Current outcomes of off-pump versus on-pump coronary artery bypass grafting: evidence from randomized controlled trials
Introduction
Despite a large body of evidence, there is an ongoing, controversial debate whether coronary artery bypass graft surgery should be performed with or without extracorporeal circulation. This intense debate is held between three schools of thought: the “pure”, off-pump surgeons, the on-pump surgeons and the “selectivists” group that reserves off-pump surgery for selected cases only. Historically, the shift towards off-pump coronary artery bypass (OPCAB) grafting was proposed both to reduce the operation cost in developing countries but also to avoid the deleterious effects of the contact of blood with the artificial extracorporeal circuit (i.e., mainly the systemic inflammatory response and coagulopathy) (1-3). Furthermore, avoidance of aortic cannulation and minimisation of aortic manipulation would theoretically translate into reduced cerebral stroke, hence reduced morbidity and perioperative mortality (4). On the other hand, on-pump surgeons argue that the comfort of the bypass circuit results in a better anastomotic technique that translates into a more complete revascularization and better graft patency (3).
Developed about 40 decades ago (5-7), OPCAB reached a plateau in Europe, accounting for nearly 15–20% of all coronary operations, while in Asia 60–100% of patients are offered coronary artery bypass grafting (2). A retrospective analysis of the Society of Thoracic Surgeons Adult Cardiac Surgery Database in USA revealed a decline in off-pump operations, currently being used in fewer than one out of five patients (8). The current review focuses on the main outcomes of on-pump coronary artery bypass (ONCAB) grafting versus OPCAB from randomized controlled trials (RCTs) (i.e., level I evidence). The main criticism of RCTs in this area, is the under powering because of recruitment of low risk patients but also because of the low mortality and morbidity of coronary artery bypass grafting that would require very large sample populations to detect a difference (4). Therefore, we will also be reviewing pooled data from recent, updated meta-analyses of randomized trials only. We selected in our review large sample size RCTs or large meta-analyses of RCTs to discuss the hard end-point outcomes but smaller trials were also included to discuss other outcomes.
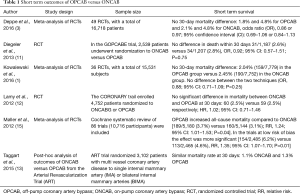
Operative mortality
The majority of the large RCTs to date failed to show a difference in early mortality between off-pump and on-pump surgery (1,3,9-13). One small sample size RCT by Fattouch et al. showed a reduced mortality in patients with ST elevation undergoing urgent/emergent off-pump coronary surgery compared to on-pump surgery (14). Deppe et al. in meta-analysis of RCTs on almost 16,900 patients found no difference in 30-day mortality. Kowalewski et al. in meta-analysis of over 19,000 patients demonstrated no significant difference in short term mortality (1). The evidence is summarised in Table 1.
