette C, Piessen G. Oesophageal cancer: how radical should surgery be? Eur J Surg Oncol 2012;38:210-3. [Crossref] [PubMed]
- Gockel I, Kneist W, Keilmann A, et al. Recurrent laryngeal nerve paralysis (RLNP) following esophagectomy for carcinoma. Eur J Surg Oncol 2005;31:277-81. [Crossref] [PubMed]
- Taniyama Y, Miyata G, Kamei T, et al. Complications following recurrent laryngeal nerve lymph node dissection in oesophageal cancer surgery. Interact Cardiovasc Thorac Surg 2015;20:41-6. [Crossref] [PubMed]
- Shen Y, Zhang Y, Tan L, et al. Extensive mediastinal lymphadenectomy during minimally invasive esophagectomy: optimal results from a single center. J Gastrointest Surg 2012;16:715-21. [Crossref] [PubMed]
- Suda K, Ishida Y, Kawamura Y, et al. Robot-assisted thoracoscopic lymphadenectomy along the left recurrent laryngeal nerve for esophageal squamous cell carcinoma in the prone position: technical report and short-term outcomes. World J Surg 2012;36:1608-16. [Crossref] [PubMed]
- Schneider B, Schickinger-Fischer B, Zumtobel M, et al. Concept for diagnosis and therapy of unilateral recurrent laryngeal nerve paralysis following thoracic surgery. Thorac Cardiovasc Surg 2003;51:327-31. [Crossref] [PubMed]
- Yang H, Wang J, Huang Q, et al. Intraoperative ultrasonography for the identification of thoracic recurrent laryngeal nerve lymph nodes in patients with esophageal cancer. Dis Esophagus 2016;29:152-8. [Crossref] [PubMed]
- Xi Y, Ma Z, Shen Y, et al. A novel method for lymphadenectomy along the left laryngeal recurrent nerve during thoracoscopic esophagectomy for esophageal carcinoma. J Thorac Dis 2016;8:24-30. [PubMed]


