Percutaneous cavitary lavage in the diagnosis of pulmonary cavities
Introduction
A pulmonary cavity is defined radiologically as a lucency surrounded by a variously thickened wall within a pulmonary consolidation, mass or nodule. The term generally implies that the central portion of the lesion has undergone necrosis and been expelled via the bronchi, with a gas-containing space remaining (1).
It is important to differentiate a cavitary malignant tumor from a benign lesion. In some cases the general appearance gives some clues for the underlying etiology, particularly whether the lesion is benign or malignant. However, specimen, either aspirate or biopsy, should be taken for microbiologic and/or pathologic examination to reach a final diagnosis in most cases. Cutting needle biopsy or fine needle aspiration techniques may fail due to not only low possibility of targeting the thin wall of the cavity but also high possibility of aspiration of the solid reactive normal tissue around the cavity wall.
Millard and Wescott, in 1974, described a method in which percutaneous aspiration of a cavity was performed (2). They inserted a 20-gauge spinal needle into the cavity under fluoroscopic control. They injected sterile saline under fluoroscopic vision until the cavity appeared filled or almost filled with saline. The fluid was then alternately aspirated and injected once or twice gently and withdrawn. In all three patients they performed this procedure, the washings were diagnostic of carcinoma. They concluded that this technique was quick and relatively easy with minimal risk. We have carried out a similar method under computed tomography (CT) guidance since 1998 in patients with a pulmonary cavitary lesion who were not diagnosed by other methods. We collected data of these patients retrospectively and decided to evaluate the role of the technique in the differentiation of malignant and benign pulmonary cavities in this study.
Materials and methods
The medical records of our hospital and patient files were evaluated retrospectively from 1998 to January 2013. A total of 16 patients [13 men and 3 women; mean age, 60.6 years (range, 37-78 years)] with pulmonary cavities who met the selection criteria were included in the study. The selection criteria of pulmonary cavities for the study were as following: (I) Other methods such as sputum examination and the bronchoscopic technique failed to diagnose; (II) The cavity should not be suitable for cutting biopsy to obtain tissue sample; (III) The cavity should be located peripherally; (IV) The wall should not be thicker than 5 mm in any part of the cavity; (V) There should be a safe route to reach the cavity.
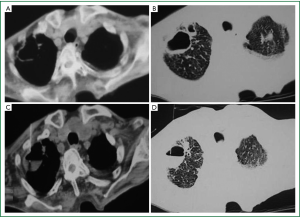
All patients have undergone a chest CT examination prior to the procedure. The cavity sizes have ranged from 2 to 4.5 cm in diameter. A procedure that was named as percutaneous cavitary lavage (PCL) by our group has been performed using an aseptic technique under chest CT guidance. Informed consent has been obtained from each patient. Position of the patients, level and direction of needle entry to provide the most direct and safe route and volume of the cavity have been determined according to previous CT examination of the patients and new scans have been obtained from the lesion depending on the previous ones. If any change in volume has occurred on the CT scans obtained during PCL, volume calculations have been revised. The volume of cavity has been calculated with the formulas 4/3×π×r3 for spherical cavities (r is the radius of the cavity) and as 4/3×π×abc for ellipsoid cavities (a, b and c are the dimensions of the cavity) on the CT scans. Using the previous CT scans as reference CT scans have been obtained to verify the exact entry point and tract of the needle. After injection of local anesthetic into the skin and subcutaneous tissue, a 22-gauge needle has been inserted into the cavity while patient was holding breath. After confirming the exact location of the tip of the needle within the cavity with CT scan, saline in quantity of two-thirds of the calculated volume (2.5-25 milliliters) has been injected through the needle using a handheld syringe and scans have been taken to see if the injected saline was enough and to calculate the distance between the needle tip and bottom of the cavity. After waiting for 3 to 5 minutes with the patient shallow breathing, the needle has been inserted as deep as the tip of the needle nearly reached the bottom of the cavity and the injected saline has been aspirated and the needle has been withdrawn while patient was holding breath (Figure 1). A part of the aspirate has been immediately prefixed with an equal volume of 50% ethanol for cytopathological examination. Specimens obtained during the procedure have been immediately transported to the laboratory for cytological and microbiological examinations. In 6 patients it has been possible to perform fine needle aspiration biopsy. To detect possible complications including pneumothorax and hemorrhage, CT images have been obtained at the end of the procedure, chest X-ray films have been taken 1 hour and 24 hours after the procedure. The patients living close to hospital have been informed about symptoms of pneumothorax and other possible complications and recommended to lie on the intervention site. They have been discharged and told to come for the chest X-ray at 24th hour. The inpatients have been followed at their clinics.
