Colobronchial fistula: the pathogenesis, clinical presentations, diagnosis and treatment
Introduction
The fistula between respiratory system and digestive tract is not uncommon in clinic. Owning to the different anatomy and physiological function of respiratory system and digestive tract, the fistula between these two systems usually cause severe clinical outcome and need to be diagnosed and treated in time. The most common fistula between respiratory system and digestive tract is tracheal or bronchial esophageal fistula. However, colobronchial fistula (CBF) [or colono pleuro bronchial fistula (CPBF)] is rare in clinic (1-5). Only 36 cases were reported from January 1960 to August 2016 in literature. So far, there is little information for this disease. CBF usually has complicated clinical presentations and is easily delayed. So, it is necessary to systemically study this disease to further improve the diagnosis and treatment of this disease.
In this study, the data from a total of 37 cases, one treated in our institute and the others reported in literature, were summarized and analyzed in order to get a comprehensive understanding of this rare disease.
Methods
A case of CBF in our institute
A 41-year-old man was admitted to our department with a one month history of productive cough with foul smelling sputum. He suffered a traffic accident 10 years ago where he had left ribs fracture. The patient was discharged after treatment in local hospital. Four years ago, he felt abdominal pain and distension without any causes. An acute appendicitis was diagnosed and an appendectomy was performed in local hospital. No obvious intestinal obstruction was found during operation. After operation, the patient recovered well until the 8th day a paroxysmal cough with yellow sputum appeared. The patient was diagnosed as pneumonia and was discharged after treatment with antibiotics. But since then, the patient had occasional cough with sputum and had lost 10 kg in weight. One month ago, he felt dyspnoea and severe productive cough with foul smelling sputum, and some fecal material appeared in the sputum.
After admission, a chest X-ray revealed an infiltration in the left lower lobe. Barium meal and follow-through study followed by a computed tomography (CT) scan with multiplanar reconstruction showed consolidation in the left lower lobe, left pleural adhesions, the splenic flexure herniated into left chest cavity and there was a suspected connection exist between the splenic flexure and the left lower lobe (Figure 1A,B). At bronchoscopy, mucopurulent secretions were observed from the left lobe. In order to avoiding the barium was flushed into bronchus, a colonoscopy was performed instead of the barium enema. At colonoscopy, there was a dead-end found in the splenic flexure and a fistula was found in this dead-end (Figure 1C), which further confirmed the fistula existed between colon and bronchus.

A left exploratory thoracotomy was performed. It was found that there was a 5 cm rupture in the left diaphragm, the splenic flexure herniated into left chest cavity and tightly adhered to left lower lobe. A fistula existed between lower lobe and the splenic flexure. The left low lobe was consolidated and couldn’t expend after recruitment. A left lower lobectomy was performed and the fistula was removed. The colon was sutured and the left diaphragm was repaired. The patient fully recovered and was discharged from hospital 14 days later. He was uneventful after 5 years follow up. The review of the patient’s information was approved by the review board of Tangdu Hospital.
Clinical data
By searching in PubMed database, China Academic Journal Network Publishing Database and using Google research engine (restricted in English and Chinese papers), the published CBF cases (36 cases) from January 1960 to August 2016 were collected. All clinical data from the total of 31 cases (age: 11–73 years; male vs. female: 19 vs. 18 cases) were reviewed and analyzed. The etiology, characteristic clinical presentation, diagnostic and treatments methods, and outcomes were summarized.
Results
The causes of CBF
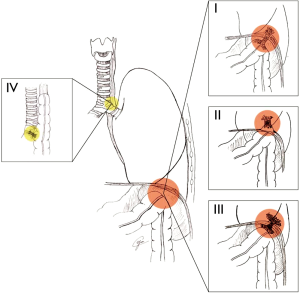
The causes behind CBF included Crohn’s disease, postoperative intraperitoneal adhesion, traumatic and un-traumatic diaphragmatic hernia, pulmonary infection or abscess, colonic malignancy, colonic interposition, radiation, hyperthermic intraperitoneal chemotherapy (HIPEC), diaphragmatic mesh repair, pulmonary tuberculosis and pyonephrosis (Table 1). Based on the anatomical location of fistula and different causes, all the CBF cases were classified into four different types. Type I, CBF secondary to the adhesion among colon, diaphragm and lung (20 cases) (1,6-17,19-22,29): both the colon and lung directly adhere to diaphragm and the fistula forms between colon and lung through diaphragm; type II, CBF secondary to diaphragmatic hernia (8 cases) (2,3,17,18,23,24): the colon goes through diaphragm to form diaphragmatic hernia, directly adheres to lung tissue and forms fistula; type III, CBF secondary to sub diaphragmatic abscess or empyema (7 cases) (4,5,25-28,30): the colon and lung tissue fistula connect indirectly through the sub diaphragmatic or pleural abscess; type VI, CBF secondary to colon interposition (2 cases, Figure 2) (31,32).
