|
Review Article
Effect of upper extremity exercise in people with COPD
Ganesan Kathiresan1, Senthil Kumar Jeyaraman2, Jayachandran Jaganathan3
1School of Therapeutic sciences, Masterskill University College, Malaysia; 2School of Therapeutic sciences, Masterskill University College, Malaysia; 3Wrexham Maelor Hospital - North East Wales NHS Trust, Wxeham, Wales
Corresponding author: Ganesan Kathiresan, lecturer. G8, Jalan Kemacahaya 11, Taman Kemacahaya, Batu 9, Cheras 43200, Selangor, Malaysia. Tel: 603-9080 5888; Fax: 603-9080 1995. Email: kathiresan@masterskill.edu.my.
|
|
Abstract
Background: Exercise for people with COPD has focused on leg training, such as walking and cycling. The role and effectiveness of arm training has not been investigated in detail. This review was undertaken to examine the literature for the effectiveness of upper extremity exercise on arm exercise capacity and arm strength in people with COPD.
Methods: Trials relating to arm endurance and strength training in COPD were located by searching electronic databases and screening the reference lists of pertinent articles. Where possible, effect sizes and 95% CI were determined and meta-analysis used.
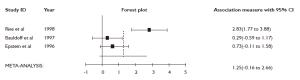
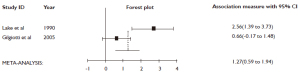
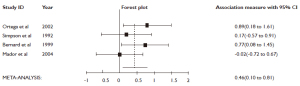
Results: The search strategy yielded 24 articles. Unsupported arm training improved arm endurance capacity (standard mean difference [SMD] =1.25; 95% CI=0.16 to 2.66) and was the optimal mode of arm endurance training. Combined unsupported and supported arm training was also found to have a large positive effect on peak arm exercise capacity (SMD=1.27; 95% CI=0.59 to 1.94). In addition arm strength training produced moderate improvements in arm strength (SMD=0.46; 95% CI=0.10 to 0.81).
Conclusion: This review suggests that in the short term, arm endurance training improves arm exercise capacity and arm strength training improves arm strength. Further research is required, in people with COPD, to investigate the long-term effects of arm training.
Key words
chronic obstructive pulmonary disease; upper extremity exercise
J Thorac Dis 2010;2:223-236. DOI: 10.3978/j.issn.2072-1439.2010.11.4
|
|
Introduction and Purpose
Chronic obstructive pulmonary disease (COPD) the commonest pulmonary condition and it is the major cause of morbidity and mortality among pulmonary patients ( 1). COPD is characterised by airflow limitation that is progressive and not fully reversible ( 2). Worldwide, COPD is recognised as a major public health problem, being a leading cause of morbidity and mortality that is projected to rank fifth in the burden of disease by the year 2020 ( 3). Exercise intolerance is one of the most distressing consequences of COPD. it not only occurs in performing lower body tasks but also manifested during arm activities. A number of studies have confirmed that people with COPD have reduced arm exercise capacity ( 4, 5) and frequently experience marked dyspnea and fatigue during the performance of arm tasks important for daily living ( 5-7). Ventilatory factors underlie the limitations to arm exercise in people with COPD ( 4, 8-10). During arm exercise, the accessory muscles of respiration are required for the arm task and may not be able to contribute to breathing ( 5, 7). There is a resultant shift in respiratory load to the mechanically disadvantaged diaphragm, which results in thoracoabdominal dyssynchrony and severe dyspnea ( 4, 5). In addition, since the muscles that move the arms and stabilise the trunk are attached to the rib cage, this increases chest wall impedance, which limits the ability to increase tidal volume during arm activities ( 4, 11). It is these impairments in ventilatory mechanics which result in the termination of arm exercise at low workloads for people with COPD compared to healthy subjects ( 12). Traditionally, exercise for people with COPD has concentrated on lower limb training, with clinical improvements in lower limb exercise capacity, symptoms of dyspnea and fatigue, and quality of life(QOL) being documented ( 13-16). It is possible that arm training, in people with COPD, may have a similar effect on arm exercise capacity, symptoms and QOL and therefore be a useful adjunct to lower limb exercise training. The role and effectiveness of arm training has not been investigated in detail ( 17, 18). The purpose of this paper is to review the current evidence for the effects of Upper Extremity exercise in people with COPD.
|
|
Methods
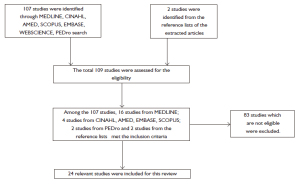
Medline, Scopus, Web of Science, CINAHL, EMBASE, AMED and PEDro databases were searched for relevant articles ( Fig 1). The inclusion criteria were randomised or quasi randomised controlled trials which included:
(1) People with COPD of any age or disease severity, as long as a formal diagnosis of COPD was based on acceptable criteria (pulmonary function tests);
(2) An arm endurance or strength training protocol in isolation or combined with other forms of training, examining outcomes of arm exercise capacity.
The exclusion criteria were:
(1) Studies including participants with other respiratory conditions such as asthma, bronchiectasis, interstitial lung disease and cystic fibrosis;
(2) Studies of strength and endurance training that did not include arm training or quantify arm performance with arm specific outcome measures;
(3) Studies written in languages other than English.
For the purpose of this review studies were divided into two main categories, namely arm endurance training and arm strength training. Arm endurance training was defined as the application of an exercise load above 50% of peak work capacity, in order to improve aerobic capacity ( 19). Studies which investigated arm endurance training were further subdivided according to whether the weight of the arm was supported or unsupported. Unsupported arm exercise was classified as any form of arm exercise where the weight of the arm was not supported ( 9) and included activities such as static arm elevation at 90 degrees shoulder flexion, performing tasks while the arms were elevated above shoulder level or moving the arms to perform functions such as lifting free weights or weighted dowels. Supported arm exercise was regarded as arm exercise in which some, or all, of the weight of the arm was supported ( 9), such as arm cycle ergometry. Strength training was defined as an exercise modality which involved the application of external resistance to a particular muscle group in order to increase muscle cross-sectional area and strength measurements ( 20). The effect of combined arm endurance and strength training was also investigated. The outcome measures examined in the selected trials included peak arm work capacity, arm exercise endurance, metabolic and ventilatory responses to arm exercise, QOL, dyspnea and perceived exertion during arm exercise and arm muscle strength. In this review, peak arm exercise capacity was used to define work performed during an incremental test and arm endurance capacity was used to define work done in a set time or to define the time taken to do set work. In addition to outlining the results of individual studies, where sufficient information was provided, post-intervention data were pooled and a meta-analysis conducted. In total, five arm endurance and two arm strength training trials were included in three separate meta-analyses ( Figs 2-4), with the effect size being interpreted descriptively using the terms described by Cohen ( 21).
