Predictors of length of stay and duration of tracheal intubation after transcatheter aortic valve implantation
Introduction
During the last decade, there has been a scientific interest focused on transcatheter aortic valve implantation (TAVI) as an acceptable alternative therapeutic option for patients, with a high surgical risk, even those who are inoperable, and with severe symptomatic aortic valve disease (1,2). Several different approaches can be used to conduct a TAVI procedure, including a retrograde transfemoral, trans-subclavian, transaortic and anterograde transapical (1).
The main benefit of the TAVI procedure concerns inoperable patients, who constitute a significant proportion of the general population of patients with severe aortic stenosis (3). The avoidance of the risks of sternotomy, cardiopulmonary bypass and aortic cross clamping is advantageous for patients at high risk (2). There is strong evidence that the TAVI procedure is superior to medical management in terms of survival (4), symptomatic outcomes (4,5), quality of life (5,6) and healthcare cost (7-9). In addition, according to the Euroheart Survey, almost a third of these patients do not undergo surgical aortic valve replacement (AVR) due to the extremely high perioperative risk, with the potential of excess complications and morbidity rates (10). This data could interpret the necessity and the growing number of patients undergoing TAVI each year, worldwide, despite the lack of robust evidence for the superiority of TAVI comparing with the conventional surgical AVR (3,11,12) and the limited expansion of TAVI into lower risk populations due to complications and costs (3,13).
Although mortality and length of stay (LOS) have long been studied for TAVI procedure (14-17), few are known to regard the predictors of these short-term outcomes. Additionally, to the best of our knowledge, concerning the post-procedural duration of tracheal intubation, there is a lack of available literature and research data. The aim of this study was to identify the predictors of higher in-hospital mortality rates, prolonged LOS and increased tracheal intubation time amongst patients who underwent TAVI. Our study intends to add new data to TAVI outcomes body of knowledge and to strengthen the importance of the early identification of patients at high risk for adverse or poor periprocedural outcomes.
Methods
Study design and participants
A retrospective cohort study was conducted. During a 5-year period (September 2008–October 2013), 164 consecutive patients with aortic valve disease were admitted to our cardiothoracic surgery center in Liverpool, United Kingdom for TAVI procedure under general anaesthesia. All patients were implanted with the Edwards SAPIEN-XT valve (Edwards Lifesciences Inc., Irvine, California). Two patients required conversion to an open surgical AVR and were excluded from our study. The final sample of our study consisted of 162 patients (response rate 98.8%) with successful implantation.
Data collection
The collection of data took place in November 2014. We used the hospital’s structured database (e-cardiac), which included basic demographic and perioperative patient data for data collection purposes. The obtained information included patients’ age, gender, height, weight, logistic EuroSCORE, the TAVI approach (transapical or transfemoral), comorbidity (diabetes mellitus, hypercholesterolemia, chronic renal insufficiency), cardiac patient history (Q wave myocardial infarction, previous cardiac surgery, preoperative coronary angiography, preoperative cardiac rhythm, left ventricular ejection fraction, oral inotropic therapy), smoking status, preoperative serum creatinine (Cr) levels, duration both of the postoperative tracheal intubation and the perioperative inotropic support, LOS in the intensive care unit (ICU) and in hospital, and the cases of in-hospital death (in-hospital mortality).
ICU LOS was estimated from the time of the TAVI procedure to the ICU discharge and the in-hospital LOS from the time of the TAVI procedure to the hospital discharge. Tracheal intubation time was the duration (in hours), of tracheal intubation (if present) from ICU admission to tracheal extubation. For these variables, values below the median were considered as normal and values above the median were considered as increased or prolonged. Additionally, in-hospital mortality represented the case of patient death, postoperatively, and during his/her hospitalization. Aiming to ensure the reliability and validity of the data collection process, a single researcher obtained the data based on medical and nursing patient records review.
