Hybrid approach of percutaneous coronary intervention followed by minimally invasive mitral valve surgery: a 5-year single-center experience
Introduction
In patients with concomitant coronary artery and mitral valve (MV) disease, performing combined coronary artery bypass grafting (CABG) with MV surgery confers a higher risk of mortality when compared with isolated MV repair or replacement (1,2). In these patients, one may attempt to reduce the operative risk by performing two smaller, lower risk procedures. This “hybrid” staged approach consists of percutaneous coronary intervention (PCI) to treat the coronary artery disease, and a minimally invasive approach for the MV surgery. The use of PCI in treating the coronary artery disease permits the use of minimally invasive surgical techniques, obviating the need for a median sternotomy and CABG (3).
The benefits of minimally invasive mitral valve surgery (MIMVS) include improved cosmesis, fewer blood transfusions, less pain, less wound infections, shorter ventilation time, shorter hospital length of stay, an enhanced post-operative recovery, and lower costs, when compared with a conventional sternotomy approach (4-8). In the setting of coronary artery and valvular disease, the less invasive approach of PCI plus minimally invasive valve surgery has demonstrated excellent early and mid-term outcomes (9-17). However, the data evaluating the use of PCI for coronary artery disease prior to isolated MV surgery (PCI + MIMVS) are limited. We report our 5-year single center experience utilizing this technique.
Methods
The Mount Sinai Medical Center (Miami Beach, FL, USA) Institutional Review Board approved the study, and patients were enrolled in our institutional Society of Thoracic Surgeons (STS) Database after written informed consent was obtained. The study was a retrospective review of all patients with combined coronary artery and MV disease who underwent hybrid PCI + MIMVS between February 2009 and April 2014. Baseline variables, operative characteristics and outcomes, and major adverse cardiovascular events during the follow-up period were analyzed using our institutional electronic medical records, outpatient surgical and cardiology office visits, and a follow-up survey at 6-month intervals.
Excluded were patients with endocarditis, those who underwent a procedure on another valve, or had a procedure on the aorta. A hybrid approach for intervention was selected after a comprehensive Heart Valve Team evaluation, which included calculation of the STS predicted risk of morbidity and mortality or EuroSCORE II (European System for Cardiac Operative Risk Evaluation), incorporation of the SYNTAX (Synergy Between PCI With Taxus and Cardiac Surgery) score to determine the suitability of PCI for the coronary disease, and individual patient co-morbidity and preference (18,19). Dual antiplatelet therapy with clopidogrel (600 mg) and aspirin (325 mg) was commenced after coronary stenting in all patients, followed by clopidogrel 75 mg and aspirin 81 mg daily thereafter. All patients resumed their antiplatelet regimen within 24 to 48 hours after surgery.
The technique for MIMVS performed at our institutions has been previously described (20). In summary, a right thoracotomy was performed via a 5–6 cm skin incision made in the 4–5th intercostal space lateral to the anterior axillary line and, subsequently, the MV was accessed via a standard left atriotomy. A chordal-sparing technique was utilized for MV replacement, with preservation of the posterior leaflet and chords with anterior leaflet excision, or preservation of both leaflets when feasible. The MV repairs were performed with reconstructive techniques tailored to the specific MV lesion, and sizing of the annuloplasty ring was based on the height or surface area of the anterior mitral leaflet.
Statistical analysis
The variables are reported as the mean ± standard deviation (SD), median and interquartile range (IQR, 25–75%), or number (N) and percentage. Follow-up survival was estimated with a Kaplan-Meier analysis. The Statistical Package for Social Sciences, version 21 (SPSS Inc., Chicago, IL) was used for all statistical analyses.
Results
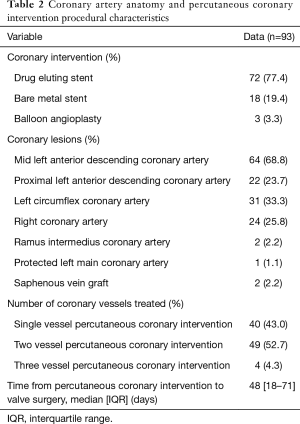
There were 93 patients identified who underwent PCI + MIMVS, of which there were 54 men (58.1%) and 39 women (41.9%), with a mean age of 73±8 years. All patients had severe mitral regurgitation, and the median left ventricular ejection fraction was 55% (IQR, 40–62%). There were 15 (16.1%) patients with a history of previous cardiac surgery. The etiology of mitral regurgitation was primary in 59 (63.4%), secondary (ischemic) in 29 (31.2%), and 5 (5.4%) patients had prosthetic MV regurgitation. The majority of patients (84%) had their PCI and valve surgery performed in two separate hospital admissions, while the remaining 16% had both procedures done within the same hospital stay. The median time interval between PCI and surgery was 48 days (IQR, 18–71) (Table 1). Single-, two-, and three-vessel PCI was performed in 40 (43%), 49 (52.7%), and 4 (4.3%) patients, respectively. The most commonly treated coronary arteries were the mid-left anterior descending in 64 (68.8%) patients, the proximal left anterior descending in 22 (23.7%), the right coronary in 24 (25.8%), and the left circumflex in 31 (33.3%), with the majority of patients receiving drug-eluting stents (77.4%) (Table 2).