|
|
Results
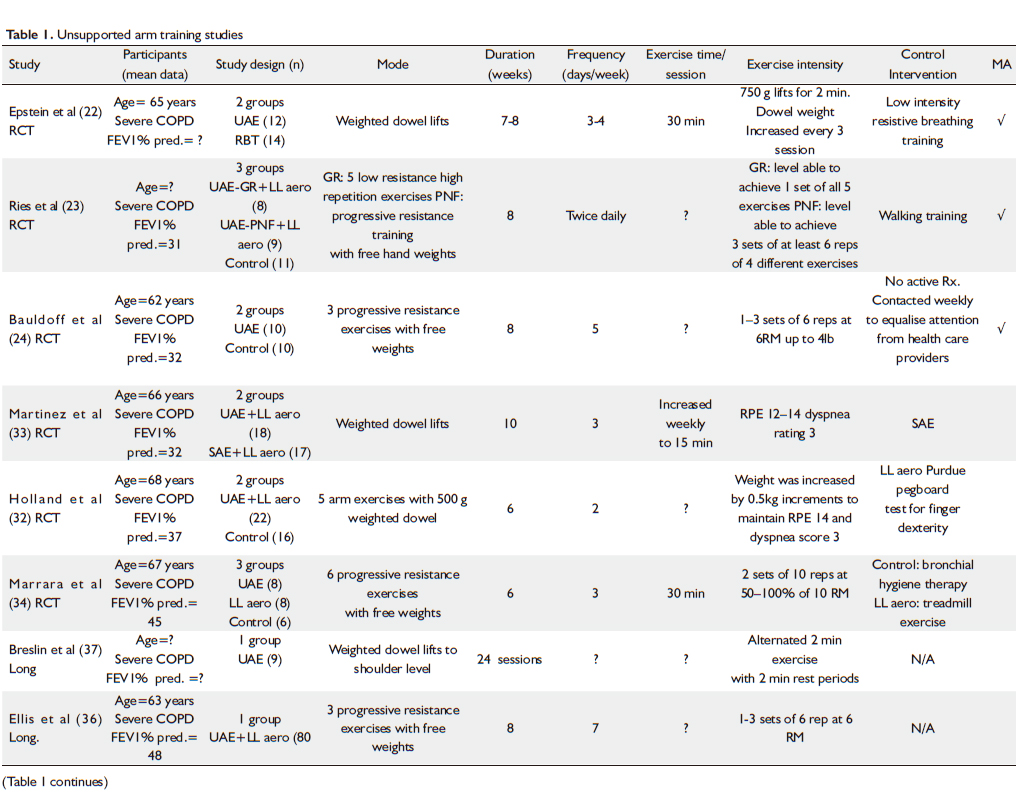
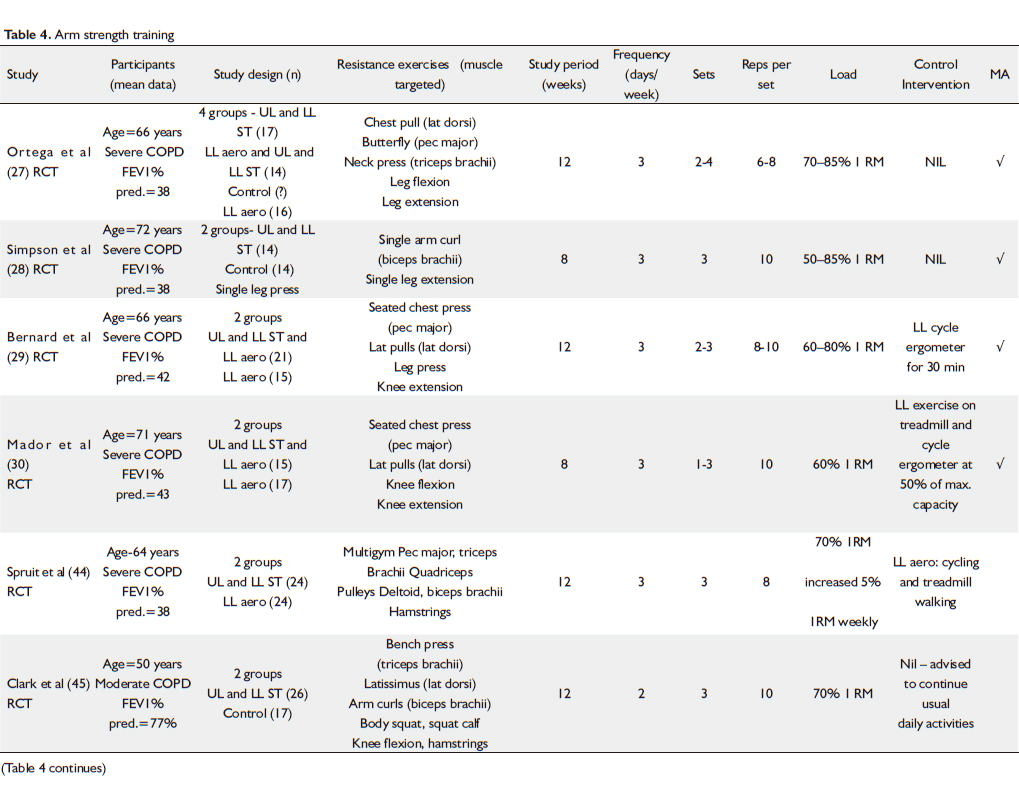
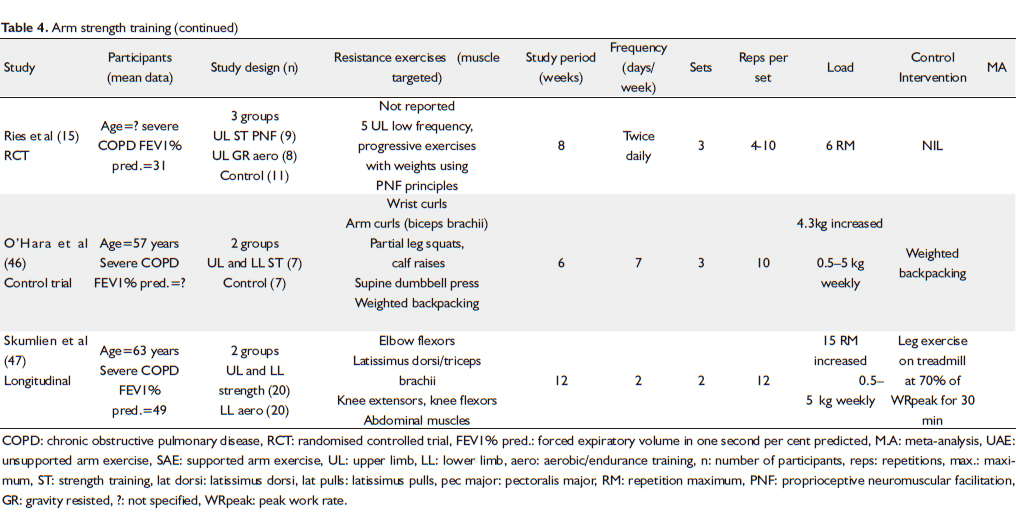
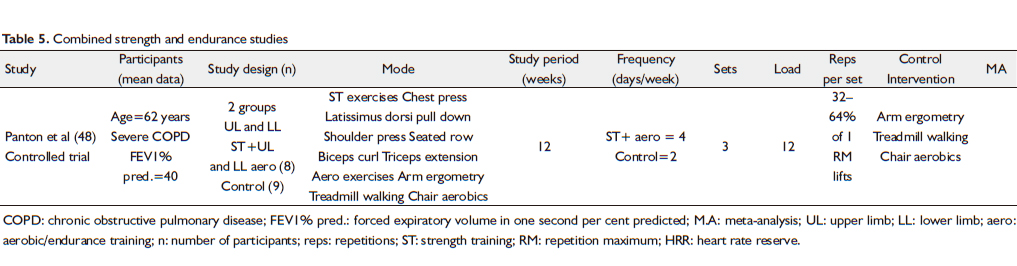
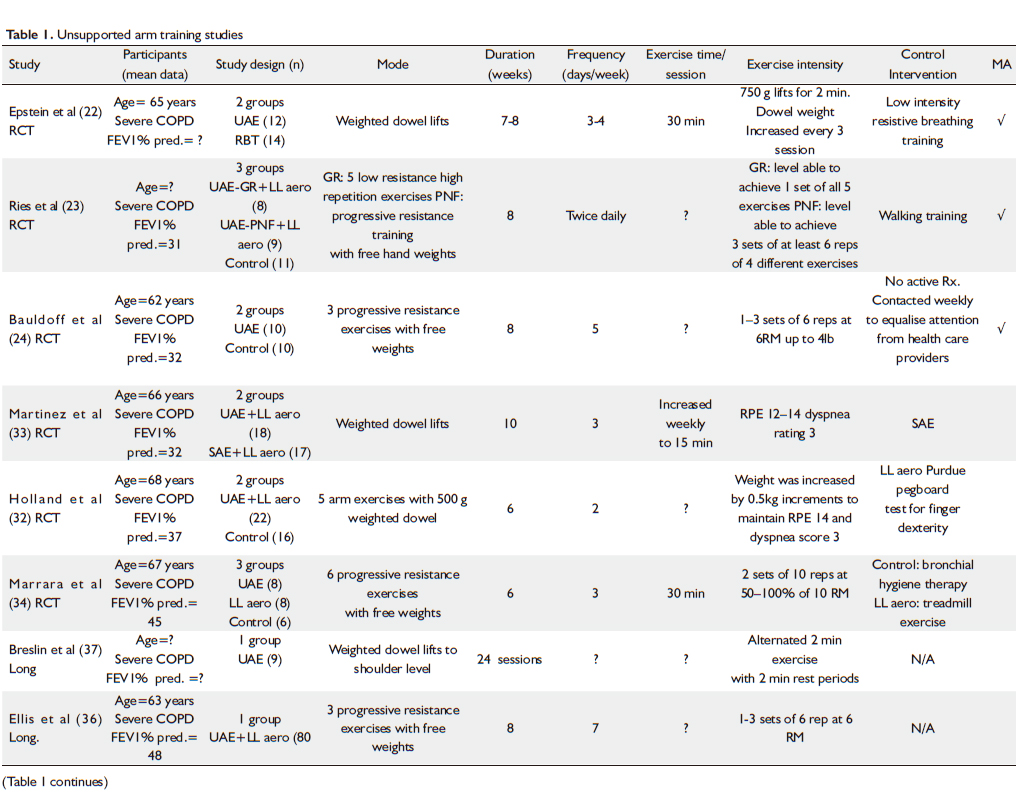
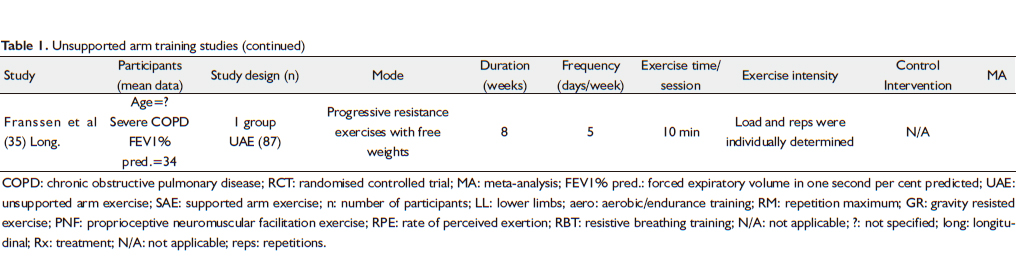
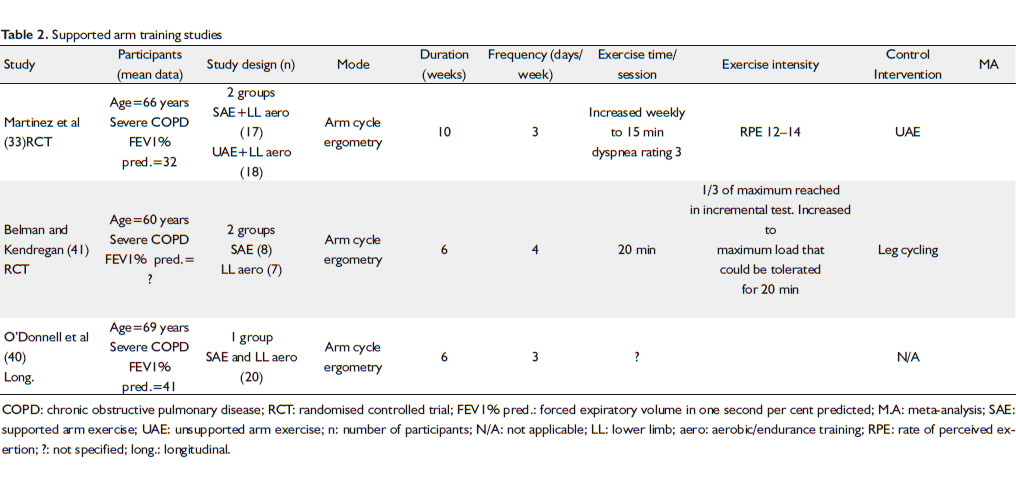
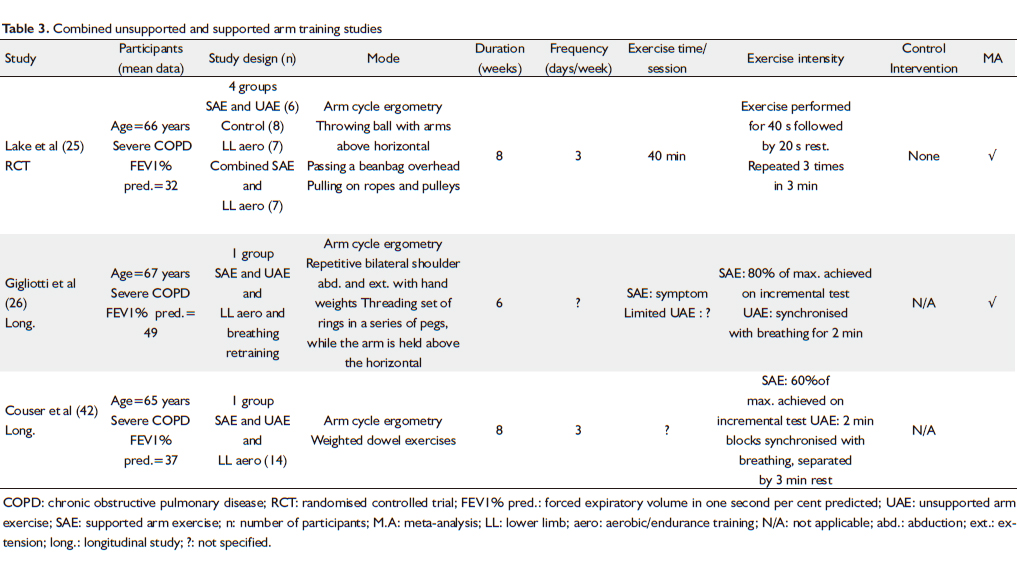
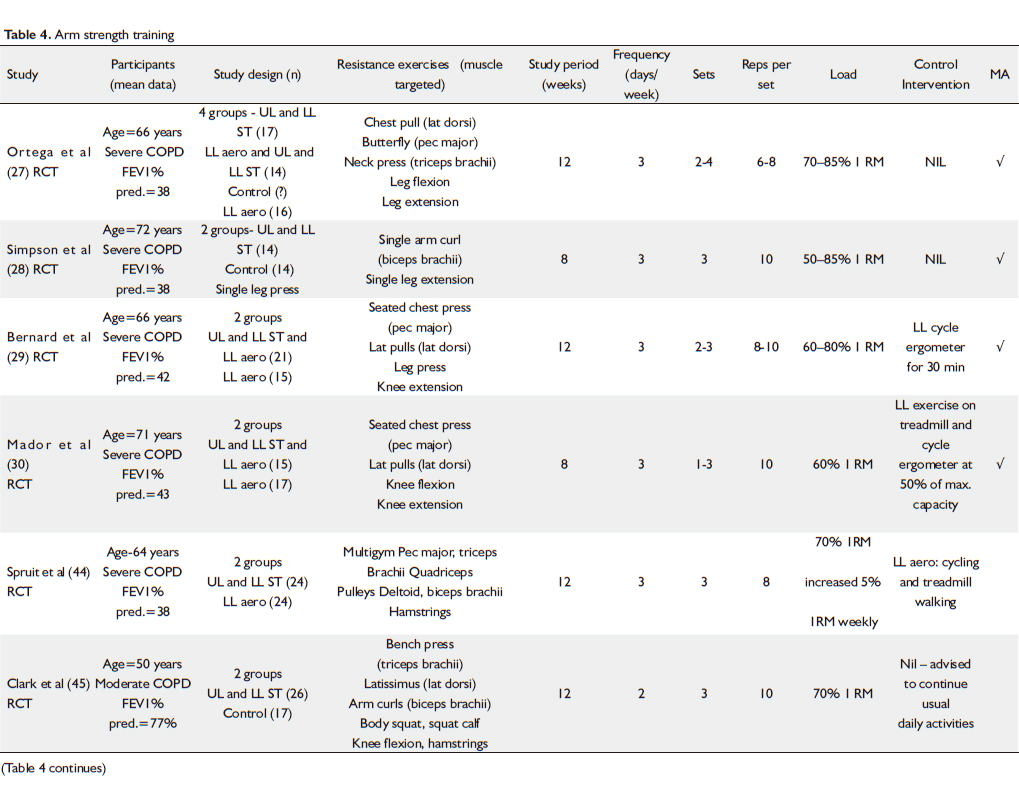
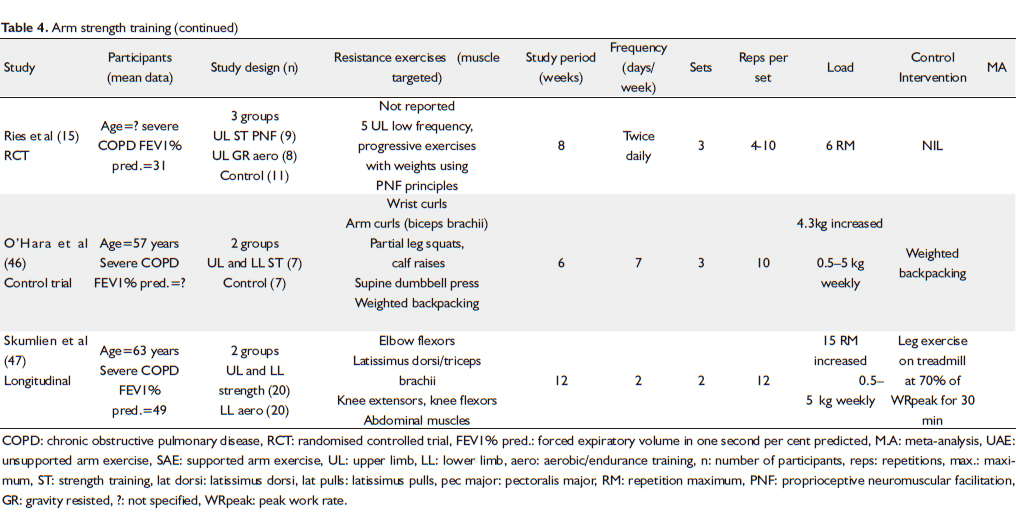
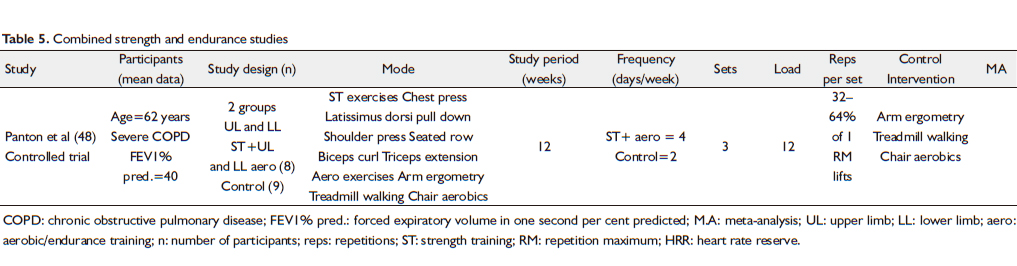
Selection of studies: The abstracts of 101 articles were identified during an electronic search on Medline, with 16 studies selected as relevant to the review. A repetition of the search on CINAHL, EMBASE, AMED, Scopus and Web of Science revealed four more articles and on searching the PEDro database, two more relevant trials were located. Two further