Statistical analysis
Continuous variables are presented as median and interquartile range (IQR), while categorical variables are presented as absolute and relative frequencies. Continuous variables that were extremely skewed were converted into binary variables using median values as the criterion for separation. For BMI the criterion for separation was the international limit of 24.9 kg/m2, while for serum Cr levels the cut-off point was defined at 1.4 mg/dL, a value that constitutes the limit between the normal and the increased Cr levels of the biochemistry laboratory of the hospital in which our study was conducted. Chi-square test, Fisher’s exact test and chi-square trend test were used to identify differences between groups. Student’s t-test was used to compare a continuous variable with a dichotomous. Variables that were significantly different (P<0.20) in bivariate analyses were entered into the backward stepwise multivariate logistic regression analysis. We estimated adjusted odds ratios (ORs) with 95% confidence intervals (CIs) for the independent variables included in the model. P values of less than 0.05 were considered significant. Statistical analysis was performed using the IBM SPSS 21.0 (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp).
Ethics
As there was no randomization, no new treatment being explored and no potential harm to the patients there was no need for ethical approval by the ethics committee of the “Heart and Chest Hospital” of Liverpool, United Kingdom. The investigation was carried out in accordance with the ethical standards of the responsible institutional committee for human experimentation and with the Helsinki Declaration of 1975, as revised in 2013.
Results
The median (IQR) age of our patients was 84 [9] years old and female subjects constituted the majority (53.1%) of our cohort. Ninety patients (55.6%) underwent TAVI through a transapical approach and 72 (44.4%) through a transfemoral approach. The median (IQR) duration of hospitalization in the ICU and in-hospital was 1 [2] and 7 [7] days, respectively. Patients remain intubated for a median (IQR) of 0 [2] hours postoperatively and the overall in-hospital mortality was 3.7%. The main socio-demographic, clinical and surgical patient characteristics and outcomes are depicted in Table 1.
