Detection of salivary aspiration using radionuclide salivagram SPECT/CT in patients with COPD exacerbation: a preliminary study
Introduction
Chronic obstructive pulmonary disease (COPD) is a major public health problem. The acute exacerbation of chronic obstructive pulmonary disease (AECOPD) is associated with the worsening of symptoms and quality of life, as well as an increased morbidity and mortality (1-3). COPD exacerbations can be precipitated by several factors, the most common of which is respiratory tract infection. However, the cause of approximately one-third of severe COPD exacerbations cannot be identified. Several studies have shown that COPD exacerbations may be associated with aspiration (4-8).
Pulmonary aspiration can occur as a result of swallowing dysfunction, gastro-oesophageal reflux, or an inability to adequately protect the airway from oral secretions. Chronic aspiration of saliva is the least-commonly recognized form of aspiration and is usually not diagnosed prior to the development of significant lung injury. In addition, there is currently no standard test for the detection and evaluation of salivary aspiration. The role of salivary aspiration in COPD exacerbation has not been demonstrated convincingly. If salivary aspiration is confirmed to be an important precipitant or aggravating factor of COPD exacerbations, strategies to prevent aspiration have the potential to improve quality of life and survival and reduce health care costs.
Radionuclide salivagram is a useful method for detecting salivary aspiration during small bolus swallows. However, it is mostly used in pediatric patients (9-12), and no previous study has assessed its utility in AECOPD patients. Furthermore, in all studies of radionuclide salivagram, only traditional planar images were obtained, and the poor spatial and temporal resolution of planar images and the lack of anatomic landmarks are limiting factors. Single photon emission computed tomography/computed tomography (SPECT/CT) allows the coregistration of functional and anatomic imaging and has been used for a wide array of oncologic and non-oncologic indications (13-15). However, no study to date has examined the clinical value of the combination of planar images and SPECT/CT fusion images for the detection salivary aspiration.
Therefore, the purpose of this study was to assess the utility of radionuclide salivagram for detecting salivary aspiration in AECOPD patients. This study also evaluated the added value of SPECT/CT in combination with radionuclide salivagram for detecting salivary aspiration in AECOPD patients.
Methods
Patients
Consecutive AECOPD patients at Guangzhou Institute of Respiratory Disease were enrolled in this study between April 2012 and March 2014. The inclusion criteria were the following: (I) ≥50 years of age; (II) smoking history of ≥30 packs of cigarettes per year; (III) medical history and physical examination, chest radiography, and pulmonary function test (PFT) results consistent with the diagnosis of COPD; (IV) ratio of post-bronchodilator forced expiratory volume in 1 s (FEV1) to forced vital capacity (FVC) of 70% or less; and (V) case fulfills COPD exacerbation criteria (worsened dyspnoea, increased cough and/or expectoration beyond the daily variation, and requirement for additional drug therapy). The exclusion criteria were the following: (I) previous history of swallowing problems; (II) known neurological disease; (III) known gastro-oesophageal reflux disease; and (IV) incomplete information.
Our final study population included 52 AECOPD patients (5 women and 47 men; age range, 53–88 years, mean age: 73±9 years). Patient characteristics are shown in Table 1. History assessment, physical examination, calculation of body mass index (BMI), exacerbation frequency in the past year, chest radiography and the modified Medical Research Council (mMRC) dyspnoea scale were evaluated after admission. Water swallow test (a widely used test for aspiration) and radionuclide salivagram were performed on the day immediately before hospital discharge for all subjects. This study was approved by the Scientific Research Ethics Review Committee of the First Affiliated Hospital of Guangzhou Medical University, and all subjects signed a written informed consent form.
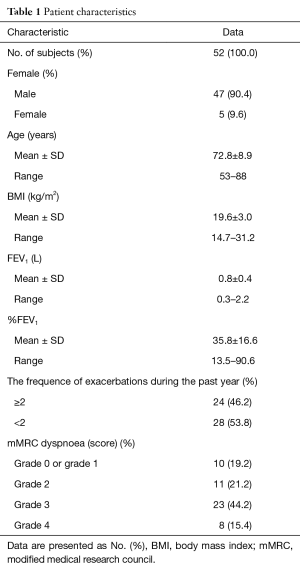
Full table
Water swallow test
Patients were asked to drink 30 mL of water without interruption. Any coughing or throat clearing was indicative of an abnormal water swallow test. The water swallow test results were classified as follows: grade 1: no interruption, no choking or coughing; grade 2: two or more interruptions, no choking or coughing; grade 3: no interruption, with coughing; grade 4: more than two interruptions, with choking; grade 5: frequent cough, cannot swallow entirely. Patients with grade 3 to 5 results were considered positive for aspiration.