articles were identified from the reference lists of extracted articles. A total of 14 studies examined the effects of arm endurance training ( Tables 1-3) and nine investigated the effects of arm strength training ( Table 4). In addition, one study compared arm endurance to arm strength training and was included in both the arm endurance and strength review, while another trial combined arm endurance and arm strength training ( Table 5). Thus, a total of 24 relevant papers were identified for review.
Effect of endurance training
The effect of unsupported arm training on arm endurance capacity was examined by pooling post intervention data from three studies ( 22-24) with 71 participants using a fixed effects model. The Meta analysis indicated that unsupported arm training increased arm endurance capacity (standard mean difference [SMD] =1. 25; 95% CI - 0.16 to 2. 66) ( Fig 2). The effect of combined unsupported and supported arm training, on peak arm exercise capacity, was examined by pooling post-intervention data from two studies, ( 25, 26) with 45 participants using a fixed effects model. Combined arm training was found to have a very large positive effect on peak arm exercise capacity (SMD=1. 27; 95% CI=0. 59 to 1. 94) ( Fig 3).
Effect of strength training
The effect of machine and free weight arm strength training, on peripheral arm muscle strength, was examined by pooling post-intervention data from four trials ( 27-30) with 129 participants, using a fixed effects model. The meta-analysis showed that arm strength training moderately increased peripheral arm strength (SMD=0. 46; 95%; CI=0. 10 to 0. 81) ( Fig 4).