Full table
Full table
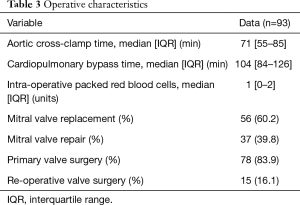
At surgery, 65 (69.9%) patients were on dual anti-platelet therapy. There were 78 (83.9%) who underwent primary surgery, and 15 (16.1%) who underwent re-operative valve surgery, which consisted of 56 (60.2%) MV replacements, and 37 (39.8%) MV repairs. The median aortic cross-clamp and cardiopulmonary bypass times were 71 minutes (IQR, 55–85) and 104 minutes (IQR, 84–126), respectively. Intra-operatively, a median of 1 unit of packed red blood cells was transfused (IQR, 0–2). There were 2 (2.2%) patients that required conversion to median sternotomy due to poor surgical field exposure (Table 3).
Full table
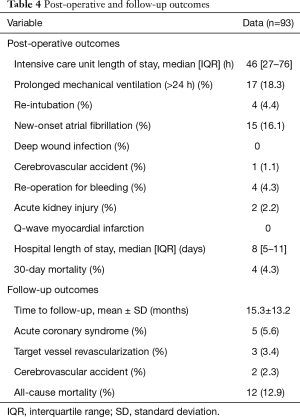
The median intensive care unit and hospital length of stay, which included the time frame for the PCI, was 46 hours (IQR, 27–76) and 8 days (IQR, 5–11), respectively. The post-operative complications included 17 (18.3%) prolonged mechanical ventilation (>24 h), 15 (16.1%) post-operative atrial fibrillation, 1 (1.1%) cerebrovascular accident, 4 (4.4%) re-operations for bleeding, and 2 (2.2%) patients with acute kidney injury. Thirty-day mortality occurred in 4 (4.3%) patients, as a result of: 1 cerebrovascular accident, 1 cardiogenic shock, 1 sepsis, and 1 multi-organ failure (Table 4).
Follow-up was 100% complete. At a mean of 15.3±13.2 months post-operatively, 5 (5.7%) patients had an acute coronary syndrome, of which 3 (3.4%) required target-vessel revascularization. Cerebrovascular accidents and renal insufficiency occurred in 2 (2.3%) patients each (Table 4). There were 8 more deaths that occurred during the time frame of the study, and the actuarial survival was 89% and 85% at 1 and 3 years, respectively.
Full table
Discussion
The STS adult cardiac surgery database cites the operative mortality of isolated MV repair at 1.1%, and MV replacement at 4.7% (1). When performing concomitant CABG, the operative mortality increases to 4.1% for repair and 9.8% for replacement, with a significantly greater occurrence of post-operative complications. Thus, it is hypothesized that the operative risk of combined CABG and MV surgery may be reduced by partitioning the operation into the two lower-risk procedures of PCI + MIMVS. The present study demonstrated a low morbidity and mortality with hybrid PCI + MIMVS for significant coronary artery and MV disease, with the majority of patients having multi-vessel PCI and subsequently undergoing primary or re-operative surgery.
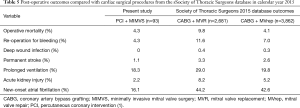
Although one needs to be cautious when making direct comparison with other studies, reductions in the parameters of morbidity were noted when compared with data from the most recent STS adult cardiac surgery database outcomes. In patients undergoing CABG plus MV repair or replacement, the most common complication is new-onset atrial fibrillation, which occurs in 42.6% and 44.2%, respectively, and increases peri-operative morbidity and hospital length of stay (21,22). This figure is higher than the 16.1% noted in present cohort of PCI + MIMVS, and is consistent with prior studies suggesting a reduced incidence of post-operative atrial fibrillation when utilizing a minimally invasive approach for valve surgery (23,24). Similarly, prolonged mechanical ventilation occurred in 18.3% of the PCI + MIMVS cohort, with a reported incidence of 19.8% in CABG plus MV repair, and 29% in CABG plus MV replacement. By virtue of avoiding a sternotomy, minimally invasive surgery results in less thoracic surgical trauma and alterations in pulmonary physiology and biomechanics, which contributes to an enhanced post-operative recovery and faster extubation (8,12,25). The prevalence of additional parameters of peri-operative morbidity is outlined in Table 5.
