
早期肺癌患者行胸腔镜下亚肺叶切除术的适应证
引言
目前,手术依然是根治早期非小细胞肺癌(NSCLC)的最常用方法[1]。在肺癌研究小组(LCSG)进行的随机对照试验结果揭示后,肺叶切除术被视为是治疗早期NSCLC的金标准[2]。然而,为了提高切除率,我们需要为那些被认为具有高手术风险的人群如高龄、呼吸困难、多合并症的患者进行手术[3-5]。为了应对这些潜在手术风险及可能的生活质量和呼吸功能的长期损害,外科医生开始应用亚肺叶切除术来治疗肺癌。这种手术包括两种截然不同的术式:非解剖性切除(楔形切除)和解剖性切除(肺段切除)。二者的不同在于肺段切除术要求遵循肺叶切除术的肿瘤学原则,如解剖性分离肺段静脉、动脉、支气管以及较好的清除肺实质组织。
电视辅助胸腔镜手术(VATS)越来越广泛的运用于良、恶性病变的治疗。大量的研究不仅证实了VATS治疗早期肺癌的安全性和可行性,而且还说明了与开胸手术相比VATS在术后疼痛、恢复时间、恢复活动、术后免疫反应以及肿瘤疗效方面均具有优势[6-9]。正如开胸手术有一系列不同的手术入路(如后外侧入路、前入路、保留肌肉切口、杂交开胸手术等),VATS也有几种不同的手术方式:如后入路、前入路、两孔胸腔镜手术和单孔胸腔镜手术等[10-13]。
我们旨在探索亚肺叶切除术和VATS技术相结合治疗早期NSCLC的潜在可能性和最新经验。
非解剖性亚肺叶切除术(楔形切除术)
楔形切除术仅涉及边界清楚的肺部肿块,而不处理肺门处结构(肺动脉、肺静脉和支气管)。尽管LCSG的试验结果表明楔形切除比肺叶切除的复发率更高而被认为只是一种姑息性手术,但楔形切除的适应证却在逐渐放宽[2]。有一点是肯定的,即只有可清楚辨认的周围型病变才可以被安全的“楔形切除”,并保证足够的切缘。虽然将其作为肿瘤治疗的一种方法有其理论上的局限性,但楔形切除术依然被应用于治疗特定情况的肺癌患者[14,15]。
手术技术
VATS楔形切除术可通过单孔或多孔来完成[16]。最理想的状况是单肺通气情况下,患侧肺组织塌陷,这样便于肿物定位与器械操作,然而对于不能耐受单肺通气的患者在其患侧肺充气情况下也可尝试进行。有多种方法可以确定结节部位,包括利用器械或指尖触诊以及其他如金属丝/线圈定位技术[17,18]、各种造影剂灌注技术[19-21]、术中超声技术[22]等较为复杂的技术手段。
一旦确定了结节部位,就可以应用外科吻合器将其连带周围肺组织一并切除。视频1即是单孔途径诊断性切除左下叶结节的简介,图1示器械及切口的位置。
结果
应用楔形切除术治疗肺癌只有非常有限的证据。由LCSG开展的一项随机对照试验结果显示:与肺叶切除术相比,楔形切除术有相似的生存率,但复发率明显增高[2]。外科协会认可试验者的工作并接受了这一试验结果,甚至接受了该试验的局限性,将肺叶切除术作为早期肺癌治疗的首选,由于亚肺叶切除术对特定患者人群有保留更多肺组织和手术过程更快捷的潜在优势,故而将其作为该人群的保留术式。
VATS楔形切除术的相关试验结果与传统的开胸肺叶切除术结果一致。Wolf等回顾性对比研究了154例亚肺叶切除术(43%应用VATS)和84例肺叶切除术(10%应用VATS)治疗早期小细胞肺癌患者的术后效果。结果表明肺叶切除组的患者有更好的生存率和无病生存率,但本试验及其他同类试验选择性偏倚均比较显著,例如亚肺叶切除组的患者年龄更大且呼吸功能储备更差[23]。Landreneau等通过多中心研究对比了102例楔形切除术(60%应用VATS)与肺叶切除术的术后效果,也得到了相似的结论[24]。
