Acute chest pain in a triathlete: rupture of the noncoronary sinus of Valsalva into the right ventricle
Introduction
Sinus of Valsalva (SoV) aneurysm is a rare cardiac disease. The prevalence of aneurysms originating from the right coronary sinus (65–85%) is the highest, followed by the noncoronary sinus (10–30%), and the lowest in the left coronary sinus (<5%) (1,2). A web-based search revealed an onset of the disease at 35 years of age and that males predominated with about two thirds of the clinical cases (3). Furthermore, Asians are more frequently affected than other ethnic groups (4). Often the patient is asymptomatic. However, a ruptured SoV aneurysm presents a clinical emergency due to formation of hemodynamically relevant aortic cardiac shunts. Diagnosis of this disease and other common causes of acute heart failure rely on echocardiography.
Case presentation
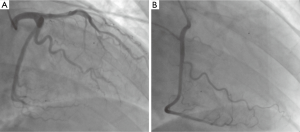
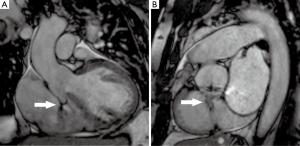
A 45-year-old male was admitted to our emergency department because of acute onset of palpitation and chest pain that started a few hours ago. His medical history has been unremarkable. The patient has frequently taken part in triathlons. His last competition had been eight months ago. Physical examination after admission showed tachycardia with systolic-diastolic cardiac murmur. Transthoracic echocardiography detected a continuous shunt into the right ventricle. The left ventricle was not dilated and showed normal global systolic function and no regional wall motion abnormalities. The right cardiac chambers were enlarged. Laboratory analysis showed creatinine kinase levels of 385 U/L (reference range <171 U/L), creatinine kinase isoenzyme MB levels of 41 U/L (reference range 7–25 U/L) and troponin-Ths levels of 323 ng/L (reference range <14 ng/L). The transaminase levels (glutamate oxalacetate transferase, glutamate pyruvate transferase) were also increased with values of 633 U/L (reference range <35 U/L) and 205 U/L (reference range <45 U/L), respectively. Immediately performed transesophageal echocardiography suspected a ruptured aneurysm of SoV. Hence, the patient was transferred to our ICU. Because of elevated troponin-Ths levels and persistent chest pain the patient underwent coronary angiography. The left (Figure 1A) and right coronary arteries (Figure 1B) showed no signs of stenosis. The thoracic aortogram revealed a contrast jet column directed from one of the aortic sinuses of Valsalva into the right ventricle. For further evaluation of the anatomical relationship we supplemented the diagnostic workup with a cardiovascular margnetic resonance (CMR) examination which revealed a ruptured noncoronary SoV aneurysm with a windsock appearance into the right ventricle (Figure 2). The patient was then shifted to the cardiac surgery unit for emergency repair which confirmed a ruptured noncoronary sinus shunting into the right ventricle (1 cm × 1 cm). The defect was repaired successfully with glutaraldehyde-treated autologous pericardium. The postoperative period was uneventful. The patient was discharged from the Division of Cardiac Surgery eight days following surgery. He was asymptomatic at the first follow-up examination after discharge.
Discussion
Ruptured SoV aneurysms present a clinical emergency because of formation of hemodynamically relevant aortic cardiac shunts that can lead to progressively deteriorating heart failure (5). This rupture can occur with direction towards the right atrium, right ventricle, or left atrium. Therefore, SoV aneurysms should be considered as differential diagnosis for patients who show symptoms of acute heart failure with chest pain and new heart murmurs. Transthoracic echocardiography and transesophageal echocardiography present the main diagnostic methods (6). However, alternative imaging techniques (CMR, CT) have been previously proposed for the diagnosis of SoV aneurysms (3). In the present case, we demonstrate the benefit of CMR in this emergency setting. Due to its high resolution, this method did not only confirm the diagnosis, but also provided more details about rupture localization, shunt direction and functional compromise of the right ventricle, thus optimizing the preoperative planning of the repair strategy. Therefore, CMR has been proved a useful tool to visualize and confirm the pathology of a ruptured SoV in an emergency setting.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Topi B, John J, Agarwal A, et al. An uncommon cause of a continuous murmur. Exp Clin Cardiol 2012;17:148-9. [PubMed]
- Harkness JR, Fitton TP, Barreiro CJ, et al. A 32-year experience with surgical repair of sinus of valsalva aneurysms. J Card Surg 2005;20:198-204. [Crossref] [PubMed]
- Bricker AO, Avutu B, Mohammed TL, et al. Valsalva sinus aneurysms: findings at CT and MR imaging. Radiographics 2010;30:99-110. [Crossref] [PubMed]
- Dong C, Wu QY, Tang Y. Ruptured sinus of valsalva aneurysm: a Beijing experience. Ann Thorac Surg 2002;74:1621-4. [Crossref] [PubMed]
- Post MC, Braam RL, Groenemeijer BE, et al. Rupture of right coronary sinus of Valsalva aneurysm into right ventricle. Neth Heart J 2010;18:209-11. [Crossref] [PubMed]
- Shah RP, Ding ZP, Ng AS, et al. A ten-year review of ruptured sinus of valsalva: clinico-pathological and echo-Doppler features. Singapore Med J 2001;42:473-6. [PubMed]