Cytopathology results were categorized in 4 groups (Table 1).

Full Table
The final diagnosis was made by either surgery, or FNAB if available, or clinical and radiological follow-up. All patients were followed for up to 6 months.
Descriptive analyses were processed with Windows based SPSS 10.0 software. McNemar and Kappa (measurement of agreement) tests were used in statistical analysis of the data. In addition, diagnostic values, sensitivity, specificity, positive and negative predictive values of the procedure for malignant-benign differentiation were calculated.
The Institutional Ethics Committee approved the study.
Results
Sixteen patients, with a pulmonary thin-walled cavitary lesion filled with air underwent CT guided PCL. The demographic features of patients, category of PCL, final diagnosis and method of final diagnosis are given in Table 2.
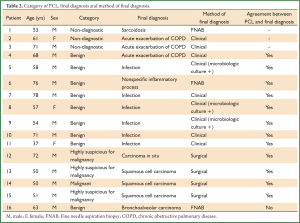
Full Table
The procedure correctly categorized cavitary lesions as either malignant or benign in 12 of 16 patients (75%). Four cavities that were categorized as either malignant or highly suspicious for malignancy according to PCL procedure had a final diagnosis of malignancy. Eight of the nine patients with a benign result in PCL had the same final diagnosis and the procedure missed malignancy in only 1 patient.
The patients were followed-up for 6 months. Four of the 5 malignant cavities according to final diagnosis underwent surgery and given adjuvant chemotherapy and one only received chemotherapy. Specific microorganisms had grown in 3 of 6 patients (50%) in cavities diagnosed as infectious (Two Mycobacterium tuberculosis and one Pseudomonas aeruginosa). No microorganism had grown in the other 3 patients. They had a diagnosis of pulmonary abscess clinically. Cavities in pulmonary abscess cases and due to Pseudomonas aeruginosa had resolved completely whereas cavities due to Mycobacterium tuberculosis had regressed. Among the three cavities whose PCL results were nondiagnostic, one was diagnosed finally as sarcoidosis by FNAB. The cavity had resolved completely at the 30th day of corticosteroid treatment. The other 2 nondiagnostic results were acute exacerbation of chronic obstructive pulmonary disease and the cavities had resolved after antibiotic treatment. However, there was no specific organism in culture of specimens taken from cavities. During the follow-up period all benign lesions showed improvement both clinically and radiologically with the given therapy.
We observed only one complication, a pneumothorax resolved without any intervention. We did not encounter any hemorrhage after PCL.
The average total time spent during the PCL procedure was 10-15 minutes.
There was no statistically significant difference between PCL and final diagnosis for malignant or benign diagnosis of cavitary lesions by McNemar test (P=1.0). The agreement between PCL and final diagnosis by Kappa test was found statistically significant (κ=0.831, P=0.002).
Excluding the 3 non-diagnostic specimens, the diagnostic sensitivity, specificity and accuracy of PCL for malignant-benign differentiation was 80%, 100% and 92.3%, respectively. The positive predictive value of PCL was 100% whereas its negative predictive value was 88.8%. There was only one complication (6%) due to PCL procedure.
Discussion
Etiologies of pulmonary cavitary lesions may be benign such as infections, vasculitidies, thrombooemboli, sarcoidosis, trauma or malignant either primer or metastatic. The most important expectation in diagnostic evaluation of a pulmonary cavitary lesion is to determine whether the lesion is benign or malignant since it will affect the management of the patient. The general appearance may give some clues for the differentiation of benign and malignant lesions (3). However, specimen, either aspirate or biopsy, should be taken for microbiologic and/or pathologic examination to reach a final diagnosis in most cases. The most widely accepted methods are CT-guided percutaneous fine needle aspiration biopsy and core biopsy. Although there are papers in literature reporting effectiveness of these CT-guided methods for pulmonary lesions, there is no data for cavitary lesions specifically (4-9). For peripheral malignant lesions, CT-guided cutting biopsy has a diagnostic accuracy rate of >92.7% and a sensitivity rate of >93% whereas CT-guided FNAB has a diagnostic accuracy rate of >77.2% and a sensitivity rate of >82%, depending on lesion size (4-9). CT-guided cutting needle biopsy also achieves better diagnostic accuracy than FNAB for benign lesions (92% vs. 40%) (10).
