Duration of dual antiplatelet therapy (DAPT): a call for personalized medicine
Advances in drug-eluting stent (DES) technology have led to a decrease in the risk of developing stent thrombosis (1). Nevertheless, the optimal duration of dual antiplatelet therapy (DAPT) required after DES placement has remained elusive. Data from randomized studies have had conflicting results, with some suggesting that durations of DAPT as short as 3 or 6 months might be as effective in limiting these events as compared with longer durations previously supported by guidelines (2-5). On the other hand, the largest randomized study comparing DAPT durations, the DAPT study, found that continuation of therapy for 30 months significantly reduce rates of stent thrombosis and myocardial infarction (6), including among patients receiving second generation DES, at the expense of increased bleeding (7).
Thus, after randomization of more than 34,000 patients in 11 randomized trials (8), the optimal duration of DAPT after stent implantation has continued to be the subject of considerable debate. To synthesize the latest data and provide more clarity on the topic, the American College of Cardiology and American Heart Association recently release the “2016 ACC/AHA Guideline Focused Update on the Duration of Dual Antiplatelet Therapy in Patients with Coronary Artery Disease” in a March 2016 issue of JACC (9). Here, we review the most significant guideline updates and offer insight into its application in clinical practice.
The focused updated guidelines for patients with DES implantation after acute coronary syndrome continue to recommend a minimum duration of 12 months of DAPT as a class I (level of evidence B) indication based largely on the CURE trial, showing benefit in this sub-group regardless of treatment with revascularization or medical therapy (10). However, the minimum duration of DAPT in patients with elective DES placements for stable ischemic heart disease (SIHD) has been reduced from 1 year to 6 months, a class I (level of evidence B) recommendation. Furthermore, the authors of the focused update provide a class IIb (level of evidence C) recommendation for consideration of just 3 months of DAPT after DES placement for patients who have developed a serious bleeding event or are at high risk of major bleeding complications (9). While prior recommendations calling for 12 months of DAPT after DES placement were in large part driven by observational studies and expert consensus, the updated guidelines reflect the lower incidence of stent thrombosis in new generation stents along with review of studies suggesting low rates of stent-related events after percutaneous coronary intervention (PCI) and SIHD. A large patient level pooled-analysis of randomized control studies comparing short duration DAPT (≤6 months) to longer duration DAPT (12 months) found similar rates of MACE and higher rates of bleeding in the extended therapy arm (11). The studies supporting this recommendation were not considered by the committee to constitute the highest level of evidence, however, due to a number of considerations (12). The possibility of shorter time frames for DAPT in the updated recommendations reflects the minimum therapy necessary to prevent stent thrombosis for 2nd generation DES.
Looking beyond stent thrombosis
The update on dual antiplatelet therapy not only provides guidance for the duration of use of antiplatelet agents but also marks a shift in focus on their role in coronary artery disease. While recognizing the shorter duration of DAPT necessary to limit stent thrombosis, the focused update recommends a careful consideration for extending dual antiplatelet therapy for patients with a favorable ischemic/bleeding profile beyond the minimum recommended duration of DAPT (class IIb, level of evidence A) (9). While the addition of a P2Y12 inhibitor to aspirin has generally been used to prevent stent thrombosis, recent data suggest a benefit beyond just the prevention of this often-catastrophic event. The DAPT study not only showed a reduction of stent thrombosis for individuals on extended dual-antiplatelet therapy after stent implantation compared to placebo [0.4% vs. 1.4%; hazard ratio (HR), 0.29; P<0.001] but also a reduction in myocardial infarction (2.1% vs. 4.1%; HR, 0.47; P<0.001), with more than half of the events prevented being spontaneous myocardial infarction unrelated to the index stent (6). This suggests dual anti-platelet therapy has a role in the treatment of a vulnerable vascular bed apart from its role in limiting stent thrombosis.
This notion has been suggested in other primary and secondary prevention trials including CHARISMA, which randomized individuals at high risk for atherothrombotic events to clopidogrel and aspirin vs. placebo and aspirin for a median of 28 months. While the primary endpoints were not significantly different between the groups, a reduction in MACCE was seen for patients with clinically evident cardiovascular disease (13). Likewise, in PEGASUS-TIMI 54, patients with SIHD (1–3 years removed from a myocardial infarction) receiving ticagrelor (P2Y12 inhibitor) in addition to aspirin had a reduction in MACCE as compared to lone aspirin therapy (14).