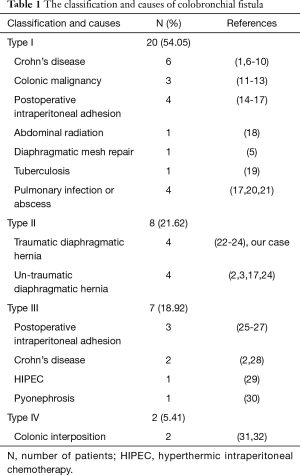
Full table
For type I cases, the causes included Crohn’s disease (6 cases), colonic malignancy (3 cases), postoperative intraperitoneal adhesion (4 cases), abdominal radiation (1 case), diaphragmatic mesh repair (1 case), tuberculosis (1 case) and pulmonary infection or abscess (4 cases, Table 1). For type II cases, traumatic (4 cases) and un-traumatic (4 cases) diaphragmatic hernias were the causes (Table 1). For type III cases, the causes included postoperative intraperitoneal adhesion (3 cases), Crohn’s disease (2 case), HIPEC (1 case) and pyonephrosis (1 case, Table 1). For type IV, all 2 cases accepted colonic interposition (Table 1). There were 30 cases (2,4,6-10,12-14,16,17,19-21,23-32) with the left side fistula and 7 cases (1,3,5,11,15,18,22) with the right side fistula.
The clinical presentations of CBF
The clinical presentations of CBF included productive cough with (78.38%) or without (10.81%) foul smelling sputum, weight loss (32.43%), fever (32.43%), chest pain (27.03%), dyspnoea (21.62%), hemoptysis (16.22%), dysphagia or diarrhoea (13.51%), hematemesis or melena (5.41%), and change of bowel habit (2.70%, Table 2).
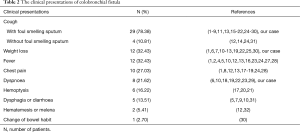
Full table
The methods to confirm the diagnosis of CBF
The methods that finally confirmed the diagnosis of CBF included barium enema or water-soluble contrast enema study (67.57%), CT scan/with multiplanar reconstruction (16.22%), barium swallow (10.81%), flexible sigmoidoscopy or colonoscopy (2.70%), and postmortem examination (2.70%, Table 3).
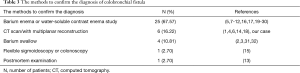
Full table
The treatment and outcome of CBF
The treatment included etiological treatment, nutrition supporting treatment and surgery. Among 37 patients, 35 patients (94.59%) accepted the surgical interventions. Among these 35 patients, 33 patients accepted the resection of the fistula, the related colon with (14 cases) or without (19 cases) lung tissue, and repair of the diaphragm; 2 patients accepted colostomy because of poor condition. For the other 2 patients, 1 patient (7) refused consent for the operation and 1 patient (31) accepted esophageal stent implanting. The follow-up results can be got from 31 out of 37 patients (83.78%). 26 patients were discharged from the hospital with a good recovery, but 5 patients died in 1 month after treatment. The reasons of death include uncontrolled infection (5,23,30), carcinoma (13) and pulmonary embolus (24).
Discussion
Owning to the complex etiology and the complicated clinical presentations of CBF, this disease is not fully understood and easily delayed in clinic. Therefore, it is necessary to carefully review and summary these 37 cases which have been reported in our institute and in literature for further understanding this disease.
The causes of CBF are complicated. Anything which may induce the direct or indirect connection between colon and lung tissue may result in CBF. In order to easily understand the pathogeneses of CBF, we developed a classification system based on the anatomical location and causes of fistula (Figure 2). For type I cases, Crohn’s diseases, pulmonary infection or abscess, and iatrogenic intraperitoneal adhesions are the main reasons. The other reasons include colonic cancer invasion to diaphragma and pulmonary tuberculosis induced adhesion. For type II cases, diaphragm hernia increases the incidence of this fistula formation between colon and bronchus. For type III cases, the spontaneous rupture of a subphrenic abscess which goes into adjacent colon, penetrates the diaphragm into the pleural cavity and further into the adherent lung or vice versa, may be the cause. For type IV, it should be consider a complication of colonic interposition. It is worth noting that much more attention should be paid to patients with a history of Crohn’s diseases and abdominal surgical or radiological interventions. Probably, Crohn’s diseases and abdominal iatrogenic interventions may increase the incidence of abdominal organ adhesions or abscess formation. Although the left side CBF is more commonly reported because of the existence of liver in the right upper quadrant of the abdomen, there are still 18.92% patients with right side CBF. The abdominal surgical intervention in the right side such as hepatic resection, right nephrectomy and right diaphragmatic surgery may increase the risk of right CBF.
