Firm evidence of complete revascularization with culprit and target vessel revascularization only after ST-segment elevation myocardial infarction
We read with great interest the recently published article written by Anantha Narayanan et al. (1) entitled ‘What is the optimal approach to a non-culprit stenosis after ST-elevation myocardial infarction - Conservative therapy or upfront revascularization? An updated meta-analysis of randomized trials’. Non-culprit percutaneous coronary intervention during a ST-segment elevation myocardial infarction (STEMI) is still controversial. Anantha Narayanan et al. (1) performed a meta-analysis of randomized controlled trials comparing a strategy of complete revascularization (CR) with culprit and target vessel revascularization (TVR)-only after SETMI in patients with multi-vessel disease. The authors found concluded that CR strategy in STEMI patients with multi-vessel disease is associated with reduction in major adverse cardiac events (MACE), cardiac mortality and need for repeat revascularization but with no decrease in the risk of subsequent myocardial infarction or all-cause mortality.
AlBalawi et al. (2) found that false positive and false negative meta-analyses are common but infrequently recognized in cardiovascular meta-analyses even among methodologically robust reviews published by the Cochrane Heart group and recommended that meta-analysis and readers should incorporate trial sequential analysis (TSA) when interpreting results. Therefore, we performed TSA of primary outcomes (MACE, all-cause mortality, repeat revascularization and myocardial infarction) of CR strategy versus TVR in STEMI patients in order to well interpret and understand the evidence presented by the authors (1). The TSA was performed using a priori diversity-adjusted information size (APDIS) with α=0.05, β=0.2 (power 80%), and 30% of an anticipated intervention effect of relative risk reduction (2-6).
The results of meta-analyses and TSA of primary outcomes were presented in Table 1. The TSA of MACE showed that the 2,004 (84.3%) of the 2,376 APDIS was accrued (Figure 1). The cumulative z-curve crossed both the conventional boundary and the trial sequential monitoring boundary providing firm evidence of decreased MACE in STEMI patients with multi-vessel diseases treated with CR and TVR. The TSA of all-cause mortality showed that the 2,004 (28.4%) of the 7,058 APDIS was accrued. The cumulative z-curve did not cross both the conventional boundary and the trial sequential futility boundary. The TSA of repeat revascularization showed that the 1,044 (78.3%) of the 1,334 APDIS was accrued. The cumulative z-curve crossed both the conventional boundary and the trial sequential futility boundary and reached the APDIS. The TSA of myocardial infarction showed that the 1,671 (36.3%) of the 4,609 APDIS was accrued. The cumulative z-curve crossed the conventional boundary but did not cross the trial sequential monitoring boundary.
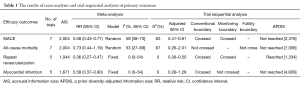
Full table
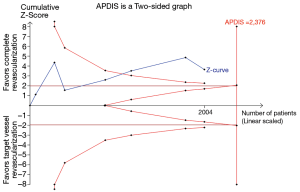
In summary, the TSA results showed that the results of MACE and repeat revascularization have been confirmed, but the result of all-cause mortality might be potential false-negative and the result of myocardial infarction might be potential false-positive. The TSA results suggested that the CR strategy was better than TVR in STEMI patients with multi-vessel disease.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Anantha Narayanan M, Reddy YN, Sundaram V, et al. What is the optimal approach to a non- culprit stenosis after ST-elevation myocardial infarction - Conservative therapy or upfront revascularization? An updated meta-analysis of randomized trials. Int J Cardiol 2016;216:18-24. [Crossref] [PubMed]
- AlBalawi Z, McAlister FA, Thorlund K, et al. Random error in cardiovascular meta-analyses: how common are false positive and false negative results? Int J Cardiol 2013;168:1102-7. [Crossref] [PubMed]
- Weng H, Zeng XT. How strong is the evidence of culprit-lesion only versus complete multivessel percutaneous intervention in ST-elevation myocardial infarction? Int J Cardiol 2016;223:171-2. [Crossref] [PubMed]
- Gu WJ. Caution! Overestimation of treatment effects of corticosteroid therapy for community-acquired pneumonia in a meta-analysis of randomized controlled trials. J Thorac Dis 2015;7:1885-6. [PubMed]
- Wetterslev J, Thorlund K, Brok J, et al. Trial sequential analysis may establish when firm evidence is reached in cumulative meta-analysis. J Clin Epidemiol 2008;61:64-75. [Crossref] [PubMed]
- Brok J, Thorlund K, Gluud C, et al. Trial sequential analysis reveals insufficient information size and potentially false positive results in many meta-analyses. J Clin Epidemiol 2008;61:763-9. [Crossref] [PubMed]