Personalized over dogmatic approach
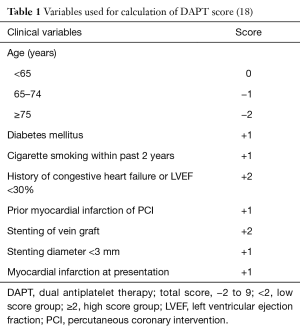
While the benefit of extending dual antiplatelet therapy beyond previously recommended guidelines are apparent for prevention of ischemic events, the risks of major bleeding are a cause for concern. For instance, the extended therapy arm in the DAPT trial had a higher incidence of moderate to severe bleeding as compared to the placebo group (2.5% vs. 1.6%; HR, 1.61; P=0.001) (6), a finding consistent with other studies examining the safety profile of extended dual antiplatelet therapy (11). The significant trade-off in daily clinical practice where individual patient decisions may be more complex and patients may be different than those enrolling in large randomized trials prevents the application of stringent guidelines. The focused update does well to allow clinicians to implement an individualized approach to the optimal DAPT. Clinicians have at their disposal clinical resources to help guide them in their decision process including bleeding scores such as ACUITY, CRUSADE, HAS BLED that can help identify individuals at increased risk of severe bleeding post stent implantation (15). Specific scores stratifying bleeding or ischemic risks after stent implantation have also been created (16,17). Most recently, the DAPT score is the first clinical tool that simultaneously stratifies bleeding and ischemic risks, helping to identify patients that are expected to benefit the most from extending dual anti-platelet therapy after stent implantation beyond 12 months, as well as those likely to be harmed (Table 1) (18). The DAPT score was explicitly identified in the new guidelines as a tool to help clinicians sort through the class IIb recommendations that recommend selective use of longer or shorter durations of DAPT based on individual patient profiles. In the DAPT Study, patients receiving extended P2Y12 inhibitor therapy with DAPT scores ≥2 had the greatest benefit—with fewer myocardial infarction or stent thrombosis events as compared with aspirin therapy and placebo [2.7% vs. 5.7%; risk difference (RD), −3.0% (95% CI, −4.1% to 2.0%); P<0.001], with a negligible increase in bleeding events [1.8% for continued P2Y12 inhibitor vs. 1.4% for placebo; RD 0.4% (95% CI, −0.3% to 1.0%); P=0.26]. Comparatively, patients receiving extended P2Y12 inhibitor therapy with DAPT scores <2 appeared to be harmed, with smaller reductions in myocardial ischemia or stent thrombosis [1.7% for continued P2Y12 inhibitor vs. 2.3% for placebo; RD, −0.7% (95% CI, −1.4% to 0.09%); P=0.07] but a greater increase in bleeding events [3.0% for continued P2Y12 inhibitor vs. 1.4% for placebo; RD, 1.5% (95% CI, 0.8% to 2.3%); P<0 .001] (18).
While these clinical tools allow the clinician some clarity into the appropriate recommendations regarding dual antiplatelet therapy duration, it also promotes a greater emphasis on a personalized approach to decision making apart from guideline driven focus. For instance, the focused update on DAPT guidelines also provides a class IIb recommendation for extending dual antiplatelet therapy after DES placement beyond the minimum 12 months after ACS (9). In a case of 60-year-old male with a history multiple past myocardial infarctions, diabetes and tobacco use who received a DES for an indication of NSTEMI, the calculated DAPT score would be 4. A score ≥2 (high score group) confers a favorable ischemic/bleeding risk profile and should be considered as a marker for benefit from extension of DAPT. However, the DAPT scores (ranging from −2 to 9) likely reflect a continuum of a benefit/risk profile (18). Thus, for our patient who has tolerated DAPT for 12 months without a significant bleeding event, a class IIb recommendation for extension of dual antiplatelet therapy might not accurately reflect the appropriateness of DAPT past 1 year for such an elevated ischemic risk. The use of the relatively simple and easy to use DAPT score not only informs clinicians as to the most appropriate therapy but also can empower patients to become involved in this shared decision making opportunity. A necessary corollary to this is the understanding that patients enrolled in DAPT tolerated therapy for 12 months without significant bleeding events. The discussion of whether to continue treatment should be made after assessing the effect of the initial treatment period.
Gaps in knowledge
Though the updated guidelines introduce the concept of extended dual antiplatelet therapy and clinical scores provide clinicians with guidance on this issue, there remains a significant gap in our understanding of the extent to which DAPT plays a role in clinical practice. For instance, how long beyond 1 year after stent implantation should DAPT be continued for individuals with a favorable ischemic/bleeding risk profile? In the DAPT study, the 3 months after discontinuation of the study drug in the extended therapy arm saw a 2-fold increase in hazard for stent thrombosis or myocardial infarction compared with the final 3 months (months 27–30) of the treatment period (6). This raises the question of whether extending therapy beyond what has been studied in clinical trials for individuals able to tolerate DAPT might be more optimal. Furthermore, in an effort to limit bleeding risks, the on-going international TWILIGHT trial (NCT02270242) will inform us of whether after a minimum duration of DAPT for 3 months post-DES placement, if treatment with a P2Y12 inhibitor (ticagrelor) alone confers the same protection in high risk patients (including patients with acute coronary syndrome) compared to aspirin and ticagrelor over a 12-month period. It’s readily apparent the recommendations around antiplatelet regimens after stent implantation will continue to evolve with the availability of more data and as technologies evolve.