Full table
Attempting to reduce the operative risk of combined CABG and valve surgery by performing PCI and valve surgery has been evaluated in different clinical scenarios, which have included the use of a median sternotomy or minimally invasive approach, as well as application in primary or re-operative single or double valve surgery (17). Leacche et al. reported the outcomes of 39 high-risk patients who underwent PCI + MIMVS via a right thoracotomy (26). Of the 39 patients, 5 (13%) presented with acute coronary syndrome, 19 (49%) were in congestive heart failure, 16 (41%) underwent urgent or emergent surgery, and 16 (41%) were re-operations. Thirty (77%) patients underwent a single staged procedure of PCI + MIMVS in a hybrid operating room, while the remaining 9 (23%) had a two-staged procedure of PCI 1 to 4 days prior to MIMVS. Operative mortality occurred in 1 (2.6%) patient, which was lower than the STS predicted mortality of 14%. A subsequent study by our group evaluated the outcomes of 31 patients treated with hybrid PCI + MIMVS via a right thoracotomy for coronary artery disease and severe ischemic mitral regurgitation (15). Of note, 29 of these patients underwent isolated MV surgery, and are included in the current analysis. The mean left ventricular ejection fraction was 35%±11%, all patients were in New York Heart Association functional class III or IV, and 4 (13%) were re-operations. Single and two-vessel PCI was performed in 22 (77%) and 9 (29%) patients, respectively. There were 18 (58%) MV repairs and 13 (42%) replacements performed, with concomitant tricuspid valve repair in 2 (6%) patients, and papillary muscle approximation in 5 (16%). The 30-day mortality was 3%. At a mean follow-up of 2.4±1.6 years, 2 (6%) patients required PCI for target-vessel revascularization. Survival was 84% and 80% at 1 and 5 years, respectively, demonstrating excellent short and mid-term outcomes.
The most recent data from STS demonstrate that in those undergoing isolated MV surgery, the rate of MV repair was 57.4%, and MV replacement was 42.6% (2). In the cases where MV pathology and etiology were documented, 56.6% were identified as having mitral regurgitation due to annular or degenerative disease, without stenosis, of which repair was performed in 75.0% of patients. In the present study, the repair rate was 39.8%, with the MV being replaced in 60.2% of the cases. While the reason for the lower repair rate cannot be clearly deduced, it should be noted that the etiology of mitral regurgitation was mixed. Primary mitral regurgitation consisted of patients with degenerative, calcific, or rheumatic disease and the reparability of these pathologies varies markedly. Additionally, one-third of population consisted of secondary (ischemic) mitral regurgitation, and 5.4% had prosthetic MV insufficiency, in whom the only option was MV re-replacement.
The primary limitation of the present study is its retrospective nature, and the associated potential for treatment selection bias. This includes the selection process for PCI + MIMVS, which was dependent upon a suitable coronary anatomy for PCI. Importantly, the study was clinically driven and did not follow a protocol, which may be more representative of the practice patterns of community interventional cardiologists. All procedures were elective and the operation consisted of isolated MV surgery, and as such, the outcomes presented herein cannot be extrapolated to other clinical scenarios. Finally, given the observational nature of the analyses and lack of a comparison group undergoing CABG plus MV surgery, the data are best interpreted as providing evidence for the safety and feasibility of hybrid PCI + MIMVS for select patients with combined coronary artery and isolated MV disease requiring surgical intervention.
In conclusion, a hybrid approach of PCI + MIMVS can be performed safely in the setting of coronary artery and MV disease, and is associated with good short and follow-up outcomes. This includes patients with single or multi-vessel coronary artery disease, and those undergoing primary or re-operative MV surgery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This retrospective study was approved by the Institutional Review Board at the Mount Sinai Medical Center, Miami Beach, Florida, USA.