The clinical presentations of CBF are various because they refer to both the respiratory system and digestive system (Table 2). But for CBF, the respiratory symptoms such as cough, chest pain, dyspnoea and hemoptysis, are much more common than digestive symptoms such as diarrhoea, hematemesis and change of bowel habit. The most characteristic symptom for CBF is productive cough with foul smelling sputum, which should be paid much more attention and raise the suspicion for this disease.
In clinic, it usually takes a long time to confirm the diagnosis of CBF because of the complicated pathogenesis and various clinical presentations. Besides routine laboratory tests and chest radiography, some specific examinations should be performed to confirm the existence of fistula (Table 3). The barium enema or water-soluble contrast enema study has a unique role in diagnosis of CBF. Most of the patients can be detected the existence of fistula by using barium enema or water-soluble contrast enema study. Considering the potential risk of barium or water soluble contrast spillage into the fistulous tract or the lungs, which could be a source of infection and may not be easily removed, a CT scan with multiplanar reconstruction has been widely used to visualize the fistula recently. By using CT scan with multiplanar reconstruction instead of barium enema, 16.22% cases had been confirmed. The other valuable diagnostic methods include flexible colonoscopy and postmortem examinations. A combination of radiological and endoscopic investigations is more helpful to obtain a clear and confirmed diagnosis for CBF. Sputum culture with intestinal flora positive, such as Escbericbia coli, is helpful for the suspicion of CBF (14).
The treatment of CBF is not easy. Owning to the infection and fasting, the patients are usually in very poor condition. Therefore, the antibiotic treatment and total parenteral nutrition are essential, which may control the infection and provide a relative better condition for further surgical treatment. At the same time, Specific treatment aiming to different causes should be performed. For example, infliximab has been successfully used to treat a Crohn’s disease induced CBF, which totally controlled the progress of Crohn’s disease, resulted in dramatic clinical improvement and simplified surgical management (1).
Surgery may be the only way to cure the CBF. The basic surgical procedures include the resection of fistula, the related colon and the lung tissue. If the CBF is nonmalignant, the surgeon should try to resect the lung and colon as little as possible. Our study implied that 57.6% (19/33) patients did not need the lung tissue resection. If the CBF is malignant, the surgeon should try to remove the tumor, dissect the lymph nodes, resect the fistula, and reconstruct the respiratory system and digestive tract at the same time. But it is very challengeable for the surgeon. Even though medicine has been developed quickly, the mortality of CBF isn’t reduced recently. There were 3 (13,24,30) out of 23 patients died of CBF from 1960 to 2000, and 2 (5,23) out of 14 patients died of CBF from 2000 to 2012, which means much more efforts should be made to improve the treatment of CBF in future.
There is a limitation in this study. Owning to the low morbidity of this disease, most of the data in this study comes from the literature. Some important information may be not reported because the authors may concentrate on different aspect in their own publications. But, through this overall study, a panoramic view of CBF can be provided, which is helpful for the thoracic and general surgeons to understand and treat this disease.
In conclusion, CBF is a rare disease with complicated clinical presentations. Productive cough with foul smelling sputum is the most important symptom. Radiological investigations such as barium enema and/or CT scan with multiplanar reconstruction, combined with endoscopic investigations, are valuable for the diagnosis of this disease. Surgical treatment based on the etiological treatments may be the best choice for the patients.
Acknowledgements
We really appreciate Ms. Yiming Chun (University of Toronto) for drawing the illustration and Prof. Mingyao Liu (MD, Msc, University of Toronto) for his critical reading and comments on this manuscript.
Funding: The project was partially supported by Natural Science Basic Research Plan in Shaanxi Province of China (Program No. 2016JM8087).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The review of the patient’s information was approved by the review board of Tangdu Hospital.
References
- Mercadal NR, Wiebke EA. Recurrent pneumonia and colobronchial fistula from Crohn’s disease: Infliximab alters and simplifies surgical management. Ann Gastroenterol 2012;25:361-4.
- Sahu SK, Singh NK, Singh S, et al. Colobronchial fistula: a rare cause of chronic cough. Natl Med J India 2011;24:345-6.
- Kumar M, Chandra A, Kumar S. Right-sided diaphragmatic hernia complicated with broncho-pleuro-colonic fistula presenting as fecoptysis. BMJ Case Rep 2011;2011. pii: bcr0620114296.
- Badiani S, Bowley D, Steyn R, et al. A very 'tickly' cough. Colorectal Dis 2011;13:e87-89. [Crossref]
- Mohanraj MM, Mayer D, Harkin TJ, et al. Colo-bronchial Fistula as a rare complication of diaphragmatic mesh repair. Am J Respir Crit Care Med 2010.A5826.
