CT localization for a patient with a ground-glass opacity pulmonary nodule expecting thoracoscopy: a mixture of lipiodol and India ink
Introduction
Most pulmonary nodules (PNs) can be palpable, but small or deeply seated lesions may require appropriate localization prior to surgery. Recently, video-assisted thoracoscopic surgery (VATS) has become the mainstay for undetermined PNs for diagnostic and/or curative purpose. However, pure ground-glass opacity (GGO) lesions are usually difficult to detect without localization via thoracoscopic view, neither the pathologists can easily find target lesions in the frozen sections, even in cases with preoperative localization. Lipiodol has been used to confirm adequate localization within or near the deep-seated lung lesions. Also, India ink tattoo has been applied to gastrointestinal surgery for preoperative localization for decades. Thus, we are introducing a modified localization technique using a mixture of lipiodol and India ink for easy detection to facilitate VATS resection and for frozen or permanent analysis of undefined PNs.
Case presentation
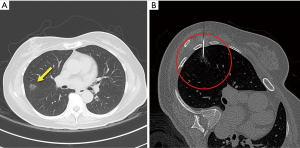
A 52-year-old female patient presented with a pure GGO lesion (12 mm) in the right upper lobe. This peripherally located pulmonary lesion was incidentally found during a work-up for intermittent cough symptom, and it was strongly suggestive of primary lung malignancy (adenocarcinoma) on chest CT scan (Figure 1A). The distance of the GGO lesion from the pleural surface was less than 10 mm. CT-guided needle biopsy was not considered for the lesion because surgical diagnosis was planned. Informed consent was obtained from the patient about the localization technique and surgical procedures. For preoperative localization prior to VATS surgery, we used 0.5 mL of lipiodol (Lipiodol Ultra Fluide; Laboratoire Guerbet, Aulnay-Sous-Bois, France) and 0.5 mL of India ink (Black India Ink; Windsor & Newton, France). A sterile solution of India ink was prepared by boiling for 30 seconds in a stainless steel bowl. Then, we created a mixture (1.0 mL) of India ink and lipiodol using a three-way connector and two 10-mL syringes with aseptic technique. A dedicated CT scanner was used for the procedure (Somatom Definition AS+; Siemens, Erlangen, Germany). The patient was placed in a posterior oblique position, and then an expiratory CT scan was performed (120 kV, 35 mAs, slice thickness 1 mm, reconstruction interval 1 mm). After sterilization of the skin and infiltration of local anesthetics (1% lidocaine), an 18-gauge Chiba biopsy needle (Calibrated Chiba Stylet needle; Cook Medical Co., Bloomington, IN) was percutaneously inserted towards the target using intermittent CT guidance by a radiologist (Figure 1B). Once the needle was approximately 1 mm superior to the target, the mixture (0.2 mL) was slowly injected in order to mark the area near the upper border of the target lesion rather than the target nodule itself. Another 0.2 mL of the mixture was injected while the needle was being withdrawn from the lesion in order to mark the visceral pleural surface. This localization procedure took less than 30 minutes, and the patient was transferred to the operating room immediately after the procedure. Whole procedure was conducted with aseptic condition and tattooing-technique-related complications including hematoma or ink spillage were not detected. Pulmonary complications such as hemorrhage or pneumothorax were also not observed on the follow-up chest X-ray.
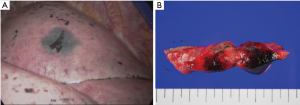
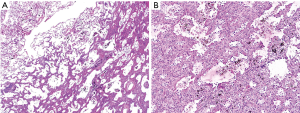
VATS wedge resection followed by lobectomy is briefly described as follows. In the operating room, single lung ventilation was maintained under general anesthesia by intubation with a double lumen endotracheal tube in a left lateral decubitus position for thoracoscopic surgery. A trocar port was inserted into the mid-axillary line at the level of the eighth intercostal space for the thoracoscopy. A minimal working incision was made on the fourth intercostal space, and a wound protector was placed for two-port VATS. A black-pigmented tattoo lesion was clearly identified under 30° 10-mm thoracoscopic views (Figure 2A). Wedge resection of the GGO lesion including the tattooed area was performed with an adequate resection margin using endo staplers (Ethicon Endo-Surgery, Cincinnati, OH), without palpation procedure or fluoroscopy assistance (Figure 2B). Frozen sections revealed suggestive of adenocarcinoma, and subsequent VATS lobectomy and mediastinal lymph node dissection were performed. Duration of the operation was 140 minutes, and the estimated blood loss was 50 mL. The pathologic results revealed 1.3 cm × 0.9 cm sized, stage I (pT1aN0M0), well-differentiated adenocarcinoma with lepidic predominance. Microscopic examination revealed infiltration of black pigments in the alveolar spaces and interstitial tissue in the peripheral portion of the nodule (Figure 3). Pleural invasion was absent (PL0), and mutation studies demonstrated a positive EGFR mutation in exon 21 (pL858R). The patient was discharged on postoperative day 5 without complications, and recurrence was not detected during follow-up period of 15 months.
