First case in China: Onyx for bronchial artery embolization in treatment of refractory massive hemoptysis in one case
Introduction
Massive hemoptysis is a severe, life-threatening illness. Bronchial artery embolization is commonly used to treat massive hemoptysis. In May 2012, we first used a new liquid embolic agent (Onyx) for bronchial artery embolization in treatment of refractory massive hemoptysis in one patient in China and obtained good outcomes. The patient did not experience hemoptysis during a 10-month follow-up.
Summary of disease history
A 72-year-old male patient had a 40-year history of recurrent hemoptysis and purulent sputum. The hemoptysis had become aggravated during the last 4 months. He was hospitalized after 1 day of massive hemoptysis. The volume of hemoptysis was 300 mL within 24 hours prior to admission. Physical examination on admission revealed stable vital signs, a heart rate of 75 beats/minute, blood pressure of 110/70 mmHg, normal respiration, crackles over the bilateral lower lobes, and no lip cyanosis. The patient was placed on strict bed rest and received intensive care; hemocoagulase, pituitrin, tranexamic acid, and phentolamine for hemostasis, and an injected with fresh plasma. He was also subjected to cryoprecipitation for 5 days. However, no obvious clinical changes were observed. The average volume of hemoptysis was 200 mL/day. Chest computed tomography (CT) displayed bronchiectasis in the middle of right lung and bilateral lower lobes. Thus, the patient was subjected to bronchial artery embolization for hemostasis. Preoperative CT angiography revealed that at the level of superior border of the fifth thoracic vertebra, the bronchial artery branched out in the 10-o’clock direction from the right anterior wall of descending aorta with a common trunk of 0.5 cm. The artery diameter at the original site was about 4.0 mm. The artery was divaricated into left and right bronchial arteries, which became thickened and curly and contributed to the blood supply of the lesions in the left and right lungs.
Surgical procedures
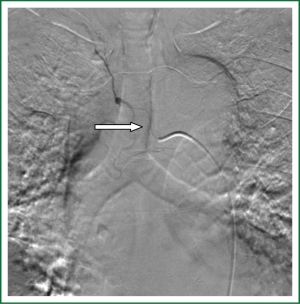
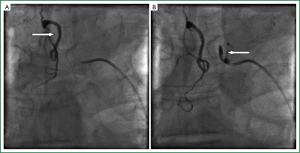
Preoperative examinations revealed no contraindications to bronchial artery embolization. The patient was placed in the supine position and consecutively monitored using an electrocardiogram monitor. A 5-French Cobra microcatheter was placed in the descending aorta through the femoral artery using the Seldinger technique. The bronchial artery was identified coursing in the 10-o’clock direction of the right anterior wall of descending aorta at the level of superior border of the fifth thoracic vertebra and confirmed to be bilateral bronchial artery lesions by angiography. The artery was first embolized with embolic microspheres. The microcatheter was inserted into the opening of the left bronchial artery, which was infused with 30 mL of 700- to 900-µm embolic microspheres (Embosphere microspheres, 10 mL × 3 bottles, BioSphere). However, this procedure was ineffective. Angiography displayed the proximal and distal ends of the left bronchial artery and its branches (Figure 1), suggesting poor effects of the embolic microspheres. We decided to use metal spring coils for embolization. We tried to insert the cobra catheter into the deep part of the left bronchial artery, but this catheter was stuck in the “V”-shaped crotch of the left and right bronchial arteries. The catheter could not be advanced further, despite guidance and adjustment with a guide wire. The cobra catheter was then replaced by 4-French cobra catheter, 5-French RLG catheter and conical catheter. However, these could not be inserted (Figure 2); they entered the superficial part of the artery to only about 0.5 cm, and inadequate space was available for release of the spring coil. To avoid the spring coil ejected from the artery, the surgery was temporarily terminated.


The patient still experienced hemoptysis. The Department of Neurosurgery of our hospital recently introduced a novel liquid embolic agent (Onyx) for cerebrovascular malformations, and its outcomes were good. Onyx can be inserted using a microcatheter and subsequently coagulates within blood vessels. This embolic agent will hopefully resolve the difficulty of bronchial artery embolization in patients with refractory hemoptysis. However, there are few reports on Onyx for bronchial artery embolization in China, and a few outside China. The availability and safety of Onyx for bronchial artery embolization in china remain unclear. With the cooperation of neurosurgeons, we decided to first use Onyx for bronchial artery embolization in the treatment of refractory hemoptysis in a Chinese patient and evaluate its outcome and safety.