References
- D'Agostino RS, Jacobs JP, Badhwar V, et al. The Society of Thoracic Surgeons adult cardiac surgery database: 2017 update on outcomes and quality. Ann Thorac Surg 2017;103:18-24. [PubMed]
- Badhwar V, Rankin JS, He X, et al. The Society of Thoracic Surgeons mitral repair/replacement composite score: a report of the Society of Thoracic Surgeons quality measurement task force. Ann Thorac Surg 2016;101:2265-71. [PubMed]
- Greelish JP, Ailiwadi M, Balaguer JM, et al. Combined percutaneous coronary intervention and valve surgery. Curr Opin Cardiol 2006;21:113-17. [PubMed]
- Schmitto JD, Mokashi SA, Cohn LH. Minimally-invasive valve surgery. J Am Coll Cardiol 2010;56:455-62. [PubMed]
- Cheng DC, Martin J, Lal A, et al. Minimally invasive versus conventional open mitral valve surgery: a meta-analysis and systematic review. Innovations (Phila) 2011;6:84-103. [PubMed]
- Nagendran J, Catrip J, Losenno KL, et al. Minimally invasive mitral repair surgery: why does controversy still persist? Expert Rev Cardiovasc Ther 2017;15:15-24. [PubMed]
- Santana O, Larrauri-Reyes M, Zamora C, et al. Is a minimally invasive approach for mitral valve surgery more cost-effective than median sternotomy? Interact CardioVasc Thorac Surg 2016;22:97-100. [PubMed]
- Mihos CG, Santana O, Lamas GA, et al. Outcomes of right mini-thoracotomy mitral valve surgery in patients with previous sternotomy. Ann Thorac Surg 2011;91:1824-27. [PubMed]
- Byrne JG, Leacche M, Unic D, et al. Staged initial percutaneous coronary intervention followed by valve surgery ("hybrid approach") for patients with complex coronary and valve disease. J Am Coll Cardiol 2005;45:14-18. [PubMed]
- Brinster DR, Byrne M, Rogers CD, et al. Effectiveness of same day percutaneous coronary intervention followed by minimally invasive aortic valve replacement for aortic stenosis and moderate coronary disease ("hybrid approach"). Am J Cardiol 2006;98:1501-03. [PubMed]
- Umakanthan R, Leacche M, Petracek MR, et al. Combined PCI and minimally invasive heart valve surgery for high-risk patients. Curr Treat Options Cardiovasc Med 2009;11:492-98. [PubMed]
- Santana O, Funk M, Zamora C, et al. Staged percutaneous coronary intervention and minimally invasive valve surgery: Results of a hybrid approach to concomitant coronary and valvular disease. J Thorac Cardiovasc Surg 2012;144:634-39. [PubMed]
- Santana O, Pineda AM, Cortes-Bergoderi M, et al. Hybrid approach of percutaneous coronary intervention followed by minimally invasive valve operations. Ann Thorac Surg 2014;97:2049-55. [PubMed]
- George I, Nazif TM, Kalesan B, et al. Feasibility and early safety of single-stage hybrid coronary intervention and valvular cardiac surgery. Ann Thorac Surg 2015;99:2032-37. [PubMed]
- Mihos CG, Santana O, Pineda AM, et al. Percutaneous coronary intervention followed by minimally invasive mitral valve surgery in ischemic mitral regurgitation. Innovations (Phila) 2015;10:394-7. [PubMed]
- Pineda AM, Chandra R, Gowani SA, et al. Completeness of revascularization and its impact on the outcomes of a staged approach of percutaneous coronary intervention followed by minimally invasive valve surgery for patients with concomitant coronary artery and valvular heart disease. Catheter Cardiovasc Interv 2016;88:329-37. [PubMed]
- Santana O, Singla S, Mihos CG, et al. Outcomes of the hybrid approach of combined percutaneous coronary revascularization and minimally invasive valve surgery in patients with concomitant coronary and valvular heart disease. Innovations (Phila) 2017;12:4-8. [PubMed]
- Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention 2005;1:219-27. [PubMed]
- Shahian DM, O’Brien SM, Filardo G, et al. The Society of Thoracic Surgeons 2008 cardiac surgery risk models: part 3-valve plus coronary artery bypass grafting surgery. Ann Thorac Surg 2009;88:S43-62. [PubMed]
- Santana O, Reyna J, Pineda AM, et al. Outcomes of minimally invasive mitral valve surgery in patients with an ejection fraction of 35% or less. Innovations 2013;8:1-5. [PubMed]
- Mathew JP, Fontes ML, Tudor IC, et al. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA 2004;291:1720-29. [PubMed]
- Saxena A, Dinh DT, Smith JA, et al. Usefulness of postoperative atrial fibrillation as an independent predictor for worse early and late outcomes after isolated coronary artery bypass grafting (multicenter Australian study of 19,497 patients). Am J Cardiol 2012;109:219-25. [PubMed]
- Moscarelli M, Fattouch K, Casula R, et al. What is the role of minimally invasive mitral valve surgery in high-risk patients? A meta-analysis of observational studies. Ann Thorac Surg 2016;101:981-89. [PubMed]
- Mihos CG, Santana O, Lamas GA, et al. Incidence of postoperative atrial fibrillation in patients undergoing minimally invasive versus median sternotomy valve surgery. J Thorac Cardiovasc Surg 2013;146:1436-41. [PubMed]
- Ragnarsdóttir M. Short-term changes in pulmonary function and respiratory movements after cardiac surgery via median sternotomy. Scand Cardiovasc J 2004;38:46-52. [PubMed]
- Leacche M, Umakanthan R, Zhao DX, et al. Surgical update: hybrid procedures, do they have a role? Circ Cardiovasc Interv 2010;3:511-18. [PubMed]