In a cavitary lesion, biopsy is obtained from the lesion wall; however, it is usually impossible to get specimens from the pulmonary cavities by either cutting biopsy or fine needle aspiration when they are thin walled. In addition, the solid reactive normal tissue around the cavity wall can be aspirated and this may cause a false normal result. For these reasons an alternative technique was described by Millard and Wescott and only 2 studies were reported with this technique in English literature (2,11,12).
Black et al. used a contrast technique to improve sampling in cavitating lung lesions in 12 patients (11). A 22 gauge Westcott needle was used and 3-4 mL of half strength contrast material was instilled. The contrast medium was used to lavage the cavity and then was aspirated for analysis. A diagnosis was made in 11 of the 12 patients (92%). The main diagnosis was infection (8 of 12 patients, 67%) followed by malignancy (3 of 12 patients, 25%) and methotrexate-induced interstitial lung disease (1 of 12 patients, 8%). One patient who had not been diagnosed following the procedure showed resolution of the cavity on follow up.
Nakahara et al. studied a percutaneous technique named as percutaneous needle washing in patients with pulmonary thin-walled cavitary lesions filled with air (12). Percutaneous needle washing was performed on 27 patients in whom diagnosis could not be reached by sputum and bronchoscopic examinations. The procedure was done under fluoroscopy guidance and after the 22-gauge needle was inserted, normal saline was injected into the cavity and aspirated. The procedure detected either malignant cells (in 10 patients) or the causative microorganism (in 9 patients) in 19 of 27 patients (70%). The diagnosis of 16 of the 17 patients who were negative for malignant cells on percutaneous needle washing was ascertained as benign disease during their clinical course. Final diagnosis could not be made in only one patient thus diagnostic accuracy was 96% (26/27). The diagnostic sensitivity of percutaneous needle washing for malignant diseases was 91% (10/11), while that for infections was 69% (9/13).
Our technique was similar to the technique of Nakahara et al., except that we performed PCL under CT guidance. This provided us a more reliable and rapid way to obtain specimens. We calculated the injected saline volume on previous CT scans. However, if any change in volume occurred on the CT scans obtained during PCL, we could revise our calculations. We confirmed the exact location of the tip of the needle. If possible we also performed fine needle aspiration in the same session. The mean time for the procedure was 10 to 15 minutes.
We could correctly categorize cavitary lesions either malignant or benign in 12 of 16 patients (75%) by PCL similar to the findings of Nakahara et al. (70%) and somewhat lower than Black et al. (98%). Excluding the 3 non-diagnostic specimens, the diagnostic sensitivity, specificity and accuracy of PCL for malignant-benign differentiation was 80%, 100% and 92.3%, respectively. The positive predictive value of PCL was 100% whereas its negative predictive value was 88.8%.
Safety is an important point of consideration in evaluation of a new diagnostic technique. Two mild pneumothoraces with 7% (2 of 27 patients) were found in study of Nakahara et al., and one single small pneumothorax with 8.3% (1 of 12 patients) was present in the study of Black et al. whereas there was only one pneumothorax (6.3%, 1 of 16 patients) in our study (11,12). Main complication of CT-guided FNAB and cutting needle biopsy was reported as pneumothorax with 17-28.4% (8,13-16). These figures are higher than that of PCL and washing.
The results of previous studies and our study suggest that PCL is an accurate method for obtaining suitable specimen from a cavitary lesion for laboratory examination including both microbiologic and cytologic examinations. The lavage of the cavity allows taking a greater sample volume for analysis. Morbidity rate is very low. PCL serves to provide adequate specimen in a short time, accurately and safely so that adequate differentiation of malign and benign etiologies can be done earlier, eliminating many laboratory investigations, diagnostic procedures and long hospital stay. It should be kept in mind that PCL will be useful only if positive, and it will not exclude any lung pathology when negative. Since the number of patients in our study and similar studies are small to be conclusive, further studies enrolling large number of patients are needed to clarify this subject.