Radionuclide salivagram
Preparation of radioactive tracer
The radiopharmaceutical was Tc-99m sulphur colloid (SC). It was prepared using kits provided by Guangzhou Atom High-tech Isotope Pharmaceutical Co., Ltd. (Guangzhou, China) that contained 3 separate nonradioactive components: (I) 1.5 mL solution of 0.148 N HCl in a reaction vial; (II) 1 mL solution of 2.0 mg sodium thiosulfate, 18.1 mg gelatin (porcine), and 2.3 mg sodium edetate; and (III) 1 mL solution of 0.8 M phosphate buffer. Tc-99m SC was prepared by adding 1–3 mL of Tc-99m pertechnetate to the reaction vial at a dosage of 3,700–7,400 MBq (10–20 mCi) and then immediately adding component B. Next, the vial was placed into a boiling water bath for 3 min. Finally, the vial was cooled, and component C was added, and the solution was mixed thoroughly.
Radionuclide salivagram dynamic acquisition
Salivagram was performed using a modification of the method reported previously (9,16). The radiopharmaceutical was Tc-99m SC at a dosage of 74.0 MBq (2 mCi) in 20 mL normal saline in a syringe. The syringe was attached to an infusion prolonged tube (150 cm in length and 0.1 cm in diameter), and the distal end of the tube was placed inside the mouth of the patient. Tc-99m SC was continuously infused into the oral cavity using a micro-injection pump (WZ-50C6T, Zhejiang University Medical Instrument Co., Ltd. Zhejiang, China) over 30 min.
No patient preparation was required before the examination. During this period, the patients were asked to maintain normal swallowing activity. Imaging was performed using a Siemens Symbia T16 SPECT/CT system (Siemens Healthcare, Munich, Germany) with a 128×128 matrix and a low energy high resolution (LEHR) collimator and Zoom of 1.45. Patients were allowed to swallow naturally in the supine position, and posterior planar images from the mouth to the stomach were obtained. The dynamic acquisition occurred over 30 min at a rate of one frame per 30 s. If no radioactivity was detected in the bronchi or lungs throughout the dynamic acquisition, static images in the anterior and posterior projections were acquired with 5-min delay at 6 h after the radiopharmaceutical instillation with a 256×256 matrix, and Zoom of 1.45.
SPECT/CT acquisition
If the dynamic acquisition was positive for aspiration, the patients were given 100 mL of water to drink, and then SPECT/CT fusion images were obtained. SPECT scanning was performed in a 64×64 matrix over 360° (with a 6° step and 20 s per frame). CT was then performed in the same position (130 kV and 80–120 mA) with a slice thickness of 3 mm.
Image interpretation
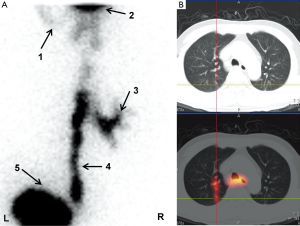
All images were interpreted independently by two experienced nuclear medicine physicians without knowledge of the subjects’ histories. The final diagnosis was obtained by consensus of the two readers. The images were analyzed by visual interpretation as follows:
Positive aspiration: Radioactivity present in the bronchus and/or lung fields (Figure 1). Negative aspiration: No evidence of radioactivity in the bronchi or lungs. Radiotracer activity only observed from the mouth through the esophagus and into the stomach. The severity of aspiration was scored as grade 1 if the activity was only present in the location of the main bronchi and grade 2 if the activity was also present in the more peripheral bronchi ramifications (17).