Full table
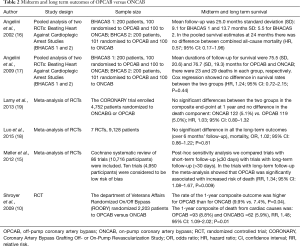
Mid- and long-term survival
Angelini et al. pooled midterm follow-up outcomes from two RCTs—Beating Heart against Cardioplegic Arrest Studies (BHACAS 1 and 2). The mean follow-up was 25.0 months for BHACAS 1, and 13.7 months for BHACAS 2. Combined all-cause mortality did not differ between patients in off-pump and on-pump groups [hazard ratio (HR), 0.57; 95% confidence interval (CI): 0.17–1.96] (16). A later study by the same group found no difference in long term survival up to 6–8 years between on-pump and off-pump coronary surgery (HR, 0.84; 95% CI: 0.58–1.24; P=0.39) (17). The Veterans Affairs Randomized On/Off Bypass (ROOBY) trial randomly assigned 2,203 of patients to either off-pump or on-pump. It was the first trial where off patients were recruited in based on the surgeon’s experience (minimum number of 20 cases) though some argue that the learning curve extends beyond this set point (4). The primary long term (1 year) composite of death, repeat revascularization, non-fatal myocardial infraction was higher (9.9% vs. 7.4%, P=0.04) for the OPCAB group with no significant differences between the individual composite components. The sensitivity analysis revealed a trend toward more death from cardiac causes in the on-pump group (2.7% vs. 1.3%, P=0.03). A Cochrane systematic review of RCTs off-pump versus on-pump found an increased risk of death with off-pump in the long term (>30 days) follow-up studies [relative risk (RR), 1.34; 95% CI: 1.08–1.67; P=0.009] (15). Luo et al. in a recent meta-analysis of RCTs found no difference in patients with over 6 months’ follow-up [odds ratio (OR), 1.02; 95% CI: 0.86–1.22; P=0.81] (18). The Coronary Artery Bypass Grafting Off- or On-Pump Revascularization Study (CORONARY) remains the largest RCT to date that recruited 4,752 patients (12,19). At 1 year the study reported no difference in primary composite of death, myocardial infarction, stroke, or new renal failure requiring dialysis. The primary outcome event had occurred in 288 participants (12.1%) in the off-pump group and 316 participants (13.3%) in the on-pump group (HR with the off-pump procedure, 0.91; 95% CI: 0.77–1.07; P=0.24). There was no significant difference between the rates of the individual primary outcome components. The 5-year long term outcomes from the CORONARY trial are still awaited (Table 2).
Full table
Graft patency, number of grafts and need for repeat revascularization
Graft patency
Graft patency was the primary endpoint in a RCT conducted by Puskas et al. on 200 patients. The authors found similar graft patency between off-pump and conventional surgery at 30 days (absolute difference, 1.3%; 95% CI: −0.66–3.31%; P=0.19) and 1 year (absolute difference, −2.2%; 95% CI: −6.1–1.7%; P=0.27) (20). Similarly, Magee et al. found no difference in vein patency or arterial graft patency at 1 year in 1,920 patients that completed angiographic follow-up (20). Lingaas et al. (21) reported no significant differences in arterial and vein graft patency in 120 patients randomized to OPCAB or ONCAB.
In contrast to previous studies, several trials reported poor graft patency for patients undergoing off-pump. Khan et al. found a poorer graft patency at 3 months for patient undergoing OPCAB (22). Houlind et al. found reduced graft patency in the OPCAB group compared to the on-pump group, on 481 patients that completed angiographic follow-up at 6 months (23). At 1 year follow-up, Widimsky et al. found a lower graft patency for the off-pump vein grafts while the arterial graft patency were similar for both arms (24). The ROOBY trial found a significantly lower graft patency in the off-pump group than in the on-pump group (82.6% vs. 87.8%, P<0.01) at 1 year (10). Similar results were found by Zhang et al. in a recent meta-analysis of 12 RCTs, on a total of 3,894 patients (4,137 grafts). Interestingly, the authors found an increased risk of occlusion of vein grafts but no difference in arterial graft patency [left internal mammary artery (IMA) and radial artery conduits] (25). In the longest follow-up study to date (up to 6 to 8 years) of patients recruited in two randomized trials comparing OPCAB to ONCAB, Angelini et al. demonstrated that the likelihood of graft occlusion was no different between OPCAB (10.6%) and ONCAB (11.0%) groups (OR, 1.00; 95% CI: 0.55–1.81; P>0.99). Furthermore, the authors found the graft occlusion to occur more likely at the distal anastomosis (OR, 1.11; 95% CI: 1.02–1.20) in both groups (17) (Table 3).