In conclusion, we suggest that PCL can be used as an alternative method in malignant versus benign differentiation of thin walled pulmonary cavitary lesions safely in patients whose diagnosis could not be made by sputum and bronchoscopic procedures and who are not suitable for cutting biopsy.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Tuddenham WJ. Glossary of terms for thoracic radiology: recommendations of the Nomenclature Committee of the Fleischner Society. AJR Am J Roentgenol 1984;143:509-17. [PubMed]
- Millard JR, Westcott JL. Percutaneous needle washings in the diagnosis of cavitary lesions of the lung. Radiology 1974;111:474. [PubMed]
- Vourtsi A, Gouliamos A, Moulopoulos L, et al. CT appearance of solitary and multiple cystic and cavitary lung lesions. Eur Radiol 2001;11:612-22. [PubMed]
- Hiraki T, Mimura H, Gobara H, et al. CT fluoroscopy-guided biopsy of 1,000 pulmonary lesions performed with 20-gauge coaxial cutting needles: diagnostic yield and risk factors for diagnostic failure. Chest 2009;136:1612-7. [PubMed]
- Heyer CM, Reichelt S, Peters SA, et al. Computed tomography-navigated transthoracic core biopsy of pulmonary lesions: which factors affect diagnostic yield and complication rates? Acad Radiol 2008;15:1017-26. [PubMed]
- Yeow KM, Tsay PK, Cheung YC, et al. Factors affecting diagnostic accuracy of CT-guided coaxial cutting needle lung biopsy: retrospective analysis of 631 procedures. J Vasc Interv Radiol 2003;14:581-8. [PubMed]
- Wallace MJ, Krishnamurthy S, Broemeling LD, et al. CT-guided percutaneous fine-needle aspiration biopsy of small (< or =1-cm) pulmonary lesions. Radiology 2002;225:823-8. [PubMed]
- Ohno Y, Hatabu H, Takenaka D, et al. CT-guided transthoracic needle aspiration biopsy of small (< or = 20 mm) solitary pulmonary nodules. AJR Am J Roentgenol 2003;180:1665-9. [PubMed]
- Laspas F, Roussakis A, Efthimiadou R, et al. Percutaneous CT-guided fine-needle aspiration of pulmonary lesions: Results and complications in 409 patients. J Med Imaging Radiat Oncol 2008;52:458-62. [PubMed]
- Gong Y, Sneige N, Guo M, et al. Transthoracic fine-needle aspiration vs concurrent core needle biopsy in diagnosis of intrathoracic lesions: a retrospective comparison of diagnostic accuracy. Am J Clin Pathol 2006;125:438-44. [PubMed]
- Black JA, Blake MP, Cameron DC. A contrast technique to improve sampling in cavitating lung lesions. Australas Radiol 1996;40:6-9. [PubMed]
- Nakahara Y, Mochiduki Y, Miyamoto Y. Percutaneous needle washing for the diagnosis of pulmonary thin-walled cavitary lesions filled with air. Intern Med 2007;46:1089-94. [PubMed]
- Covey AM, Gandhi R, Brody LA, et al. Factors associated with pneumothorax and pneumothorax requiring treatment after percutaneous lung biopsy in 443 consecutive patients. J Vasc Interv Radiol 2004;15:479-83. [PubMed]
- Saji H, Nakamura H, Tsuchida T, et al. The incidence and the risk of pneumothorax and chest tube placement after percutaneous CT-guided lung biopsy: the angle of the needle trajectory is a novel predictor. Chest 2002;121:1521-6. [PubMed]
- Yeow KM, Su IH, Pan KT, et al. Risk factors of pneumothorax and bleeding: multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest 2004;126:748-54. [PubMed]
- Khan MF, Straub R, Moghaddam SR, et al. Variables affecting the risk of pneumothorax and intrapulmonal hemorrhage in CT-guided transthoracic biopsy. Eur Radiol 2008;18:1356-63. [PubMed]