Statistical analysis
The results are expressed as the means ± SD or medians. The radionuclide salivagram and water swallow test results were compared using kappa values, with excellent agreement represented by kappa values greater than 0.75. The relationship between radionuclide salivagram results and exacerbation frequency was evaluated with the Person χ2 test, and 95% confidence intervals (CI) were calculated. P values less than 0.05 were considered to indicate a statistically significant difference. Statistical calculations were performed using the SPSS18.0 software.
Results
Frequency and time of salivary aspiration
All subjects completed the radionuclide salivagram, and they did not complain of any discomfort. Salivary aspiration was diagnosed by radionuclide salivagram in 17 of the 52 AECOPD patients (33%) and was excluded in the other 35 patients (67%). Among the positive salivagram cases, aspiration into the following areas was observed: right main bronchus and branch in 8 patients (47%), bilateral main bronchi in 6 patients (35%), and left lung field in 3 patients (18%). In regards to aspiration severity, 3 cases were classified as grade 1 and 14 as grade 2. Regarding the timing of visualization of salivary aspiration after oral administration of the radiotracer, the earliest was at 3 min, and the latest was at 25 min (median 20 min).
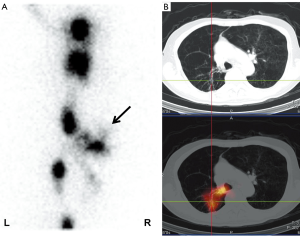
SPECT/CT findings
A total of 13 AECOPD patients with positive aspiration underwent SPECT/CT fusion images. SPECT/CT provided more accurate information on the extent and location of salivary aspiration. Radiotracer was present at the bronchus level in 2 out of 13 patients, and this SPECT/CT finding was consistent with the planar imaging findings. Radiotracer was present at the level of the segmental bronchus and beyond in 11 out of 13 patients (Figure 2). However, in those patients, planar imaging did not identify the actual level of penetration of the radiotracer. Moreover, SPECT/CT revealed salivary aspiration caused aspiration pneumonia in 8 cases (Figure 3).
Comparison of radionuclide salivagram and water swallow test results
Eleven of 52 patients had a positive water swallow test. Six patients with positive salivary aspiration findings on salivagram had negative water swallow test results; whereas, all patients with abnormal water swallow test results were positive for salivary aspiration on salivagram (Table 2). There was general agreement between the radionuclide salivagram and water swallow test results (Kappa =0.712; 95% CI 0.504–0.920; P<0.001).
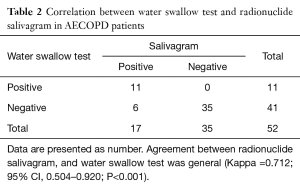
Full table
Correlation between radionuclide salivagram and exacerbation frequency
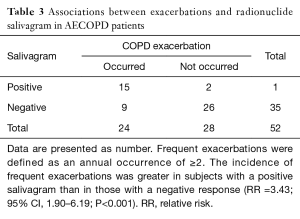
Frequent exacerbations were defined as an annual occurrence of ≥2 (18). The incidence of frequent exacerbations was greater among subjects with positive salivagram than among those with negative salivagram results (RR =3.43; 95% CI, 1.90-6.19; P<0.001) (Table 3).
Full table
Discussion
Radionuclide salivagram is an objective method for detecting salivary aspiration. The unique advantages of salivagram include the following: (I) safety and ease of performance; (II) ease of acceptance and cooperation of patients; (III) consistency with normal physiological swallowing conditions; (IV) ability to reveal more distal penetration (19); and (V) long-term monitoring. Our study of radionuclide salivagram showed that salivary aspiration was frequent (33%) in AECOPD patients, which suggests that salivary aspiration plays an important role in COPD exacerbation.
The localization of salivary aspiration is related to the construction of each bronchial tree and the posture of the patient during aspiration. In our study, the most common location of salivary aspiration was the right main bronchus and branch, which is due to the vertical position of the right main bronchus and its larger diameter compared to the left main bronchus. As salivary aspiration events often occur intermittently, dynamic imaging can detect salivary aspiration during swallowing for a long duration. Therefore, this approach is useful to improve the detection accuracy of salivary aspiration. All salivary aspiration was observed in the initial dynamic acquisition phase of the study, which is consistent with the previously reported data (12). However, the occurrence time of aspiration varied among the included patients; thus, further studies are needed to determine whether aspiration time point is associated with the severity of AECOPD.