Full table
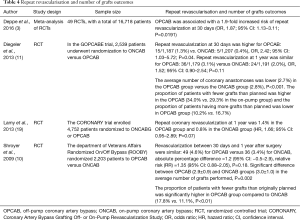
Number of grafts and repeat revascularization
Several trials demonstrated a reduced number of grafts performed in OPCAB arms and increased revascularization rates. The ROOBY trial demonstrated that the proportion of patients with fewer grafts than initially planned was higher in the off-pump arm than in the on-pump arm (17.8% vs. 11.1%, P<0.01) (10). Similarly, the Off-Pump versus On-Pump Coronary-Artery Bypass Grafting in Elderly Patients trial (GOCABE) trial (11) revealed that fewer grafts were performed in the off-pump arm compared to on-pump arm. At 30 days, patients having OPCAB had a higher rate of repeat revascularization while at 1 year the revascularization rates remained similar. Similarly, the CORONARY trial showed fewer grafts performed in the off-pump group and higher early revascularization rate at 30 days, but at 1 year the revascularization rates were no longer different (12,19). A large meta-analysis of RCTs by Deppe et al. (3) showed increased early (30 days) revascularization in the off-pump group (Table 4).
Full table
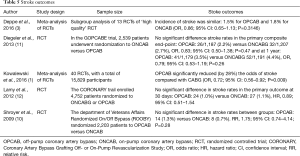
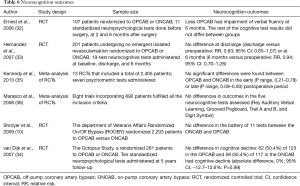
Stroke and neurocognitive outcomes
Cerebral stroke is a major complication after coronary artery bypass grafting that increases mortality, morbidity and cost (27). Minimization of aortic manipulation (28) and avoidance of the extracorporeal circuit (29) reduce the risk stroke and cerebral embolization respectively. Therefore, OPCAB should offer better outcomes in this respect. The most prominent off-pump versus on-pump trials to date failed to show a reduction of stroke rates with use of OPCAB (10-12). Deppe et al. in the subgroup meta-analysis of 13 trials found no difference in stroke rates between OPCAB or ONCAB (3). However, the recent meta-analysis by Kowalewski et al. on 40 RCTs found OPCAB to be associated with a significant 28% reduction in odds of cerebral stroke (OR, 0.72; 95% CI: 0.56–0.92; P=0.009; I2=0%) (1).
Several studies suggested neurocognition to be more related to aortic manipulation rather the use of extracorporeal circulation (30,31). The ROOBY trial demonstrated no difference in neurophysiological outcomes between off or on-pump groups (10). Similarly, three other randomized trials (32-34) and two systematic reviews of RCTs (35,36) failed to show any benefit with OPCAB in terms of neurocognitive function (Tables 5,6).
Full table
Full table
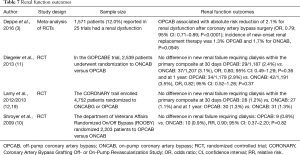
Postoperative renal dysfunction
The ROOBY trial found no significant difference between OPCAB and ONCAB, in terms of renal failure requiring dialysis (10). The CORONARY trial found the use of OPCAB to significantly reduce acute kidney injury (28.0% vs. 32.1%; RR, 0.87; 95% CI: 0.80–0.96; P=0.01) (12). The GOPCABE trial found no difference between off-pump or on-pump in new renal-replacement therapy required at 30- or 1-year which was part of the primary composite endpoint (11). In a subgroup meta-analysis of 1,571 patients from 25 trials, Deppe et al. found OPCAB to reduce the absolute risk of renal dysfunction by 2.1% (OR, 0.79; 95% CI: 0.71–0.89; P<0.0001) but no difference in the new onset of renal replacement (3) (Table 7).