|
|
Discussion
Unsupported endurance training
Arm activity in people with COPD results in a significant increase in metabolic and ventilatory demand, which is most marked during unsupported arm tasks ( 4-6, 31). This finding, combined with the recognition that unsupported arm work closely simulates the arm activities of daily living, has provoked interest in the effectiveness of unsupported arm training. Overall, six randomised controlled trials ( 22-24, 32-34) and three longitudinal studies ( 35-37) have investigated the impact of unsupported arm training on arm exercise capacity in people with COPD and one study has examined the effect of unsupported arm training on QOL ( 32). The majority of the research has come from trials with small participant numbers, which included adults over 60 years of age, with severe COPD. These trials ranged from 6 to 10 weeks in length, with participants training from 2 days a week to twice daily. Unsupported arm training consisted of weighted dowel lifts or low resistance high repetition arm exercises with free weights ( Table 1) and either formed part of a comprehensive outpatient rehabilitation programme or was implemented as the sole training strategy. The effectiveness of unsupported arm training on endurance capacity, peak arm work capacity, dyspnea, perceived exertion, metabolic and ventilatory demands and QOL were investigated in these studies. There were sufficient data from three studies ( 22-24) for a meta-analysis to be performed on the effect of unsupported arm training on arm endurance capacity ( Fig 2). However, the effect of unsupported arm exercise on other outcome measures, such as peak arm exercise capacity, dyspnea and perceived exertion could not be pooled due to insufficient raw data ( 32-37) As a consequence the results of these studies will be outlined separately and comparisons made, where appropriate. The meta-analysis of unsupported arm training on arm endurance capacity indicated a large effect favouring the intervention. However, the precision of the estimate was poor given only three studies were eligible for inclusion and the wide standard deviation of the pooled results which spanned across zero. This implies that there is uncertainty whether all people with COPD will experience improvements in arm endurance capacity following unsupported arm training. Another four studies were not included in the analysis due to the absence of a control group or post-intervention data ( 33, 35-37). These trials also reported an increase in unsupported arm endurance time to fatigue following unsupported arm training with the exception of an observational study by Franssen et al. that found arm endurance capacity remained unchanged following unsupported arm training ( 35). Unsupported arm training has been shown to produce significant improvements in peak arm work capacity in two randomised controlled trials. Compared to sham intervention, unsupported arm training increased peak unsupported arm exercise on an incremental unsupported upper limb exercise test by an additional 55 seconds (95% CI=8 to102 seconds, P=0.02) ( 32). Statistically significant increases in peak arm work capacity on an arm cycle ergometer (P=0.0002) were also displayed following unsupported arm training ( 33). However, there was one disparity with Ries et al. demonstrating that unsupported arm training did not result in improved peak arm exercise capacity on the arm cycle ergometer ( 23), i.e. unsupported arm training did not result in improved performance for a test unrelated to the mode of training. Dyspnea and arm fatigue are common sequelae of unsupported arm exercise in people with COPD and are frequently reported during activities of daily living involving the arms ( 6). As unsupported arm activities are required for self-care and independent living, three randomised controlled trials have investigated the effect of unsupported arm training in relieving dyspnea and arm fatigue during arm tasks. Unsupported arm training was found to result in a significant decrease in perceived exertion and dyspnea at the end of arm exercise tests, even when performance levels increased ( 23, 32). In terms of symptoms during activities of daily living, one study reported significant improvements over time in ratings of perceived fatigue using the breathlessness and fatigue scale (P=0.03), however there was no difference over time for ratings of perceived breathlessness following unsupported arm training ( 24). Unsupported arm training has also been found to reduce the metabolic and ventilatory requirements for unsupported arm tasks. Compared to resistance breathing training, unsupported arm exercise at isotime has been shown to reduce oxygen consumption and minute ventilation by an additional 22% (P<0.05) and 27% (P<0.05) respectively ( 22). Following unsupported arm training a significant decrease in metabolic and ventilatory demand (P<0.05) was also obtained during a blackboard erasing task, which required sustained arm elevation ( 34). This finding is important because it is known that arm elevation in people with COPD is associated with high metabolic and ventilatory demand which limits their ability to perform unsupported arm tasks ( 11, 31, 38). There is insufficient evidence to determine whether unsupported arm training improves health related QOL in people with COPD. In the one study that did evaluate health related QOL, no additional improvements on the chronic respiratory questionnaire could be shown with unsupported arm and leg training compared to a group who underwent leg training alone ( 32). As illustrated by the above trials, unsupported arm training improves both arm endurance and peak arm exercise capacity with the SMD of the meta-analysis confirming that unsupported arm training has a large effect on arm endurance capacity. In addition, unsupported arm training appears to reduce oxygen consumption at a given submaximal workload. Other benefits may include reductions in symptoms such as dyspnea and perceived exertion at the end of arm exercise, although it is questionable whether this translates into an identifiable reduction in dyspnea during activities of daily living. The absence of trials investigating QOL prohibits conclusions of the effect of unsupported arm training on this outcome measure. Furthermore, variability in training protocols, small sample size, limited follow-up, the unknown reliability and validity of some outcome tests ( 39), the inability to perform a meta-analysis on some outcome measures and the poor precision of the estimate in the meta-analysis hinders the generalisations of the results and prevents definitive conclusions.
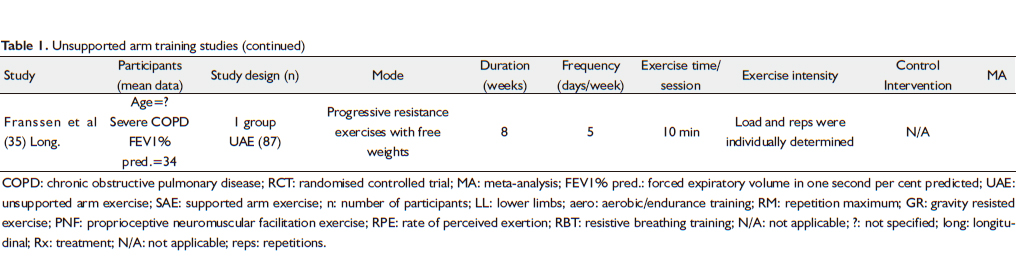
Supported endurance training
The effect of supported arm training, in people with COPD, has not been investigated as extensively as unsupported arm training, with only three trials examining the effects of supported arm training on arm exercise capacity ( 33, 40, 41). These studies had small participant numbers and predominately included adults over 60 years of age, with severe COPD. The duration of the supported arm exercise programme ranged from 6 to 10 weeks, with participants training 2 to 3 days per week. Supported arm training, in all programmes, included arm cycle ergometry which was generally performed as an adjunct to aerobic leg exercise training ( Table 2). The outcome measures evaluated in these trials included arm endurance capacity, peak arm work capacity and dyspnea and perceived exertion during arm tasks. The absence of sufficient outcome data in the three trials prevented the results from being pooled and meta-analysed and thus findings from individual trials will be outlined separately. Supported arm training has been shown to increase arm endurance capacity. All three trials ( 33, 40, 41) demonstrated an increase in arm endurance capacity, with supported arm training resulting in an improvement in supported arm endurance of (12±5)% (P<0.05) ( 40), a statistically significant increase in unsupported arm endurance (P=0.0002) ( 33) and higher sustained workloads for a set time period ( 41). In this latter study, the workload that could be sustained for 20 min on an arm cycle ergometer increased from (14±2.4) to (25±2.5) W/min following supported arm training. However, this trial provided no comparative data for the control group, so the true effect of supported arm training could not be determined. Supported arm training has also been shown to significantly increase peak arm work capacity during peak arm ergometry testing (P=0.002) ( 33). The effect of supported arm training on dyspnea and perceived arm exertion remains largely unknown, with only one study ( 40) investigating these outcome measures. In this trial, significant increases in arm endurance time were associated with significant reductions in Borg ratings of perceived breathlessness by 1.5 points (P<0.05) and exertion by 2 points (P<0.01) at isotime. To date, no studies have examined the effect of supported arm training on health related QOL. In summary, the three trials, which examined the effectiveness of supported arm training on arm exercise capacity, demonstrated that supported arm training may lead to improvements in arm endurance and peak arm exercise capacity. Other possible benefits include reductions in breathlessness and perceived exertion during supported arm tasks. The effect of supported arm training on QOL remains unclear, as it has not been investigated in the literature. Conclusions on the effects of supported arm training are constrained by the small number of trials investigating the effectiveness of supported arm training, the quality of the trials, small participant numbers, the different tools used to quantify outcome measures, the variability in training programmes and the inability to pool post-intervention data to conduct a meta-analysis. Furthermore, in the majority of the trials the participants were trained and tested on an arm cycle ergometer, which makes it difficult to determine if these results will translate into improvements in arm exercise capacity in activities of daily life.