Discussion
Undefined PNs are being increasingly encountered with the wide use of multi-detector CT scans in screening or surveillance for follow up of lung cancer. Currently, VATS has become the standard procedure for both accurate pathological diagnosis and therapeutic modality for PNs with little morbidity. However, it is difficult to identify very small and deeply seated PNs; even for peripheral nodules, small faint lesions, such as non-palpable GGO PNs, are thoracoscopically invisible without pleural retraction (1). Furthermore, accurate preoperative localization of indiscernible lesions is important to save operative time to find the obscure targets, and to avoid thoracotomy conversion in VATS surgery (2). Thus, several studies have suggested various methods of intra-operative or preoperative localization on PNs using a dye marker or metallic material (such as hook-wire or microcoils) to improve the success rate of VATS surgery (3).
Dendo et al. divided preoperative localization techniques into three types: imaging modalities such as ultrasonography and CT fluoroscopy; injection of dyes, contrast media, radionuclides, or colored adhesive agents; and hook-wire placement (4). All of these methods have demonstrated beneficial and satisfactory results, but some have shown technical drawbacks. For example, hook-wire has been used with acceptable results from several studies, but failure occurred in 3–20% of patients due to its dislodgement, pneumothorax, bleeding, and air embolism (5). We have also introduced preoperative CT-guided localization using fragmented platinum microcoils and fluoroscopy-assisted thoracoscopic surgery (FATS), which were followed with 6.2% of detecting failures due to displacement of microcoils. For contrast media, barium sulfate has demonstrated its efficacy for labeling due to its radio-opaque nature under CT guidance (1,6). The radio-opacity of barium sulfate can be clearly seen on the fluoroscopic monitor but radiation exposure should be considered, and it sometimes interferes with pathological analysis. Several studies have revealed the efficacy of tattooing using indigo carmine and methylene blue solution, which can be then directly seen, but it has its limitations of often disappearing over time or over-diffusion, making it difficult to incorporate into the operative schedule after localization.
India ink has been applied to gastrointestinal surgery fields with satisfactory results (7,8). Small number of case reports showed its limitation such as transmural injection and inflammatory effect. However, it has been regarded as an acceptable material for endoscopic preoperative localization in colorectal surgery fields with proper preparation and injection technique (9,10). In 2009, Magistrelli et al. introduced India ink as a localization agent for undiagnosed PNs, but it has not been actively used in the current VATS fields (11). Lipiodol is also a radio-opaque, lipid-soluble material, which demonstrated acceptable results from our previous report as well as several studies on CT-guided percutaneous localization (1,12-15). Jin et al. reported injection of a mixture of lipiodol and methylene blue in rabbit lungs to evaluate their localization ability (16). The mixture showed superior localization over methylene blue alone, which directed us to focus on the mixture of lipiodol and India ink solution for VATS surgery.
The value of our technique is that India ink plays a key role in detection through pleural tattooing for surgical detection during VATS. We injected the mixture of dye solution to the nearest area rather than target lesion to indicate the main pathologic lesion without contaminating it, to help the pathologist with the detection of obscure lesion on frozen sections and permanent analysis. In our case, the size of the GGO lesion was small and located peripherally that it was easily resected with adequate margins after retractions under collapsed lung. The radio-opacity of lipiodol has a useful role to detect the target lesion in CT guided percutaneous localization. It can be applied to guide the lesion during stapling procedure using fluoroscopy to confirm the resection margins, if needed. Additionally, our technique does not cause injury to the pulmonary tissue or pain, which can be developed by dislodgement of hookwire or microcoil when lung deflates during one lung ventilation or lung manipulation during VATS. Recently, uniportal VATS is increasingly performed for pulmonary resection but localization of deeply situated or GGO PNs are still challenging. Thus, our localization technique is thought to be applicable and promising for easy detection for indiscernible, non-palpable lesions via a minimal 3- to 4-cm working incision in uniportal VATS fields (17). The disadvantage of our technique is that black color may not be clear enough to demarcate or indicate the lesion in cases with severe anthracotic pigmented lung surface. Proper standardized method should be also reassessed in both preparation (sterilization and dilution) and injection procedure to prevent possible adverse effects. However, this technique is easy to perform for preoperative localization for GGO lesion prior to VATS, as was demonstrated by the satisfactory outcome of our case. The pathologic result was also clear enough to interpret without interruption in microscopic analysis by pathologists.