Full table
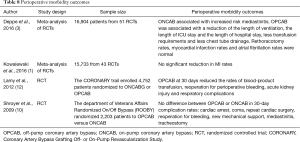
Other perioperative complications
The current literature debating about perioperative morbidity related to OPCAB or ONCAB focuses on the following clinical outcomes: low cardiac output, perioperative myocardial infarction, infection rates, bleeding and reintervention rates, length of stay, ventilation time and rates of atrial fibrillation. The ROOBY trial demonstrated no difference in reoperation for bleeding, new mechanical support or mediastinitis (10). In the CORONARY trial, the use of OPCAB reduced perioperative transfusions (50.7% vs. 63.3%; RR, 0.80; 95% CI: 0.75–0.85; P<0.001), reoperation for perioperative bleeding (1.4% vs. 2.4%; RR, 0.61; 95% CI: 0.40–0.93; P=0.02), acute kidney injury (28.0% vs. 32.1%; RR, 0.87; 95% CI: 0.80–0.96; P=0.01), and respiratory complications (5.9% vs. 7.5%; RR, 0.79; 95% CI: 0.63–0.98; P=0.03). Two large meta-analyses of RCTs (1,3) found no difference in myocardial infraction rates between ONCAB or OPCAB. In the meta-analysis by Deppe et al. (3), the incidence of low cardiac output and infection were reduced with use off-pump. Furthermore, the number of patients needing transfusion and the chest tube drainage was significantly reduced in the in the off-pump group, but with no difference in re-thoracotomy rates. In the same meta-analysis (3) there was no difference in atrial fibrillation rates between off-pump versus on-pump, contrary to a smaller, previous meta-analysis of RCTs (37) (Table 8).
Full table
High-risk patients
Most of the available evidence for the high risk patient is focused on several high risk groups: left ventricular dysfunction, renal impairment, left main stem disease, old age, stroke, re-do coronary artery bypass grafting, chronic lung disease, emergency surgery and patients with an European system for cardiac operative risk evaluation (EuroSCORE) of >5 (1). In a RCT of 411 high risk patients (EuroSCORE ≥6), OPCAB was found to reduce mortality and morbidity at 30 days (38). Similarly, a smaller RCT by Hlavicka et al. of 206 patients with EuroSCORE ≥6 found a significantly higher incidence of the combined endpoint (all-cause deaths, stroke, myocardial infarction, or renal failure requiring new haemodialysis) in the ONCAB group at 30 days, while at 1 year there was no significant difference between the two groups (39). In the large meta-analysis of RCTs by Kowalewski et al., the main finding was a significant linear relationship between the risk profile and the beneficial effect of OPCAB (1). A randomized study of patients with preoperative non-dialysis-dependent renal insufficiency by Sajja et al. demonstrated that ONCAB adversely affects renal function compared to the off-pump group (40). Two large RCTs on elderly populations failed to show any mortality or morbidity benefit with use OPCAB (11,23). Masoumi et al. reported significantly lower rates of mortality, morbidity, balloon-pump support, inotropic usage, gastrointestinal bleeding, renal dysfunction, reintubation, intensive care and hospital stay reported patient with a poor ejection fraction (≤35%) in patients randomly assigned to OPCAB or ONCAB (41). In the RCT by Fattouch et al. patients undergoing emergency OPCAB had a reduction in early mortality (14) while the late mortality did not differ compared to conventional surgery (42). Several retrospective studies found a benefit in using off-pump techniques in other high risk groups such as: females (43) or reoperative coronary artery bypass grafting (44). Overall, the weight of randomized data for the high risk patient undergoing coronary surgery shows a clear benefit from OPCAB as demonstrated by other landmark retrospective studies (45) or large meta-analyses of non-randomized trials (46) (Table 9).

Full table
Conclusions
The current evidence synthesised from RCTs demonstrates comparable early and late survival for both off-pump and conventional coronary artery bypass grafting. However, patients undergoing OPCAB grafting appear to have fewer coronary anastomoses and increased repeat revascularisation rates. Some studies suggest poorer vein graft patency but comparable midterm arterial conduit patency. In contrast, a long term follow-up study found no difference between venous and arterial graft patency pooled randomised data shows a reduction in stroke rates with use off-pump techniques. OPCAB grafting seems to reduce postoperative renal dysfunction, bleeding, transfusion requirements and respiratory complications while perioperative myocardial infarction rates remain unchanged. The high risk patient groups seem to benefit from off-pump coronary surgery.