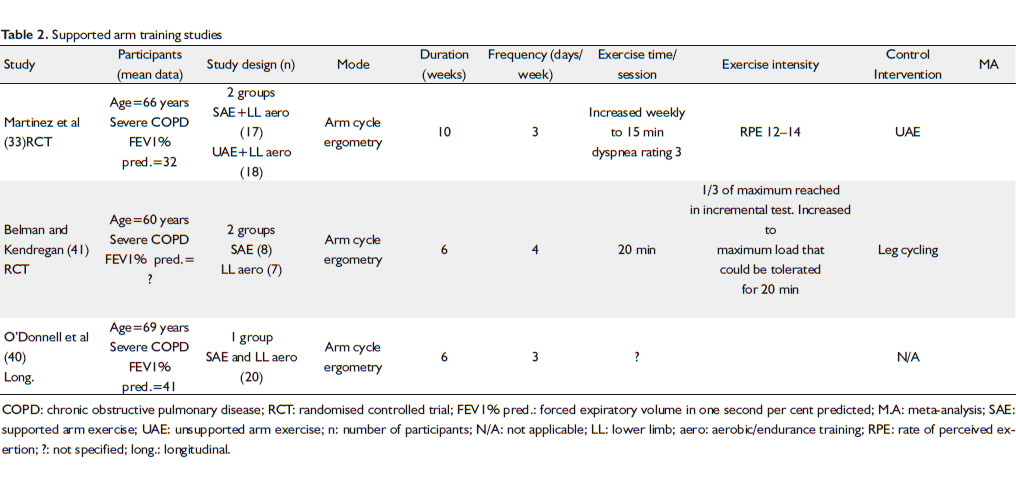
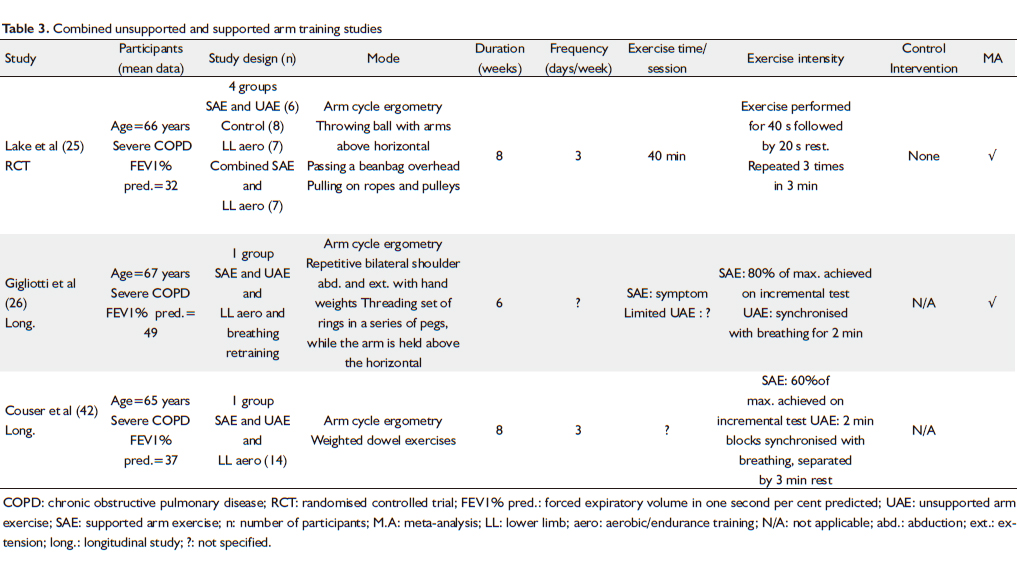
Combined unsupported and supported endurance training
Some research studies, investigating the effects of arm training on arm exercise capacity and QOL, have used a combination of unsupported and supported training modalities ( 25, 26, 42). Training consisted of arm cycle ergometry with varying resistance and unsupported arm tasks such as weighted dowel lifts, repetitive movements with light hand weights and tasks which required the arms to be sustained above shoulder level. These trials included people over 60 years of age with severe COPD, with the duration of the programmes ranging from 6 to 8 weeks and participants training three times per week ( Table 3). The effect of combined arm training on peak arm work capacity, dyspnea, perceived exertion, metabolic and ventilatory demands and QOL were investigated. Only the effect of combined arm training on peak arm work capacity permitted a meta-analysis. There was insufficient raw data, in trials investigating other outcome measures, which prevented the post-intervention results from being pooled. Meta-analysis of the effect of combined unsupported and supported arm training on peak arm exercise capacity confirmed that combined arm training has a very large positive effect on peak arm exercise capacity ( 25, 26). The effectiveness of combined arm training on arm endurance capacity could not be established as no trials investigated this outcome measure. The effect of combined unsupported and supported arm training on dyspnea and perceived exertion has been investigated in two trials. These results indicate that following combined arm training perceived dyspnea at peak exercise improved, with dyspnea levels remaining unchanged despite a higher peak work rate ( 25, 26). However, at submaximal work rates the results were conflicting. One randomised controlled trial found no change in dyspnea or perceived arm exertion scores during a submaximal supported arm test ( 25), while a recent longitudinal study indicated that at a standardised work rate on an arm ergometer both dyspnea and arm effort decreased significantly ( 26). Significant reductions in metabolic and ventilatory requirements with combined unsupported and supported arm training have been reported in people with COPD. Following 8 weeks of training, combined arm exercise has been demonstrated to reduce the metabolic and ventilatory requirements for arm elevation, with VO2 being shown to fall 21mL/min (P<0.05) and minute ventilation decreasing 1.4L/min (P<0.01), during 2 min of simple arm elevation ( 42). At a standardised submaximal arm ergometry work rate, combined arm training resulted in a significant decrease in minute ventilation ( 26). The effect of combined unsupported and supported arm training on health related QOL, in people with COPD, has been investigated in one study ( 25). The addition of combined arm training to leg training was found to lead to significant improvements in self efficacy on the Bandura Scale, which measures QOL, self-confidence and self-esteem. However, no improvements were noted with combined arm training alone, which suggests that combined arm training may not increase health related QOL when performed in isolation. In conclusion, the meta-analysis has indicated that combined unsupported and supported arm training has a very large positive effect on increasing peak arm exercise capacity. Other benefits of combined arm training may include a decreased metabolic and ventilatory demand, a reduction in dyspnea and arm effort during arm tasks and improved QOL when arm training was integrated into a comprehensive pulmonary rehabilitation programme. Again, variability in training protocols, small sample sizes, the absence of a meta-analysis for most outcome measures and the small number of studies eligible for inclusion in the meta-analysis, suggests that further investigations are required before definitive conclusions are drawn.