Pulmonary aspiration can be assessed by a number of methods, including clinical assessment (e.g., water swallow test), videofluoroscopic swallowing study (VFSS), and fiberoptic endoscopic evaluation of swallowing (FEES). The water swallow test is a widely used test for aspiration that is perceived to be simple and easy to perform and can be repeated frequently; however, it fails to identify all patients with salivary aspiration. VFSS can be used to directly evaluate the oropharyngeal and esophageal phases of swallowing. However, it has significant false-negative results in predicting those who will progress to have aspiration pneumonia (20), and it uses a greater radiation dose (1.23 mSv), which limits the ability to perform frequent follow-up examinations (21). FEES can be performed at the bedside and does not expose the patient to radiation; however, it is invasive and difficult to perform (18). Our study compared radionuclide salivagram and water swallow test results. Six patients with positive salivary aspiration findings on salivagram were negative on the water swallow test. Thus, 14.6% of the patients (6/41) had false negative results on the water swallow test. Therefore, a normal water swallow test result did not rule out salivary aspiration in these AECOPD patients.
In the present study, we demonstrated the clinical application of SPECT/CT for the detection of salivary aspiration in patients experiencing a COPD exacerbation. SPECT/CT provides anatomic and functional information, which has revolutionized the field of diagnostic medical imaging. The values of SPECT/CT include the following: (I) The poor spatial resolution of planar images prevents them from accurately identifying the actual level of penetration of the radiotracer in the segmental bronchus and beyond. In contrast, SPECT/CT shows the precise anatomic location of salivary aspiration. Furthermore, accurate positioning helps to identify tracheal aspiration that may otherwise be missed on planar salivagram dynamic images because of overlapping of the trachea with the esophagus. In our experience, SPECT/CT images did not identify more cases of salivary aspiration than salivagram with planar imaging; however, they did allow for more precise identification of the location of salivary aspiration. (II) Physicians require sensitive and specific imaging techniques to reflect the relationship between salivary aspiration and aspiration pneumonia. SPECT/CT fusion imaging accurately reveals the degree of respiratory tract infections caused by salivary aspiration. Salivary aspiration location is consistent with the areas of the respiratory tract that are infected. In this study, SPECT/CT provided strong evidence establishing salivary aspiration as a direct cause of respiratory tract infection.
The swallowing reflex is an important defense against airway infection resulting from the aspiration of misdirected oropharyngeal or gastric contents into the larynx and lower airway. Therefore, impairment of this reflex is directly associated with an increased risk of silent aspiration and pneumonia (22,23). In 2010, Terada et al. (8) found that an abnormal swallowing reflex is associated with an increased frequency of COPD exacerbations. Our results showed that salivary aspiration is associated with an increased frequency of COPD exacerbations within the previous year. This is important for understanding the relationship between aspiration and COPD exacerbations.
In this study of AECOPD patients, we confirmed that radionuclide salivagram can identify the presence of salivary aspiration. We also showed that radionuclide salivagram with SPECT/CT is a more sensitive technique for visualizing salivary aspiration than radionuclide salivagram with planar imaging. However, this study had some limitations. First, it was performed at a single center, which may limit the generalizability of our results. Second, radionuclide salivagram was performed on the day immediately before hospital discharge for all subjects in consideration of patient safety. Therefore, our findings may only be generalizable to convalescent AECOPD patients.
Conclusions
Radionuclide salivagram is a useful method for detecting salivary aspiration in AECOPD patients. Moreover, SPECT/CT more accurately visualizes the penetration of the radiotracer than planar imaging, and the results of this study suggest a possible role of salivary aspiration in the pathophysiology of aspiration pneumonia.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the Scientific Research Ethics Review Committee of the First Affiliated Hospital of Guangzhou Medical University, and all subjects signed a written informed consent form.