Acknowledgements
The study was supported by the British Heart Foundation and the NIHR Bristol Cardiovascular Biomedical Research Unit.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kowalewski M, Pawliszak W, Malvindi PG, et al. Off-pump coronary artery bypass grafting improves short-term outcomes in high-risk patients compared with on-pump coronary artery bypass grafting: Meta-analysis. J Thorac Cardiovasc Surg 2016;151:60-77.e1-58.
- Taggart DP. Replacement of the aortic root with a pulmonary autograft. N Engl J Med 1994;330:1615-6. [Crossref] [PubMed]
- Deppe AC, Arbash W, Kuhn EW, et al. Current evidence of coronary artery bypass grafting off-pump versus on-pump: a systematic review with meta-analysis of over 16,900 patients investigated in randomized controlled trials†. Eur J Cardiothorac Surg 2016;49:1031-41; discussion 1041. [Crossref] [PubMed]
- Greason KL, Sundt Iii TM. Myocardial Revascularization without Cardiopulmonary Bypass. In: Cohn LH. editor. Cardiac Surgery in the Adult. 4th edition. New York: The McGraw-Hill Companies, 2012:505-22.
- Trapp WG, Bisarya R. Placement of coronary artery bypass graft without pump oxygenator. Ann Thorac Surg 1975;19:1-9. [Crossref] [PubMed]
- Buffolo E, Andrade JC, Succi JE, et al. Direct revascularization of the myocardium without extracorporeal circulation. Description of the technic and preliminary results. Arq Bras Cardiol 1982;38:365-73. [PubMed]
- Ankeney JL. Off-pump bypass surgery: the early experience, 1969-1985. Tex Heart Inst J 2004;31:210-3. [PubMed]
- Bakaeen FG, Shroyer AL, Gammie JS, et al. Trends in use of off-pump coronary artery bypass grafting: Results from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. J Thorac Cardiovasc Surg 2014;148:856-3, 864.e1; discussion 863-4.
- Hattler B, Messenger JC, Shroyer AL, et al. Off-Pump coronary artery bypass surgery is associated with worse arterial and saphenous vein graft patency and less effective revascularization: Results from the Veterans Affairs Randomized On/Off Bypass (ROOBY) trial. Circulation 2012;125:2827-35. [Crossref] [PubMed]
- Shroyer AL, Grover FL, Hattler B, et al. On-pump versus off-pump coronary-artery bypass surgery. N Engl J Med 2009;361:1827-37. [Crossref] [PubMed]
- Diegeler A, Börgermann J, Kappert U, et al. Off-pump versus on-pump coronary-artery bypass grafting in elderly patients. N Engl J Med 2013;368:1189-98. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Off-pump or on-pump coronary-artery bypass grafting at 30 days. N Engl J Med 2012;366:1489-97. [Crossref] [PubMed]
- Taggart DP, Altman DG, Gray AM, et al. Effects of on-pump and off-pump surgery in the Arterial Revascularization Trial. Eur J Cardiothorac Surg 2015;47:1059-65. [Crossref] [PubMed]
- Fattouch K, Guccione F, Dioguardi P, et al. Off-pump versus on-pump myocardial revascularization in patients with ST-segment elevation myocardial infarction: a randomized trial. J Thorac Cardiovasc Surg 2009;137:650-6; discussion 656-7. [Crossref] [PubMed]
- Møller CH, Penninga L, Wetterslev J, et al. Off-pump versus on-pump coronary artery bypass grafting for ischaemic heart disease. Cochrane Database Syst Rev 2012.CD007224. [PubMed]
- Angelini GD, Taylor FC, Reeves BC, et al. Early and midterm outcome after off-pump and on-pump surgery in Beating Heart Against Cardioplegic Arrest Studies (BHACAS 1 and 2): a pooled analysis of two randomised controlled trials. Lancet 2002;359:1194-9. [Crossref] [PubMed]