应用VATS的潜在局限性之一是难以在术中确定深部小结节的位置。应用某些技术可以协助小结节的定位。Lee等运用线圈定位技术成功地为103例肺部小结节患者中的101例进行了定位,历时平均11分钟[16]。Molins等先在门诊运用线圈定位技术为52例患者中的50例进行了定位,然后完成了VATS小结节切除[18]。运用各种不同标记(包括亚甲基蓝、放射性同位素或造影剂)进行定位的成功率相似[19-21]。此外,VATS术中可应用超声定位技术,甚至单孔胸腔镜手术中也可应用[25]。总之,不管应用哪种技术,都对VATS术中深部或小结节的定位提供了很大帮助。
适应证
根据现有的有限证据和楔形切除术治疗特定肺癌人群的相关报道,我们认为楔形切除术治疗早期NSCLC的适应证可能有以下几种:
1.必须保留更多肺组织的患者。其中包括呼吸功能储备有限的COPD患者、肺叶切除术后预后较差的严重肺纤维化患者、肺动脉高压患者以及新近发现的异时性或同时性多发性肺癌患者。
2.术前不能获取或未能证实病理类型的患者。不仅包括不能经皮穿刺活检的肺部小结节患者,而且还包括曾有其他部位恶性肿瘤病史,无法确定转移灶还是原发灶的患者,以及影像学检查并不十分倾向肺癌诊断但患者要求组织学证实者。
3.肺结节诊断困难的患者。肺部结节性疾病(如肺结核、肉瘤、风湿病等),其中一个或多个结节可疑恶性肿瘤,但由于其慢性疾病过程的掩盖有可能造成早期NSCLC的漏诊。
4.具有严重并发症或高龄仅能耐受短时间全麻的周围型肺癌患者,如果楔形切除术能在几分钟内完成,甚至能在患侧肺通气的情况下进行时,则适合行楔形切除术。
解剖性亚肺叶切除术(肺段切除术)
肺段切除术包括一个或多个肺段的解剖性切除。要求分离与所要切除肺段的动脉、静脉和支气管的段分支。在很多情况下,传统的用手或电刀寻找段间肺组织平面的技术手段已被外科吻合器所替代,外科吻合器,吻合器分离段间平面具有减少漏气和肺组织出血的优点[26-28]。
应用肺段切除术治疗早期肺癌已有文献报道,且似乎应用愈发广泛[29,30]。外科医生们认为,在某些情况下用肺段切除术替代肺叶切除术,有可能增加可手术性(如对于高龄患者、呼吸功能储备较差的患者、有肺部切除手术史患者)和提高手术切除率(如对于多灶性磨玻璃样结节患者、同时性多发肿瘤患者、有其他可能发生转移的实性恶性肿瘤病史患者),而且,对于非常小的早期NSCLC也是首选治疗方式[31,32]。
目前,VATS肺段切除术的经验虽然有限,但却在不断积累中,该技术得到了经验丰富的胸腔镜手术医生的支持,而且逐渐被更多的医疗中心采纳[33,34]。这种手术可以通过各种方式的VATS途径包括单孔途径来完成(视频2),图2显示器械的位置。
手术技术
肺段切除术可以分为典型(肺组织分离涉及 2级支气管水平)和非典型(更复杂且技术要求更高,肺段切除涉及3级支气管水平)两类。前者包括双肺的第6肺段(背段)切除、舌段切除、左肺上叶固有段切除、左肺基底段切除、右肺第7~10肺段切除等。后者少见,包括右肺7~8肺段切除和双肺第9~10肺段切除等。