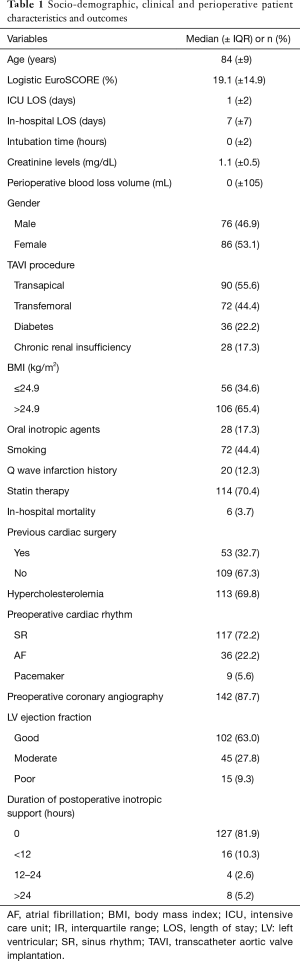
Full table
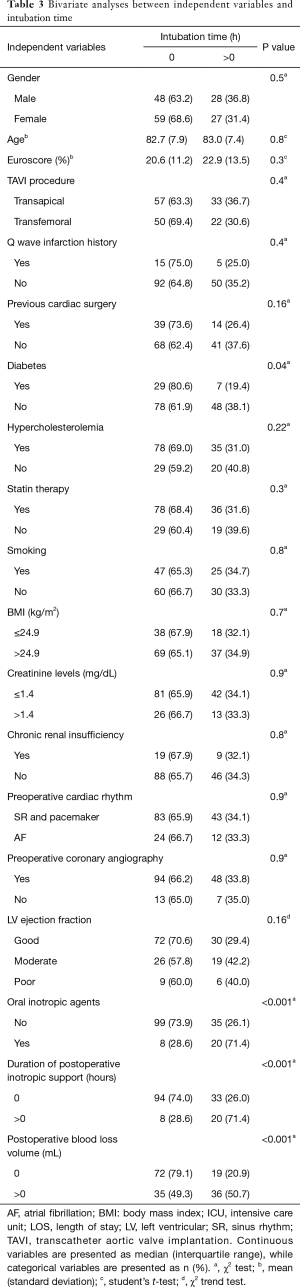
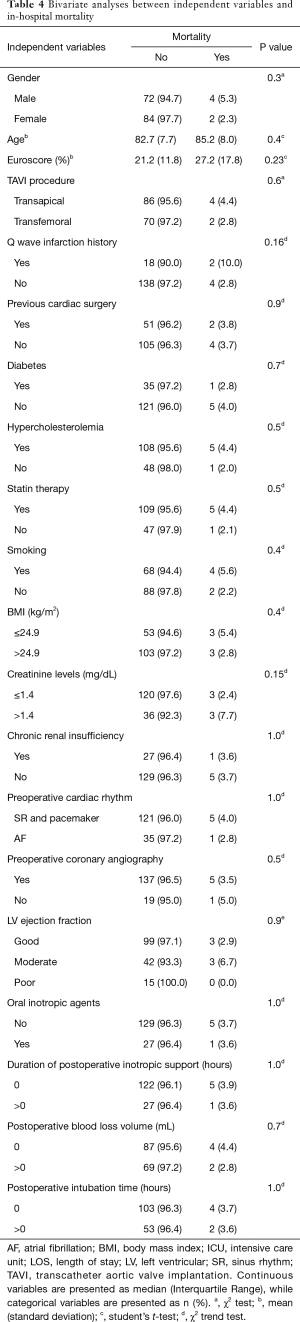
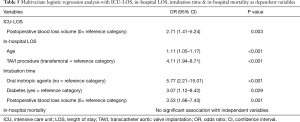
Tables 2-4 provide the main predictors of prolonged ICU LOS, in-hospital LOS and intubation time resulting from bivariate analysis. Table 5 summarizes the main findings of the logistic regression analysis. Any postoperative bleeding was the multivariate predictor of ICU-LOS longer than 1 day. In addition, older age and transapical TAVI procedure were the main independent multivariate predictors of prolonged in-hospital LOS. More analytically, older patients and those who underwent transapical TAVI procedure had an almost 1.11 and 4.11 greater probability to stay in-hospital longer than 7 days. Finally, history of oral inotropic therapy, history of non-diabetic status and postoperative volume of blood loss greater than 0 mL were the main independent predictors of increased postoperative intubation time, as resulting from multivariate analysis. Multivariate analysis did not indicate statistically significant predictors of high in-hospital mortality of TAVI patients.
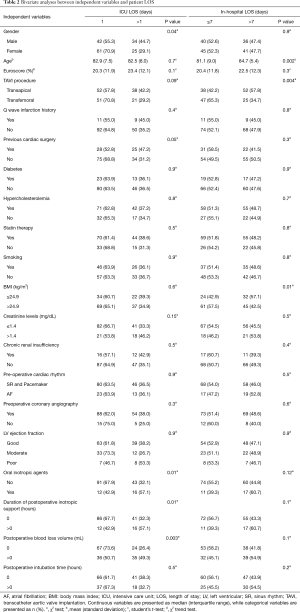
Full table
Full table
Full table
Full table
Discussion
The main findings of the present study were the identification of the independent predictors of longer postoperative hospitalization and tracheal intubation for patients undergoing TAVI. Patients undergoing transapical TAVI had an almost 4.11 times greater probability to stay in hospital longer than 7 days compared with those who underwent TAVI through transfemoral approach. Additionally, older age was a strong predictor for prolonged in-hospital LOS. Postoperative blood loss was a main predictor for ICU LOS and postoperative tracheal intubation time longer than 1 day and 0 hours, respectively. Furthermore, non-diabetics and patients who use oral inotropic agents preoperatively had an almost 3.07 and 5.77 greater probability to remain intubated after TAVI procedure completion. Finally, multivariate analysis did not reveal any predictor of in-hospital mortality.