- Alameel T, Maclean DA, Macdougall R. Colobronchial fistula presenting with persistent pneumonia in a patient with Crohn's disease: a case report. Cases J 2009;2:9114. [Crossref]
- Mera A, Sugimoto M, Fukuda K, et al. Crohn's disease associated with colo-bronchial fistula. Intern Med 1996;35:957-60. [Crossref]
- Karmy-Jones R, Chagpar A, Vallieres E, et al. Colobronchial fistula due to Crohn's disease. Ann Thorac Surg 1995;60:446-8. [Crossref]
- Singh D, Cole JC, Cali RL, et al. Colobronchial fistula: an unusual complication of Crohn's disease. Am J Gastroenterol 1994;89:2250-2.
- Domej W, Kullnig P, Petritsch W, et al. Colobronchial fistula: a rare complication of Crohn's colitis. Am Rev Respir Dis 1990;142:1225-7. [Crossref]
- Savage PJ, Donovan WN, Kilgore TL. Colobronchial fistula in a patient with carcinoma of the colon. South Med J 1982;75:246-7. [Crossref]
- Teicher I, Khan FA, Azueta V, et al. Colopulmonary fistula due to perforating carcinoma of splenic flexure. N Y State J Med 1976;76:944-7.
- Hines DR, Granson PA, Taylor RL. Colo-pleuro-bronchial fistula due to carcinoma of the colon. Ann Thorac Surg 1966;2:594-6. [Crossref]
- Kim SY, Park SH, Lee SS, et al. Diagnosis of colopulmonary fistula by virtual colonoscopy. Gastrointest Endosc 2008;67:769-71. [Crossref]
- Eltzschig HK, Palmer G, Brustowicz R. Colobronchial fistula in a pediatric patient: diagnostic value of isolated single-lung ventilation and intraoperative use of high frequency oscillatory ventilation. Anesth Analg 2002;95:621-3.
- Swerdlow B, Jenkins JG. Anaesthesia for colobronchial fistula. Anaesthesia 1985;40:42-4. [Crossref]
- Zhao QS, Cui GH, Xu JG, et al. The diagnosis and surgical treatment of Bronchopleuro-colonic fistula. Clin Med China 2000;16:714-5.
- Green MH, Gosling SS. Colobronchial Fistula Complicating a Traumatic Right Diaphragmatic Hernia: A Case Report. Eur J Trauma 2006;32:578-81. [Crossref]
- Crofts TJ, Dalrymple JO, Buhrmann JR. Tuberculous bronchocolonic fistula. A case report. S Afr Med J 1978;54:795-6.
- Wang ZH, Zheng CH, Li SY. The diagnosis and treatment of a bronchopleuro-colonic fistula case. People's Military Surgeon 1989;7:30.
- Zheng H, Ge K. Bronchopleuro-colonic fistula: a case report. Med Tianjin 1988;2:70.
- MacKay GC, Howells J, Poon FW. Colobronchial fistula: a late complication of childhood radiotherapy. Brit J Radiol 2006;79:170-2. [Crossref]
- Irving M. Colo-broncho-cutaneous fistula complicating traumatic diaphragmatic rupture. J R Soc Med 2001;94:258-9.
- Carmichael JH, Franklyn PP. Case reports: Bronchopleuro-colonic fistula. Brit J Radiol 1963;36:528-30. [Crossref]
- Ashley S, Corlett SK, Windle R, et al. Colobronchial fistula: a late complication of appendicitis. Thorax 1988;43:420-1. [Crossref]
- Caberwal D, Katz J, Reid R, et al. A case of nephrobronchial and colonobronchial fistula presenting as lung abscess. J Urol 1977;117:371-3.
- Salomon J, Kott I, Levy MJ. Broncho-pleuro-colonic fistula. Isr J Med Sci 1967;3:558-60.
- Flueckiger F, Kullnig P, Melzer G, et al. Colobronchial and gastrocolic fistulas: rare complication of Crohn's disease. Gastrointest Radiol 1990;15:288-90. [Crossref]
- Laterza B, Baratti D, Cozzi G, et al. Colobronchial fistula: an unusual complication after peritonectomy and hyperthermic intra-peritoneal chemotherapy (HIPEC). In Vivo 2009;23:151-3.
- Baker TH, Ali PM. Broncho-pleuro-colonic fistula secondary to pyonephrosis. Br J Urol 1974;46:344. [Crossref]
- Zhao X, Sandhu B, Kiev J. Colobronchial fistula as a rare complication of coloesophageal interposition: a unique treatment with a review of the medical literature. Am Surgeon 2005;71:1058-9.
- Perlmutter DH, Tapper D, Teele RL, et al. Colobronchial fistula as a late complication of coloesophageal interposition. Gastroenterology 1984;86:1570-2.