References
- Wedzicha JA, Singh R, Mackay AJ. Acute COPD exacerbations. Clin Chest Med 2014;35:157-63. [Crossref] [PubMed]
- Spencer S, Calverley PM, Burge PS, et al. Impact of preventing exacerbations on deterioration of health status in COPD. Eur Respir J 2004;23:698-702. [Crossref] [PubMed]
- Seemungal TA, Donaldson GC, Bhowmik A, et al. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2000;161:1608-13. [Crossref] [PubMed]
- Ohta K, Murata K, Takahashi T, et al. Evaluation of swallowing function by two screening tests in primary COPD. Eur Respir J 2009;34:280-1. [Crossref] [PubMed]
- Gross RD, Atwood CW Jr, Ross SB, et al. The coordination of breathing and swallowing in chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2009;179:559-65. [Crossref] [PubMed]
- Kobayashi S, Kubo H, Yanai M. Impairment of the swallowing reflex in exacerbations of COPD. Thorax 2007;62:1017. [Crossref] [PubMed]
- Singh B. Impaired swallow in COPD. Respirology 2011;16:185-6. [Crossref] [PubMed]
- Terada K, Muro S, Ohara T, et al. Abnormal swallowing reflex and COPD exacerbations. Chest 2010;137:326-32. [Crossref] [PubMed]
- Baikie G, South MJ, Reddihough DS, et al. Agreement of aspiration tests using barium videofluoroscopy, salivagram, and milk scan in children with cerebral palsy. Dev Med Child Neurol 2005;47:86-93. [Crossref] [PubMed]
- Heyman S, Respondek M. Detection of pulmonary aspiration in children by radionuclide "salivagram". J Nucl Med 1989;30:697-9. [PubMed]
- Baikie G, Reddihough DS, South M, et al. The salivagram in severe cerebral palsy and able-bodied adults. J Paediatr Child Health 2009;45:342-5. [Crossref] [PubMed]
- Somasundaram VH, Subramanyam P, Palaniswamy S. Salivagram revisited: justifying its routine use for the evaluation of persistent/recurrent lower respiratory tract infections in developmentally normal children. Ann Nucl Med 2012;26:578-85. [Crossref] [PubMed]
- Mariani G, Bruselli L, Kuwert T, et al. A review on the clinical uses of SPECT/CT. Eur J Nucl Med Mol Imaging 2010;37:1959-85. [Crossref] [PubMed]
- Scheyerer MJ, Pietsch C, Zimmermann SM, et al. SPECT/CT for imaging of the spine and pelvis in clinical routine: a physician's perspective of the adoption of SPECT/CT in a clinical setting with a focus on trauma surgery. Eur J Nucl Med Mol Imaging 2014;41 Suppl 1:S59-66. [Crossref] [PubMed]
- Tharp K, Israel O, Hausmann J, et al. Impact of 131I-SPECT/CT images obtained with an integrated system in the follow-up of patients with thyroid carcinoma. Eur J Nucl Med Mol Imaging 2004;31:1435-42. [Crossref] [PubMed]
- Drubach LA, Zurakowski D, Palmer EL 3rd, et al. Utility of salivagram in pulmonary aspiration in pediatric patients: comparison of salivagram and chest radiography. AJR Am J Roentgenol 2013;200:437-41. [Crossref] [PubMed]
- Yang J, Codreanu I, Servaes S, et al. Radionuclide Salivagram and Gastroesophageal Reflux Scintigraphy in Pediatric Patients: Targeting Different Types of Pulmonary Aspiration. Clin Nucl Med 2015;40:559-63. [Crossref] [PubMed]
- Burgel PR, Nesme-Meyer P, Chanez P, et al. Cough and sputum production are associated with frequent exacerbations and hospitalizations in COPD subjects. Chest 2009;135:975-82. [Crossref] [PubMed]
- Parrilla C, Valenza V, Calò L, et al. Is it sufficient to quantify aspiration for predicting aspiration pneumonia? Clin Nucl Med 2008;33:236-9. [Crossref] [PubMed]
- Aviv JE, Sacco RL, Mohr JP, et al. Laryngopharyngeal sensory testing with modified barium swallow as predictors of aspiration pneumonia after stroke. Laryngoscope 1997;107:1254-60. [Crossref] [PubMed]
- Treves ST, Baker A, Fahey FH, et al. Nuclear medicine in the first year of life. J Nucl Med 2011;52:905-25. [Crossref] [PubMed]
- Ramsey D, Smithard D, Kalra L. Silent aspiration: what do we know? Dysphagia 2005;20:218-25. [Crossref] [PubMed]
- Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med 2001;344:665-71. [Crossref] [PubMed]