Our study highlighted the superiority of transfemoral compared with transapical TAVI with respect to postoperative in-hospital LOS. In line with our results is the multicenter study conducted by van der Boon et al. (18) that found significantly longer in-hospital LOS in the transapical TAVI group. Transfemoral TAVI is a less invasive technique, which avoids microthoracotomy and left ventricular puncture, and has lower risk for periprocedural complications (13) which can affect negatively the patient length of hospitalization. In addition, patients with greater clinical severity and more comorbidities such as significant peripheral vascular disease, tortuous or relatively smaller diameter femoral or iliac vessels, calcified vessels and/or unfavorable aortic anatomy are preferred to have TAVI with transapical approach (13).
In addition, older age was a strong predictor for increased in-hospital LOS. Older age is a well establish risk factor for greater clinical severity, hemodynamic instability prolonged mechanical ventilation and more adverse events, which could interpret the previous association and the need for keeping these patients in hospital for longer (19,20).
As aforementioned, any postoperative bleeding was the independent predictor of prolonged ICU-LOS for TAVI patients. In line with our results and according to the study of Barbanti et al. (16) patients undergoing transfemoral TAVI with any periprocedural bleeding were less likely to be associated with early hospital discharge, shorter than 3 days. However, in contrast with our study, the investigators did not examine potential predictors for early or late ICU discharge. In addition, Borz et al. (21) stated that life-threatening bleeding was associated with prolonged in-hospital LOS after TAVI. Bleeding can lead to hemodynamic instability and the need for close monitoring in the ICU, accompanied by specialized interventions aiming to effective and immediate blood loss management.
Although, postprocedural ICU and in-hospital LOS are significant morbidity indexes (22) and among the main factors contributing to increase in periprocedural costs of TAVI (16), in the currently available literature, there is little published data on predictors of LOS, either in the ICU or in hospital, among TAVI patients series. Contrary to our results, parameters such as the New York Association (NYHA) class IV (16), the year of procedure (16), the presence of a permanent pacemaker (16,17), the presence of acute kidney injury (17) and the need for blood transfusions postoperatively (17), have been reported as independent predictors of in-hospital LOS. To the best of our knowledge, our study was the first one investigating potential predictors of longer ICU-LOS a parameter of high significance regarding the periprocedural healthcare costs and expenditures of TAVI.
Another important finding of this study was the independent predictors of mechanical ventilatory support postoperatively. Patients with heart failure of advanced NYHA class use positive oral inotropic agents. The impaired cardiac function of these, end-stage heart failure, patients affects negatively their pulmonary function and constitutes the rationale for the need of tracheal intubation and ventilator support after TAVI procedure. Additionally, patients with any bleeding during the periprocedural period are characterized by high clinical severity and more unstable condition with hemodynamic alterations and probably required more time to optimize their postoperative respiratory function.
An interesting result of our study was that non-diabetics had an almost 3.07 times greater probability to remain intubated after TAVI procedure compared with those with history of diabetes mellitus. Based on the strong association between diabetes and poor perioperative outcomes (23), the above finding cannot be clearly interpreted and could be explained only by the relatively small sample size of our study. Indeed, contrary to our results, Puls et al. (24) underlined that diabetic patients who underwent TAVI had prolonged mechanical ventilation compared with non-diabetics.
Finally, our study failed to reveal any predictor of in-hospital mortality among TAVI patients. Contrary to our results, a recent meta-analysis of 2,978 patients who underwent either transfemoral (n=1,465) or transapical (n=1,513) TAVI found significantly higher 30-day and 1-year all-cause (when modulated by logistic EuroSCORE) mortality for the transapical TAVI group compared with the transfemoral group (13). In addition, as highlighted by Moat et al. (14) patients receiving a non-transfemoral implant had significantly higher 30-day mortality than patients receiving a transfemoral TAVI. van der Boon et al. (18) concluded in similar results, and a recent study of Badheka et al. (25) showed that higher annual hospital volumes, that is to say higher number of TAVI procedures per year, are significantly predictive of reduced postprocedural mortality. Moreover and in contrast with our findings, Tamburino et al. (15) in their study underlined that conversion to open heart surgery, cardiac tamponade, major access site complications, left ventricular ejection fraction less than 40%, prior valvuloplasty and diabetes mellitus were the independent predictors of 30-day mortality among 663 TAVI patients.