- Angelini GD, Culliford L, Smith DK, et al. Effects of on- and off-pump coronary artery surgery on graft patency, survival, and health-related quality of life: long-term follow-up of 2 randomized controlled trials. J Thorac Cardiovasc Surg 2009;137:295-303. [Crossref] [PubMed]
- Luo T, Ni Y. Short-term and Long-term Postoperative Safety of Off-Pump versus On-Pump Coronary Artery Bypass Grafting for Coronary Heart Disease: A Meta-analysis for Randomized Controlled Trials. Thorac Cardiovasc Surg 2015;63:319-27. [Crossref] [PubMed]
- Lamy A, Devereaux PJ, Prabhakaran D, et al. Effects of off-pump and on-pump coronary-artery bypass grafting at 1 year. N Engl J Med 2013;368:1179-88. [Crossref] [PubMed]
- Magee MJ, Alexander JH, Hafley G, et al. Coronary artery bypass graft failure after on-pump and off-pump coronary artery bypass: findings from PREVENT IV. Ann Thorac Surg 2008;85:494-9; discussion 499-500. [Crossref] [PubMed]
- Lingaas PS, Hol PK, Lundblad R, et al. Clinical and radiologic outcome of off-pump coronary surgery at 12 months follow-up: a prospective randomized trial. Ann Thorac Surg 2006;81:2089-95. [Crossref] [PubMed]
- Khan NE, De Souza A, Mister R, et al. A randomized comparison of off-pump and on-pump multivessel coronary-artery bypass surgery. N Engl J Med 2004;350:21-8. [Crossref] [PubMed]
- Houlind K, Kjeldsen BJ, Madsen SN, et al. On-pump versus off-pump coronary artery bypass surgery in elderly patients: results from the Danish on-pump versus off-pump randomization study. Circulation 2012;125:2431-9. [Crossref] [PubMed]
- Widimsky P, Straka Z, Stros P, et al. One-year coronary bypass graft patency: a randomized comparison between off-pump and on-pump surgery angiographic results of the PRAGUE-4 trial. Circulation 2004;110:3418-23. [Crossref] [PubMed]
- Zhang B, Zhou J, Li H, et al. Comparison of graft patency between off-pump and on-pump coronary artery bypass grafting: an updated meta-analysis. Ann Thorac Surg 2014;97:1335-41. [Crossref] [PubMed]
- Puskas JD, Williams WH, Mahoney EM, et al. Off-pump vs conventional coronary artery bypass grafting: early and 1-year graft patency, cost, and quality-of-life outcomes: a randomized trial. JAMA 2004;291:1841-9. [Crossref] [PubMed]
- Puskas JD, Winston AD, Wright CE, et al. Stroke after coronary artery operation: incidence, correlates, outcome, and cost. Ann Thorac Surg 2000;69:1053-6. [Crossref] [PubMed]
- Calafiore AM, Di Mauro M, Teodori G, et al. Impact of aortic manipulation on incidence of cerebrovascular accidents after surgical myocardial revascularization. Ann Thorac Surg 2002;73:1387-93. [Crossref] [PubMed]
- Bowles BJ, Lee JD, Dang CR, et al. Coronary artery bypass performed without the use of cardiopulmonary bypass is associated with reduced cerebral microemboli and improved clinical results. Chest 2001;119:25-30. [Crossref] [PubMed]
- Hammon JW, Stump DA, Butterworth JF, et al. Single crossclamp improves 6-month cognitive outcome in high-risk coronary bypass patients: the effect of reduced aortic manipulation. J Thorac Cardiovasc Surg 2006;131:114-21. [Crossref] [PubMed]
- Hammon JW, Stump DA, Butterworth JF, et al. Coronary artery bypass grafting with single cross-clamp results in fewer persistent neuropsychological deficits than multiple clamp or off-pump coronary artery bypass grafting. Ann Thorac Surg 2007;84:1174-8; discussion 1178-9. [Crossref] [PubMed]