In conclusion, we have introduced a novel technique using a mixture of lipiodol and India ink for preoperative localization with satisfactory results. This simple, effective procedure can be considered as an option to label the target lesions of GGO predominant PNs prior to VATS surgery. However, further studies are needed to establish the efficacy and safety of this technique.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by IRB of Seoul St. Mary’s Hospital and written informed consent was obtained from the patient.
References
- Moon SW, Wang YP, Jo KH, et al. Fluoroscopy-aided thoracoscopic resection of pulmonary nodule localized with contrast media. Ann Thorac Surg 1999;68:1815-20. [Crossref] [PubMed]
- Santambrogio R, Montorsi M, Bianchi P, et al. Intraoperative ultrasound during thoracoscopic procedures for solitary pulmonary nodules. Ann Thorac Surg 1999;68:218-22. [Crossref] [PubMed]
- Powell TI, Jangra D, Clifton JC, et al. Peripheral lung nodules: fluoroscopically guided video-assisted thoracoscopic resection after computed tomography-guided localization using platinum microcoils. Ann Surg 2004;240:481-8; discussion 488-9. [Crossref] [PubMed]
- Dendo S, Kanazawa S, Ando A, et al. Preoperative localization of small pulmonary lesions with a short hook wire and suture system: experience with 168 procedures. Radiology 2002;225:511-8. [Crossref] [PubMed]
- Moon SW, Cho DG, Cho KD, et al. Fluoroscopy-assisted thoracoscopic resection for small intrapulmonary lesions after preoperative computed tomography-guided localization using fragmented platinum microcoils. Thorac Cardiovasc Surg 2012;60:413-8. [Crossref] [PubMed]
- Lee NK, Park CM, Kang CH, et al. CT-guided percutaneous transthoracic localization of pulmonary nodules prior to video-assisted thoracoscopic surgery using barium suspension. Korean J Radiol 2012;13:694-701. [Crossref] [PubMed]
- McArthur CS, Roayaie S, Waye JD. Safety of preoperation endoscopic tattoo with india ink for identification of colonic lesions. Surg Endosc 1999;13:397-400. [Crossref] [PubMed]
- Price N, Gottfried MR, Clary E, et al. Safety and efficacy of India ink and indocyanine green as colonic tattooing agents. Gastrointest Endosc 2000;51:438-42. [Crossref] [PubMed]
- Trakarnsanga A, Akaraviputh T. Endoscopic tattooing of colorectal lesions: Is it a risk-free procedure? World J Gastrointest Endosc 2011;3:256-60. [Crossref] [PubMed]
- Yeung JM, Maxwell-Armstrong C, Acheson AG. Colonic tattooing in laparoscopic surgery - making the mark? Colorectal Dis 2009;11:527-30. [Crossref] [PubMed]
- Magistrelli P, D'Ambra L, Berti S, et al. Use of India ink during preoperative computed tomography localization of small peripheral undiagnosed pulmonary nodules for thoracoscopic resection. World J Surg 2009;33:1421-4. [Crossref] [PubMed]
- Kim YD, Jeong YJ. Localization of pulmonary nodules with lipiodol prior to thoracoscopic surgery. Acta Radiol 2011;52:64-9. [Crossref] [PubMed]
- Nomori H, Horio H, Naruke T, et al. Fluoroscopy-assisted thoracoscopic resection of lung nodules marked with lipiodol. Ann Thorac Surg 2002;74:170-3. [Crossref] [PubMed]
- Watanabe K, Nomori H, Ohtsuka T, et al. Usefulness and complications of computed tomography-guided lipiodol marking for fluoroscopy-assisted thoracoscopic resection of small pulmonary nodules: experience with 174 nodules. J Thorac Cardiovasc Surg 2006;132:320-4. [Crossref] [PubMed]
- Kawanaka K, Nomori H, Mori T, et al. Marking of small pulmonary nodules before thoracoscopic resection: injection of lipiodol under CT-fluoroscopic guidance. Acad Radiol 2009;16:39-45. [Crossref] [PubMed]
- Jin KN, Lee KW, Kim TJ, et al. Computed tomography guided percutaneous injection of a mixture of lipiodol and methylene blue in rabbit lungs: evaluation of localization ability for video-assisted thoracoscopic surgery. J Korean Med Sci 2014;29:129-36. [Crossref] [PubMed]
- Shi Z, Chen C, Jiang S, et al. Uniportal video-assisted thoracic surgery resection of small ground-glass opacities (GGOs) localized with CT-guided placement of microcoils and palpation. J Thorac Dis 2016;8:1837-40. [Crossref] [PubMed]