Strength training using machine weights and free weights
Skeletal arm muscle weakness, and the associated impact on exercise tolerance and QOL, provides a strong theoretical rationale for arm strength training in people with COPD. Overall, one systematic review ( 43), seven randomised controlled trials ( 23, 27-30, 44, 45), one controlled trial ( 46) and a longitudinal trial ( 47) have investigated the effectiveness of strength training on arm muscle strength and arm exercise capacity in people with COPD. The majority of these trials included people over 60 years of age with severe COPD, in an outpatient setting, with participants training from 3 days a week to twice daily, over a 6 to 12 week period. Training modalities implemented included either machine weights or free weights and in most trials arm strength training formed part of total body strength programme ( Table 4). The meta-analysis on the effect of machine and free weight arm strength training ( 27-30) on peripheral arm muscle strength indicated that arm strength training moderately increased peripheral arm strength (SMD=0. 46; 95% CI=0.10 to 0.81) ( Fig 4). These results correspond closely with a recent systematic review of peripheral muscle strength training in COPD ( 43), which pooled the results of three of the four trials considered in the above meta-analysis ( 27-29). These authors found strong evidence for arm strength training improving arm strength, with their random effects model for meta-analysis clearly indicating a positive effect favouring treatment (SMD=0.70; 95% CI= 0.28 to 1.11, P<0.001). A further four studies ( 44-47) were not included in the analysis due to the absence of a control group or post-intervention data. These trials also reported an increase in arm muscle strength following arm strength training. Arm strength training resulted in significant improvements in latissimus dorsi strength on a 1 repetition maximum (1 RM) test (P<0.05) ( 45) and an increase of 1.5kg on a 15 repetition maximum (15 RM) test compared to endurance training (P<0.05) ( 47). There were also significantly greater improvements in arm muscle strength, on a 15 RM elbow flexor test of 0.7kg (P<0.05) ( 47), compared to endurance training and an increase in shoulder abduction and elbow flexion force, measured via a handheld dynamometer, following 12 weeks of training ( 44). However, there was one disparity with O’Hara et al. reporting that a home based arm strength programme, for 6 weeks, did not lead to objective improvements in biceps brachii or triceps brachii isometric strength ( 46). The effect of arm strength training on arm endurance capacity has not been investigated extensively. The two randomised controlled trials which have examined this outcome measure both indicate that arm strength training has beneficial effects on arm endurance capacity ( 23, 45). In one study, arm strength training led to significant improvements in arm endurance capacity, measured by a sustained test of isokinetic muscle work, compared to no intervention ( 45). In another study, proprioceptive neuromuscular arm strength training resulted in the ability to perform six more arm lifts, in 1 min, holding a free hand weight, compared to no arm training (P<0.05) ( 23). In this trial, significant decreases in perceived breathlessness and exertion ratings at the end of 1 min of arm exercise were noted, even when performance time increased. This is the only trial that has investigated the effectiveness of arm strength training in relieving dyspnea and perceived exertion. Overall, arm strength training appears to improve arm muscle strength, with a meta-analysis of the data confirming that arm strength training has a moderately positive effect on arm muscle strength in people with COPD. Furthermore, arm strength training may also enhance arm exercise capacity by improving arm endurance and reducing dyspnea and exertion at higher arm workloads. However, the small sample size in the above studies, variations in the intensity and duration of training, the inability to conduct a meta-analysis for all outcome measures and the fact that most trials were not designed specifically to examine the effect of arm strength training on arm exercise capacity, makes it difficult to draw explicit conclusions. Key areas requiring further investigation are the impact of arm strength training on peak arm exercise capacity and health related QOL. While some studies did include QOL outcome measures, they were confounded by leg strength training interventions and therefore did not reflect the effect of arm strength training alone on QOL.
Combined strength and endurance training
Theoretically, people with COPD who participate in a combination of strength and endurance arm training have the potential to gain the benefits of both modes of training. The effect of combined arm strength and endurance training on arm exercise capacity in people with COPD has been investigated in one study ( Table 5) ( 48). In this controlled trial, arm strength, assessed via a 1 RM Cybex chest press, increased an additional 33% in the combined group compared to the control endurance group. The combined group also had a significantly greater arm endurance, with an additional 12 arm raises being achieved in 1 min, compared to the control group (P<0.05). The results of this study indicate that a combined arm strength and endurance exercise programme may achieve greater improvements in arm exercise capacity than can be achieved by endurance training alone. However, further high quality studies are required to test this hypothesis. The effects of combined arm training on QOL also need further examination.
|
|
Conclusions
The observation that arm exercise, in people with COPD, is associated with dyssynchronous breathing and marked dyspnea ( 5, 6) has provoked interest in the role of arm training in improving arm function in these people. Unsupported arm training appears to be the optimal mode of arm endurance training, with this review finding strong evidence for unsupported arm training improving arm endurance capacity in the majority of people with COPD. This review has also shown that unsupported arm training positively influences peak arm exercise capacity, metabolic and ventilatory demands and symptoms such as perceived arm exertion and dyspnea. This mode of arm training also closely resembles the training required to improve activities of daily living, since improved exercise performance is specific for the muscles and tasks involved in training ( 23, 25, 41). Thus, based on the current body of evidence, it is recommended that arm endurance training can be integrated into pulmonary rehabilitation programmes to improve arm exercise capacity. This statement is supported by pulmonary guidelines ( 15, 16), which recommend unsupported arm training be included routinely as a component of the rehabilitation of people with COPD. This review of arm strength training in people with COPD has found moderate improvements in peripheral muscle strength with arm strength training. Since peripheral muscle weakness contributes to arm exercise limitation in people with lung disease ( 49), this review confirms that arm strength training should be implemented into pulmonary rehabilitation programmes. While all modes of arm strength training produce similar magnitude improvements in arm strength, free weight training does have the inherent advantage of being easily maintained in the home environment and is therefore probably the optimal mode of training. Currently, there is insufficient high quality evidence to support integrating an arm strength programme for people with COPD to improve functional arm tasks. Further high quality research, with large participant numbers, should be directed towards investigating the long term benefits of arm training and the effectiveness of combined arm endurance and strength training. The impact of arm training on QOL and functional performance in everyday situations has also not been comprehensively investigated. Further research should therefore be directed at attempting to establish the optimal arm training format, conducive to improvements in arm tasks important for daily living and increased societal participation in people with COPD.
|
|
References
- Mannino DM. COPD: epidemiology, prevalence, morbidity, mortality, and diseases heterogeneity. Chest 2002;121:S121-6.[LinkOut]
- Celli BR. Update on the management of COPD. Chest 2008;133:1451-62.[LinkOut]
- Buist SA, Roisin RR, Anzueto A, Calverley P, Casas A, Cruz A, et al. Executive summary: global strategy for the diagnosis, management, and prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease. Oregon: Medical Communications Resources, Inc., 2007; 2-3.
- Criner GJ, Celli BR. Effect of unsupported arm exercise on ventilatory muscle recruitment in patients with severe chronic airflow obstruction. Am Rev Respir Dis 1988;138:856-61.[LinkOut]
- Celli BR, Rassulo J, Make BJ. Dyssynchronous breathing duringarm but not leg exercise in patients with chronic airflow obstruction. N Engl J Med 1986;314:1485-90.[LinkOut]
- Tangri S, Woolf CR. The breathing pattern in chronic obstructive lung disease during the performance of some common daily activities. Chest 1973;63:126-7.[LinkOut]
- Celli BR. The clinical use of upper extremity exercise. Clin Chest Med 1994;15:339-49.[LinkOut]
- Spiro S, Hahn M, Edwards R, Pride N. An analysis of the physiological strain of submaximal exercise in patients with chronic obstructive bronchitis. Thorax 1975;30:415-25.[LinkOut]
- Alison J. Upper limb exercise in normal subjects and patients with cystic fibrosis. Thesis (PhD). Department of Medicine; University of Sydney, 2001.
- Owens GR, Thompson FE, Sciurba FC, Robertson R, Metz KF, Volmer RR. Comparison of arm and leg ergometry in patients with moderate chronic obstructive lung disease. Thorax 1988;43:911-5.[LinkOut]
- Baarends EM, Schols AM, Slebos DJ, Mostert R, Janssen PP, Wouters EF. Metabolic and ventilatory response pattern to arm elevation in patients with COPD and healthy age-matched subjects. Eur Respir J 1995;8:1345-51.[LinkOut]
- McKeough ZJ, Alison JA, Bye PT. Arm exercise capacity and dyspnea ratings in subjects with chronic obstructive pulmonary disease. J Cardiopulm Rehabil 2003;23:218-25.[LinkOut]
- Lacasse Y, Goldstein R, Lasserson TJ, Martin S. Pulmonary rehabilitation for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006;CD003793.[LinkOut]
- Cambach W, Wagenaar RC, Koelman TW, van Keimpema AR, Kemper HC. The long-term effects of pulmonary rehabilitation in patients with asthma and chronic obstructive pulmonary disease: a research synthesis. Arch Phys Med Rehabil 1999;80:103-11.[LinkOut]
- Ries AL, Bauldoff GS, Carlin BW, Casaburi R, Emery CF, Mahler DA, et al. Pulmonary rehabilitation: joint ACCP/AACVPR evidence-based clinical practice guidelines. Chest 2007;131:4S-42S.[LinkOut]
- Nici L, Donner C, Wouters E, Zuwallack R, Ambrosino N, Bourbeau J, et al. American thoracic society/European respiratory society statement on pulmonary rehabilitation. Am J Respir Crit Care Med 2006;173:1390-413.[LinkOut]
- Bourjeily G, Rochester CL. Exercise training in chronic obstructive pulmonary disease. Clin Chest Med 2000;21:763-81.[LinkOut]
- Rochester CL. Exercise training in chronic obstructive pulmonary disease. J Rehabil Res Dev 2003;40:59-80.[LinkOut]
- Åstrand P-O, Rodahl K, Dahl HA, Stromme SB. Textbook of work physiology: Physiological bases of exercise. 4th ed. Champaign: Human Kinetics; 2003.