The 5-French Cobra microcatheter was first inserted into the opening of the bronchial artery and guided by a hydrophilic guide wire (MirageTM.008; MTI ev3, Irvine, CA, USA). A microcatheter (Marathon; MTI ev3, Irvine, CA, USA) was placed in the distal end of right bronchial artery through the Cobra microcatheter (Figure 3). The hydrophilic guide wire was drawn out. The Marathon was then washed 10 times with physiological saline. Dead space was filled with 0.25 mL of dimethyl sulfoxide liquid. Under fluoroscopic monitoring, Onyx 18 (MTI ev3) was slowly injected at a rate of less than 0.16 mL/min. The Onyx 18 moved to the distal end of the right bronchial artery, showing good dispersion. When Onyx reflux of about 1 cm occurred, the injection was terminated and the microcatheter was immediately pulled out. Angiography displayed that the right bronchial artery was completely embolized by Onyx, and disordered blood vessels were not visible at the distal end, indicating a good outcome (Figure 4). A total of 0.8 mL Onyx was used. By the same method, the Marathon microcatheter was placed in the deep part of the left bronchial artery, and 0.6 mL of Onyx was slowly injected to completely embolize the left bronchial artery. Angiography revealed no disordered blood vessels at the distal end (Figure 4).
The patient was sent to his ward after surgery. Two hours following the surgery, his vital signs were stable: pulse, 88/min; respiration, 20/min; blood pressure, 114/67 mmHg, Spo2, 98%; and absence of fever, chest pain, dizziness, headache, limb numbness, abdominal pain, nausea, vomiting, dyspnea; and embolism symptoms of the liver, kidney, or lower limbs. Hemoptysis did not occur within 48 hours, so the patient was discharged. During the 10-month follow-up, no hemoptysis or adverse reactions occurred.
Discussion
Bronchiectasis is a common cause of recurrent massive hemoptysis, and patients have an imminent risk of drowing. Drugs, artificial pneumoperitoneum, and bronchoscopic balloon blockage can temporarily stop the bleeding. Surgery or bronchial artery embolization is needed for long-time control of the bleeding. The prerequisite for bronchial artery embolization is that 95% of hemoptysis is from the bronchial artery and only 5% is from the pulmonary artery and systemic arteries that supply the lung (1,2). Bronchial artery embolization is a recommended option for patients with recurrent massive hemoptysis who cannot undergo surgery because of extensive foci, an unclear bleeding site, or extensive adhesion between the bleeding focus and the pleura. With rapid visualization by CT angiography and the development of new embolic materials, the outcomes of bronchial artery embolization have improved and the frequency of complications has decreased. Since bronchial artery embolization was first performed in southwest China by the Department of Respiratory Medicine of The First Affiliated Hospital of Chongqing Medical University in China in 1986, more than 500 patients with massive hemoptysis or refractory hemoptysis have been successfully treated by bronchial artery embolization.
The choice of embolic materials is crucial for embolization outcomes. Previously used embolic materials for bronchial artery embolization contained thread, iodinated oil, and gelatin sponges, which were associated with low embolization rates and high recurrence rates. These are seldom used and have been gradually replaced by new materials such as embolic microspheres and metal spring coils. Given the cost of therapy, the patient in this report first underwent embolization with embolic microspheres, but the outcome was not satisfactory because of the widespread blood supply and wide dispersion of the embolic microspheres. Because the particle diameter of embolic microspheres is definite, they exhibit good outcomes in lesions with a small blood supply by a single vessel. Incomplete embolization is attained for lesions with multiple or extensive blood supplies. The immediate outcomes were satisfactory, but a second angiography revealed a blood supply to the small branches of the blood vessels (3). Metal spring coils can embolize commonly used for the embolization of bronchial artery-pulmonary artery fistulas, bronchial artery-pulmonary vein fistulas, and great vessels. When we found that the embolic microspheres were ineffective, we tried to place the spring coils at the proximal end of the target vessels, but this was ineffective. The main reason for the failure of this technique is that the trunk of the target vessel from thoracic aorta was only 0.5 cm and then split into left and right bronchial arteries; the anterior end of the microcatheter became stuck in the “V”-shaped crotch. Because the insertion was superficial, the microcatheter would eject from the target vessels secondary to increased tension. The spring coils would fall into the aorta and embolized the kidney, liver and lower limbs. Thus, spring coils embolization was ineffective.
The introduction of Onyx solves the above-mentioned problem. Onyx was a suspension of ethylenevinyl alcohol copolymer, dimethyl sulfoxide and tantalum powder microparticles (4) and is used as a nonadhesive liquid embolic agent. Ethylenevinyl alcohol copolymer is insoluble in water, but soluble in dimethyl sulfoxide. When it comes into contact with aqueous blood, dimethyl sulfoxide can rapidly disperse in blood. Ethylenevinyl alcohol copolymer can precipitate for the purpose of embolization. Tantalum powder enhances the visibility and control of Onyx. Because Onyx is liquid, it can be injected into the distal end of bronchial artery through a microcatheter, which overcomes the difficulty of spring coil placement. Another advantage of Onyx is that it can be injected slowly and cannot adhere to the wall, demonstrating its high safety. Most importantly, Onyx embolic agent can reach branching capillaries and is associated with a high complete embolic rate and low recurrence rate (5,6). Onyx can permanently embolize 80-µm capillaries with better outcomes than those by microspheres and spring coils. In 2000, Murayama et al. first used Onyx combined with balloon and spring coils in treatment of intracranial aneurysm in a swine model and obtained good outcomes (7). In our case, hemoptysis did not appear within 10-month follow-up, suggesting that Onyx is a promising bronchial artery embolic agent that is worthy of further research and application.