How do we reconcile the notion that newer generation DES have a more favorable stent thrombosis risk profile, limiting the necessary duration of DAPT, with the evidence that longer term DAPT therapy after DES implantation might be more favorable for select individuals? The answer lies in the dual roles for DAPT therapy. While the immediate need for DAPT for protection against stent thrombosis has seen a shortening in necessary anticoagulation, there is evidence for long-term protection against MACCE apart from stent related adverse events in vulnerable patients. There is an obvious trade-off between ischemic protection with the increased risk of major bleeding events. Therein lies the key to applying the updated guidelines for DAPT in coronary artery disease. There is no “one size fits all” model for DAPT. The new guidelines promote an individualized approach to the decision of how long to continue DAPT in patients receiving DES. Clinicians have at their disposal validated clinical tools to help inform themselves and engage their patients in the optimal duration of DAPT after DES placement. This at its heart exemplifies personalized medicine.
Acknowledgements
None.
Footnote
Provenance: This is an invited Editorial commissioned by the Section Editor Feng Zhang (Department of Cardiology, Zhongshan Hospital of Fudan University, Shanghai, China).
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Tada T, Byrne RA, Simunovic I, et al. Risk of stent thrombosis among bare-metal stents, first-generation drug-eluting stents, and second-generation drug-eluting stents: results from a registry of 18,334 patients. JACC Cardiovasc Interv 2013;6:1267-74. [Crossref] [PubMed]
- Feres F, Costa RA, Abizaid A, et al. Three vs twelve months of dual antiplatelet therapy after zotarolimus-eluting stents: the OPTIMIZE randomized trial. JAMA 2013;310:2510-22. [PubMed]
- Gwon HC, Hahn JY, Park KW, et al. Six-month versus 12-month dual antiplatelet therapy after implantation of drug-eluting stents: the Efficacy of Xience/Promus Versus Cypher to Reduce Late Loss After Stenting (EXCELLENT) randomized, multicenter study. Circulation 2012;125:505-13. [Crossref] [PubMed]
- Kim BK, Hong MK, Shin DH, et al. A new strategy for discontinuation of dual antiplatelet therapy: the RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation). J Am Coll Cardiol 2012;60:1340-8. [Crossref] [PubMed]
- Colombo A, Chieffo A, Frasheri A, et al. Second-generation drug-eluting stent implantation followed by 6- versus 12-month dual antiplatelet therapy: the SECURITY randomized clinical trial. J Am Coll Cardiol 2014;64:2086-97. [Crossref] [PubMed]
- Mauri L, Kereiakes DJ, Yeh RW, et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med 2014;371:2155-66. [Crossref] [PubMed]
- Hermiller JB, Krucoff MW, Kereiakes DJ, et al. Benefits and Risks of Extended Dual Antiplatelet Therapy After Everolimus-Eluting Stents. JACC Cardiovasc Interv 2016;9:138-47. [Crossref] [PubMed]
- Bittl JA, Baber U, Bradley SM, et al. Duration of Dual Antiplatelet Therapy: A Systematic Review for the 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2016;68:1116-39. [Crossref] [PubMed]
- Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA Guideline Focused Update on Duration of Dual Antiplatelet Therapy in Patients With Coronary Artery Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2016;68:1082-115. [Crossref] [PubMed]
- Yusuf S, Zhao F, Mehta SR, et al. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001;345:494-502. [Crossref] [PubMed]
- Palmerini T, Sangiorgi D, Valgimigli M, et al. Short- versus long-term dual antiplatelet therapy after drug-eluting stent implantation: an individual patient data pairwise and network meta-analysis. J Am Coll Cardiol 2015;65:1092-102. [Crossref] [PubMed]
- Yeh RW, Kereiakes DJ, Mauri L. Reply: Analysis of Dual Antiplatelet Therapy. J Am Coll Cardiol 2015;66:2056. [Crossref] [PubMed]
- Bhatt DL, Fox KA, Hacke W, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med 2006;354:1706-17. [Crossref] [PubMed]
- Bonaca MP, Bhatt DL, Cohen M, et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med 2015;372:1791-800. [Crossref] [PubMed]
- Costa F, Tijssen JG, Ariotti S, et al. Incremental Value of the CRUSADE, ACUITY, and HAS-BLED Risk Scores for the Prediction of Hemorrhagic Events After Coronary Stent Implantation in Patients Undergoing Long or Short Duration of Dual Antiplatelet Therapy. J Am Heart Assoc 2015;4:e002524. [PubMed]
- PRECISE-DAPT Score Working Group. PRECISE-DAPT Score 2016. Available online: http://www.precisedaptscore.com.
- Baber U, Mehran R, Giustino G, et al. Coronary Thrombosis and Major Bleeding After PCI With Drug-Eluting Stents: Risk Scores From PARIS. J Am Coll Cardiol 2016;67:2224-34. [Crossref] [PubMed]
- Yeh RW, Secemsky EA, Kereiakes DJ, et al. Development and Validation of a Prediction Rule for Benefit and Harm of Dual Antiplatelet Therapy Beyond 1 Year After Percutaneous Coronary Intervention. JAMA 2016;315:1735-49. [Crossref] [PubMed]