- Ernest CS, Worcester MU, Tatoulis J, et al. Neurocognitive outcomes in off-pump versus on-pump bypass surgery: a randomized controlled trial. Ann Thorac Surg 2006;81:2105-14. [Crossref] [PubMed]
- Hernandez F Jr, Brown JR, Likosky DS, et al. Neurocognitive outcomes of off-pump versus on-pump coronary artery bypass: a prospective randomized controlled trial. Ann Thorac Surg 2007;84:1897-903. [Crossref] [PubMed]
- van Dijk D, Spoor M, Hijman R, et al. Cognitive and cardiac outcomes 5 years after off-pump vs on-pump coronary artery bypass graft surgery. JAMA 2007;297:701-8. [Crossref] [PubMed]
- Kennedy ED, Choy KC, Alston RP, et al. Cognitive outcome after on- and off-pump coronary artery bypass grafting surgery: a systematic review and meta-analysis. J Cardiothorac Vasc Anesth 2013;27:253-65. [Crossref] [PubMed]
- Marasco SF, Sharwood LN, Abramson MJ. No improvement in neurocognitive outcomes after off-pump versus on-pump coronary revascularisation: a meta-analysis. Eur J Cardiothorac Surg 2008;33:961-70. [Crossref] [PubMed]
- Cheng DC, Bainbridge D, Martin JE, et al. Does off-pump coronary artery bypass reduce mortality, morbidity, and resource utilization when compared with conventional coronary artery bypass? A meta-analysis of randomized trials. Anesthesiology 2005;102:188-203. [Crossref] [PubMed]
- Lemma MG, Coscioni E, Tritto FP, et al. On-pump versus off-pump coronary artery bypass surgery in high-risk patients: operative results of a prospective randomized trial (on-off study). J Thorac Cardiovasc Surg 2012;143:625-31. [Crossref] [PubMed]
- Hlavicka J, Straka Z, Jelinek S, et al. Off-pump versus on-pump coronary artery bypass grafting surgery in high-risk patients: PRAGUE-6 trial at 30 days and 1 year. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub 2016;160:263-70. [Crossref] [PubMed]
- Sajja LR, Mannam G, Chakravarthi RM, et al. Coronary artery bypass grafting with or without cardiopulmonary bypass in patients with preoperative non-dialysis dependent renal insufficiency: a randomized study. J Thorac Cardiovasc Surg 2007;133:378-88. [Crossref] [PubMed]
- Masoumi M, Saidi MR, Rostami F, et al. Off-pump coronary artery bypass grafting in left ventricular dysfunction. Asian Cardiovasc Thorac Ann 2008;16:16-20. [Crossref] [PubMed]
- Fattouch K, Runza G, Moscarelli M, et al. Graft patency and late outcomes for patients with ST-segment elevation myocardial infarction who underwent coronary surgery. Perfusion 2011;26:401-8. [Crossref] [PubMed]
- Puskas JD, Kilgo PD, Kutner M, et al. Off-pump techniques disproportionately benefit women and narrow the gender disparity in outcomes after coronary artery bypass surgery. Circulation 2007;116:I192-9. [Crossref] [PubMed]
- Mishra YK, Collison SP, Malhotra R, et al. Ten-year experience with single-vessel and multivessel reoperative off-pump coronary artery bypass grafting. J Thorac Cardiovasc Surg 2008;135:527-32. [Crossref] [PubMed]
- Puskas JD, Thourani VH, Kilgo P, et al. Off-pump coronary artery bypass disproportionately benefits high-risk patients. Ann Thorac Surg 2009;88:1142-7. [Crossref] [PubMed]
- Kuss O, von Salviati B, Börgermann J. Off-pump versus on-pump coronary artery bypass grafting: a systematic review and meta-analysis of propensity score analyses. J Thorac Cardiovasc Surg 2010;140:829-35, 835.e1-13.