Onyx has many advantages, but also has some shortcomings that limit its clinical application. First, it is expensive at about 5,000 yuan/mL. Onyx is caustic and can induce deformation of commonly used catheters, and a specialized microcatheter (6,000 yuan) is necessary. Thus, most patients cannot financially undergo this treatment, especially when many blood vessels require embolization. Second, the dimethyl sulfoxide in Onyx is associated with a certain degree of vascular toxicity and can induce vasospasm of or damage to vessel walls. A previous study showed that patients experienced postsurgical chest pain (8), which was likely associated with vasospasm. However, as long as the dose and the injection speed of dimethyl sulfoxide are strictly controlled, most patients show good tolerance without obvious adverse reaction, as did the patient reported herein. Third, Onyx is liquid, so reflux would occur. Therefore, the physician should pay close attention to the speed of the injection. The entire process should be fluoroscopically monitored. Once reflux of more than 1 cm appears, the injection should be terminated and the microcatheter should be pulled out.
At present, Onyx is mainly used for arteriovenous malformation of brain, aneurysm and dural arteriovenous fistula. There were no reports on Onyx for bronchial artery embolization in China. This present report describes the first patient who underwent Onyx for bronchial artery embolization in treatment of refractory massive hemoptysis in China. After a Pubmed search of literature from outside China published from 2000 to the present, we retrieved four reports involving more than 50 patients who underwent procedures that utilized Onyx for hemoptysis (8-11). Adamus et al. (9) confirmed that compared with other embolic materials for bronchial artery embolization in the treatment of hemoptysis, Onyx has the following advantages: excellent controllability, rapid embolization and short angiography time (9). Khalil et al. (8) also confirmed the good controllability of Onyx in the treatment of hemoptysis in 15 patients; in particular, when the catheter was difficult to insert, Onyx still can perfectly embolize the distal target vessels with few adverse reactions and high tolerance (8).
In summary, Onyx embolic agent exhibits substantial advantages and may increase the effectiveness and success rate of bronchial artery embolizaiton, benefitting numerous patients suffering from hemoptysis. However, few cases have been reported. Numerous investigations are needed to verify its efficacy and safety in the treatment of hemoptysis, and the indications for its use should be elucidated.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Yoon W, Kim JK, Kim YH, et al. Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: a comprehensive review. Radiographics 2002;22:1395-409. [PubMed]
- Chen GD, Chen SL, Zhao ZW, et al. Clinical values of digital subtraction angiography in patients with bronchiectasis and hemoptysis. Shiyong Yixue Zazhi 2005;21:1419-20.
- Qu GL, Qiang M, Tang H, et al. Selection and application of embolic agent in the treatment of hemoptysis with bronchial artery interventional therapy. Shiyong Zhenduan yu Zhiliao Zazhi 2007;21:164-7.
- Zhang ZQ, Xia Y, Yan Y, et al. Properties of ethylene-vinyl alcohol copolymers and their applications in the field of interventional embolization. Shengwu Yixue Gongcheng Yanjiu 2011;30:109-12.
- Linfante I, Wakhloo AK. Brain aneurysms and arteriovenous malformations: advancements and emerging treatments in endovascular embolization. Stroke 2007;38:1411-7. [PubMed]
- Pierot L, Januel AC, Herbreteau D, et al. Endovascular treatment of brain arteriovenous malformations using onyx: results of a prospective, multicenter study. J Neuroradiol 2009;36:147-52. [PubMed]
- Murayama Y, Viñuela F, Tateshima S, et al. Endovascular treatment of experimental aneurysms by use of a combination of liquid embolic agents and protective devices. AJNR Am J Neuroradiol 2000;21:1726-35. [PubMed]
- Khalil A, Fartoukh M, Bazot M, et al. Systemic arterial embolization in patients with hemoptysis: initial experience with ethylene vinyl alcohol copolymer in 15 cases. AJR Am J Roentgenol 2010;194:W104-10. [PubMed]
- Adamus Nürnberg R, Uder Erlangen M, Kleinschmidt T, et al. Embolization of acute abdominal and thoracic hemorrhages with ethylene vinyl alcohol copolymer (Onyx): initial experiences with arteries of the body trunk. Rofo 2010;182:900-4. [PubMed]
- Bommart S, Bourdin A, Giroux MF, et al. Transarterial ethylene vinyl alcohol copolymer visualization and penetration after embolization of life-threatening hemoptysis: technical and clinical outcomes. Cardiovasc Intervent Radiol 2012;35:668-75. [PubMed]
- Pierce G, Ahuja C, Chadha M. Case report: Complex internal mammary to pulmonary artery fistula as a cause of hemoptysis in tuberculosis: Diagnosis and endovascular management using ethylene vinyl alcohol copolymer (Onyx). Indian J Radiol Imaging 2011;21:10-2. [PubMed]