On the other hand and in line with our findings, Barbanti et al. (16) observed no significant differences in terms of 30-day mortality in patients with significantly different in-hospital LOS, who had been divided in two groups, the early and the late discharge group, respectively. It is worth mentioning that the overall in-hospital mortality in our patients was 3.7%, a rate equivalent with (16) or lower than the early mortality rates of other studies (12,25).
The present study adds important information to the limited body of knowledge regarding the independent predictors of prolonged postprocedural in-hospital LOS among TAVI patients. In addition, this is, to the best of our knowledge, the first study investigating predictors of prolonged ICU-LOS and postoperative mechanical ventilatory support for this patient population. However, our study has some limitations. Specifically, this was a single centre study with retrospective design and small sample size. In addition, we had a lack of long term follow up data, as well as a low flow of patients. These limitations restrict the generalization of the findings to the general TAVI patient population and affect the validity of the study. Based on these limitations, further research is needed.
Conclusions
In conclusion, our findings suggest the early identification of TAVI patients at high risk for poor short-term outcomes, such as longer hospitalization and increased mechanical ventilatory support postoperatively. This piece of information is crucial for clinicians and administrators because it could contribute to more efficient patient care planning and better allocation of the limited, human and financial, healthcare resources.
Taking measures for the prevention of postoperative bleeding could contribute to shorter ICU stay and postoperative intubation time. Knowing older patients and those who underwent TAVI through transapical approach are at higher risk for prolonged postprocedural in-hospital LOS, clinicians could prepare and develop more efficient plans for patient care with better healthcare resource allocation and could be a crucial piece of information for healthcare cost saving. Furthermore, data obtained from patient history such as non-diabetic status and pharmaceutical therapy with oral inotropic agents could predict the patients who are going to remain intubated postoperatively and assist clinicians to perform preventive measures for complications associated with mechanical ventilation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The investigation was carried out in accordance with the ethical standards of the responsible institutional committee for human experimentation and with the Helsinki Declaration of 1975, as revised in 2013.
References
- Rahnavardi M, Santibanez J, Sian K, et al. A systematic review of transapical aortic valve implantation. Ann Cardiothorac Surg 2012;1:116-28. [PubMed]
- Duncan AM, Moat NE. Transcatheter aortic valve implantation in the elderly. Aging Health 2012;8:479-91. [Crossref]
- Cao C, Bannon P, Yan TD. Transcatheter aortic valve implantation: clinical evidence versus clinical practice. J Thorac Cardiovasc Surg 2013;145:615-6. [Crossref] [PubMed]
- Leon MB, Smith CR, Mack M, et al. Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. N Engl J Med 2010;363:1597-607. [Crossref] [PubMed]
- Gonçalves A, Marcos-Alberca P, Almeria C, et al. Quality of life improvement at midterm follow-up after transcatheter aortic valve implantation. Int J Cardiol 2013;162:117-22. [Crossref] [PubMed]
- Elmalem S, Dumonteil N, Marcheix B, et al. Health-related quality of life after transcatheter aortic valve implantation in elderly patients with severe aortic stenosis. J Am Med Dir Assoc 2014;15:201-6. [Crossref] [PubMed]
- Reynolds MR, Magnuson EA, Wang K, et al. Cost-effectiveness of transcatheter aortic valve replacement compared with standard care among inoperable patients with severe aortic stenosis: results from the placement of aortic transcatheter valves (PARTNER) trial (Cohort B). Circulation 2012;125:1102-9. [Crossref] [PubMed]
- Doble B, Blackhouse G, Goeree R, et al. Cost-effectiveness of the Edwards SAPIEN transcatheter heart valve compared with standard management and surgical aortic valve replacement in patients with severe symptomatic aortic stenosis: a Canadian perspective. J Thorac Cardiovasc Surg 2013;146:52-60.e3. [Crossref] [PubMed]
- Indraratna P, Ang SC, Gada H, et al. Systematic review of the cost-effectiveness of transcatheter aortic valve implantation. J Thorac Cardiovasc Surg 2014;148:509-14. [Crossref] [PubMed]
- Shroyer AL, Coombs LP, Peterson ED, et al. The Society of Thoracic Surgeons: 30-day operative mortality and morbidity risk models. Ann Thorac Surg 2003;75:1856-64; discussion 1864-5.
- Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med 2011;364:2187-98. [Crossref] [PubMed]
- Cao C, Ang SC, Indraratna P, et al. Systematic review and meta-analysis of transcatheter aortic valve implantation versus surgical aortic valve replacement for severe aortic stenosis. Ann Cardiothorac Surg 2013;2:10-23. [PubMed]
- Panchal HB, Ladia V, Amin P, et al. A meta-analysis of mortality and major adverse cardiovascular and cerebrovascular events in patients undergoing transfemoral versus transapical transcatheter aortic valve implantation using edwards valve for severe aortic stenosis. Am J Cardiol 2014;114:1882-90. [Crossref] [PubMed]
- Moat NE, Ludman P, de Belder MA, et al. Long-term outcomes after transcatheter aortic valve implantation in high-risk patients with severe aortic stenosis: the U.K. TAVI (United Kingdom Transcatheter Aortic Valve Implantation) Registry. J Am Coll Cardiol 2011;58:2130-8. [Crossref] [PubMed]
- Tamburino C, Capodanno D, Ramondo A, et al. Incidence and predictors of early and late mortality after transcatheter aortic valve implantation in 663 patients with severe aortic stenosis. Circulation 2011;123:299-308. [Crossref] [PubMed]
- Barbanti M, Capranzano P, Ohno Y, et al. Early discharge after transfemoral transcatheter aortic valve implantation. Heart 2015;101:1485-90. [Crossref] [PubMed]
- Durand E, Eltchaninoff H, Canville A, et al. Feasibility and safety of early discharge after transfemoral transcatheter aortic valve implantation with the Edwards SAPIEN-XT prosthesis. Am J Cardiol 2015;115:1116-22. [Crossref] [PubMed]
- van der Boon RM, Marcheix B, Tchetche D, et al. Transapical versus transfemoral aortic valve implantation: a multicenter collaborative study. Ann Thorac Surg 2014;97:22-8. [Crossref] [PubMed]
- Makary MA, Segev DL, Pronovost PJ, et al. Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 2010;210:901-8. [Crossref] [PubMed]
- Markle-Reid M, Browne G. Conceptualizations of frailty in relation to older adults. J Adv Nurs 2003;44:58-68. [Crossref] [PubMed]
- Borz B, Durand E, Godin M, et al. Incidence, predictors and impact of bleeding after transcatheter aortic valve implantation using the balloon-expandable Edwards prosthesis. Heart 2013;99:860-5. [Crossref] [PubMed]
- Giakoumidakis K, Baltopoulos GI, Charitos C, et al. Risk factors for prolonged stay in cardiac surgery intensive care units. Nurs Crit Care 2011;16:243-51. [Crossref] [PubMed]
- Serio S, Clements JM, Grauf D, et al. Outcomes of diabetic and nondiabetic patients undergoing general and vascular surgery. ISRN Surg 2013;2013:963930. [Crossref] [PubMed]
- Puls M, Bleckmann A, Jacobshagen C, et al. Diabetes increases short- and long-term mortality after transcatheter aortic valve implantation (TAVI). Dtsch Med Wochenschr 2014;139:822-8. [PubMed]
- Badheka AO, Patel NJ, Panaich SS, et al. Effect of Hospital Volume on Outcomes of Transcatheter Aortic Valve Implantation. Am J Cardiol 2015;116:587-94. [Crossref] [PubMed]