- Pollock ML, Wilmore JH. Exercise in health and disease: Evaluation and prescription for prevention and rehabilitation. 2nd ed. Philadelphia: Saunders;1990. 204 p.
- Cohen J. Statistical power analysis for behavioural sciences. 2nd ed. New York: Academic Press; 1988.
- Epstein SK, Celli BR, Martinez FJ, Couser JI, Roa J, Pollock M, et al. Arm training reduces the VO2 and VE cost of unsupported arm exercise and elevation in chronic obtructive pulmonary disease. J Cardiopulm Rehabil 1997;17:171-7.[LinkOut]
- Ries AL, Ellis B, Hawkins RW. Upper extremity exercise training in chronic obstructive pulmonary disease. Chest 1988;93:688-92.[LinkOut]
- Bauldoff GS, Hoffman LA, Sciurba F, Zullo TG. Home-based, upper-arm exercise training for patients with chronic obstructive pulmonary disease. Heart Lung 1996;25:288-94.[LinkOut]
- Lake FR, Henderson K, Briffa T, Openshaw J, Musk AW. Upper limb and lower-limb exercise training in patients with chronic airflow obstruction. Chest 1990;97:1077-82.[LinkOut]
- Gigliotti F, Coli C, Bianchi R, Grazzini M, Stendardi L, Castellani C, et al. Arm exercise and hyperinflation in patients with COPD: effect of arm training. Chest 2005;128:1225-32.[LinkOut]
- Ortega F, Toral J, Cejudo P, Villagomez R, Sánchez H, Castillo J, et al. Comparison of effects of strength and endurance training in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2002;166:669-74.[LinkOut]
- Simpson K, Killian K, McCartney N, Stubbing DG, Jones NL. Randomised controlled trial of weightlifting exercise in patients with chronic airflow limitation. Thorax 1992;47:70-5.[LinkOut]
- Bernard S, Whittom F, Leblanc P, Jobin J, Belleau R, Bérubé C, et al. Aerobic and strength training in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1999;159:896-901.[LinkOut]
- Mador MJ, Bozkanat E, Aggarwal A, Shaffer M, Kufel TJ. Endurance and strength training in patients with COPD. Chest 2004;125:2036-45.[LinkOut]
- Martinez FJ, Couser JI, Celli BR. Respiratory response to arm elevation in patients with chronic airflow obstruction. Am Rev Respir Dis 1991;143:476-80.[LinkOut]
- Holland AE, Hill CJ, Nehez E, Ntoumenopoulos G. Does unsupported upper limb exercise training improve symptoms and quality of life for patients with chronic obstructive pulmonary disease? J Cardiopulm Rehabil 2004;24:422-7.[LinkOut]
- Martinez FJ, Vogel PD, Dupont DN, Stanopoulos I, Gray A, Beamis JF. Supported arm exercise vs unsupported arm exercise in the rehabilitation of patients with severe chronic airflow obstruction. Chest 1993;103:1397-402.[LinkOut]
- Marrara KT, Marino DM, de Held PA, de Oliveira AD, Jamami M, Di Lorenzo VA. Different physical therapy interventions on daily physical activities in chronic obstructive pulmonary disease. Respir Med 2008;102:505-11.[LinkOut]
- Franssen FM, Broekhuizen R, Janssen PP, Wouters EF, Schols AM. Limb muscle dysfunction in COPD: effects of muscle wasting and exercise training. Med Sci Sports Exerc 2005;37:2-9.[LinkOut]
- Ellis B, Ries AL. Upper extremity exercise training in pulmonary rehabilitation. J Cardiopulm Rehabil 1991;11:227-31.[LinkOut]
- Breslin E, Pollock M, Martinez FJ, Couser JI, Celli BR. Improved respiratory muscle function and exercise endurance with unsupported arm exercise training (UAET) [abstract]. Am Rev Respir Dis 1990;14:A509.
- Dolmage TE, Maestro L, Avendano MA, Goldstein RS. The ventilatory response to arm elevation of patients with chronic obstructive pulmonary disease. Chest 1993;104:1097-100.[LinkOut]
- Zhan S, Cerny FJ, Gibbons WJ, Mador MJ, Wu YW. Development of an unsupported arm exercise test in patients with chronic obstructive pulmonary disease. J Cardiopulm Rehabil 2006;26:180-7; discussion 8-90.[LinkOut]
- O’Donnell DE, McGuire M, Samis L, Webb KA. General exercise training improves ventilatory and peripheral muscle strength and endurance in chronic airflow limitation. Am J Respir Crit Care Med 1998;157:1489-97.[LinkOut]
- Belman MJ, Kendregan BA. Exercise training fails to increase skeletal muscle enzymes in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis 1981;123:256-61.[LinkOut]
- Couser JI, Martinez FJ, Celli BR. Pulmonary rehabilitation that includes arm exercise reduces metabolic and ventilatory requirements for simple arm elevation. Chest 1993;103:37-41.[LinkOut]
- O’Shea SD, Taylor NF, Paratz J. Peripheral muscle strength training in COPD: a systematic review. Chest 2004;126:903-14.[LinkOut]
- Spruit MA, Gosselink R, Troosters T, de Paepe K, Decramer M. Resistance versus endurance training in patients with COPD and peripheral muscle weakness. Eur Respir J 2002;19:1072-8.[LinkOut]
- Clark CJ, Cochrane LM, Mackay E, Paton B. Skeletal muscle strength and endurance in patients with mild COPD and the effects of weight training. Eur Respir J 2000;15:92-7.[LinkOut]
- O’Hara W, Lasachuk K, Matheson P, Renahan M, Schlotter D, Lilker E. Weight training and backpacking in chronic obstructive pulmonary disease. Respir Care 1984;29:1202-10.
- Skumlien S, Aure Skogedal E, Skrede Ryg M, Bjortuft O. Endurance or resistance training in primary care after in-patient rehabilitation for COPD? Respir Med 2008;102:422-9.[LinkOut]
- Panton LB, Golden J, Broeder CE, Browder KD, Cestaro-Seifer DJ, Seifer FD. The effects of resistance training on functional outcomes in patients with chronic obstructive pulmonary disease. Eur J Appl Physiol 2004;91:443-9.[LinkOut]
- Hamilton AL, Killian KJ, Summers E, Jones NL. Muscle strength, symptom intensity, and exercise capacity in patients with cardiorespiratory disorder. Am J Respir Crit Care Med 1995;152:2021-31.[LinkOut]
Cite this article as: Kathiresan G, Jeyaraman SK, Jaganathan J. Effect of upper extremity exercise in people with COPD. J Thorac Dis 2010;2(4):223-236. doi: 10.3978/j.issn.2072-1439.2010.11.4
|