患者侧卧,胸部过伸以增大肋间隙,背阔肌前缘前方第4或5肋间隙4cm切口。用30度胸腔镜探查胸腔。尽量使胸腔镜靠近切口后缘,以利于2件、3件甚至更多的腔镜器械进入胸腔而不相互干扰。先用电刀分离胸腔粘连,然后行左肺上叶固有段切除术。确认肺动脉后,分离固有段肺动脉分支并用腔镜吻合器切断。然后分离并切断固有段肺静脉分支,注意保留舌段肺静脉分支以保证舌段血液回流。稍微有些难度的是固有段支气管的确认。由于曾有VATS术中误断段支气管的报道,所以我们建议游离出固有段支气管后,应在切断前先行肺膨胀测试。切断段支气管后,用肺膨胀方法确认肺组织平面,然后切除。标本装入标本袋利于取出并且理论上可以减少伤口种植转移风险。游离下肺韧带,清扫淋巴结,肺组织复张满意后放置一根肋间引流管。有些外科医生用其他方法确认段间平面:如使用吲哚菁绿滴剂或者隔离所要切除肺段,使非切除肺段膨胀等方法,这些方法都是有效的。
结果
唯一一项涉及解剖性肺段切除术治疗肺癌的随机对照试验是由LCSG开展的,可惜的是,肺段切除与楔形切除被分在同一组。这项研究的结论是亚肺叶切除术的生存率与肺叶切除术生存率相同,但复发率较高,这就为将肺叶切除术作为治疗早期肺癌的首选方式提供了有力证据。很遗憾,按照该研究的试验设计,其结论不可能用来推断肺段切除术的真实治疗效果[2]。
随后,少数病例对照研究和几项对比试验表明,无论是高危人群还是总体人群,解剖性肺段切除术在治疗小肺癌方面与肺叶切除术有同等价值[35-37]。尽管生存率和复发率相似,但有证据表明肺段切除术对于肺功能的影响较小。
大量外科实例表明VATS肺叶切除术比开胸手术有更多潜在优势(如疼痛较轻、恢复较早、并发症较少、免疫反应较弱等),这使得VATS解剖性肺段切除术的发展前景令人期待[6-9]。几位学者介绍了他们运用从四孔到单孔的一系列VATS手术方法的经验,还有些研究进行了VATS肺段切除术和开胸肺段切除术治疗肺癌的比较[38]。
总体来说,学者们认为VATS肺段切除术和VATS肺叶切除术在围术期疗效、生存率及复发率等方面没有显著差异(表1)[39-43]。不同报道中VATS肺段切除术的局部复发率在2.8%~7.7%之间,这与由相同外科医生完成的VATS肺叶切除术的局部复发率相似。Atkin等的一篇文章中比较了一家胸腔镜手术经验丰富的医疗中心的开胸及VATS肺段切除术的疗效,其围术期效果表明VATS技术并不逊色[38]。
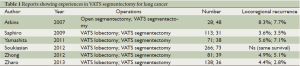
Full table
然而,学者们也没有发现VATS肺段切除术比VATS肺叶切除术明显缩短患者的住院时间,这可能是由肺段切除术比无裂缝VATS肺叶切除术对肺组织的创伤更广泛,其术后持续性肺漏气所导致的[39-43]。开胸手术中肺段切除术后肺功能优于肺叶切除术,在VATS的研究中同样得以证实[44]。
适应证
根据现有的有限证据以及正在进行的研究(肺段切除术对比肺叶切除术治疗早期肺癌的CALBG-140503临床试验)的可能结果,VATS亚肺叶切除术治疗NSCLC的可能的适应证包括:
1. 有实性恶性肿瘤病史并且术中冰冻切片不能证实其结节是原发性肺癌还是来自远处转移的患者;
2. 多灶性磨玻璃样结节,之前称作细支气管肺泡癌;
3. 既往有肺切除术病史的第二原发癌患者;
4. 施行肺叶切除术风险较高的患者,包括合并呼吸系统疾病、高龄或幼儿患者等;
5. 越来越多的直径小于2cm的周围型早期肺癌患者选择肺段切除术进行治疗。
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Lim E, Baldwin D, Beckles M, et al. Guidelines on the radical management of patients with lung cancer. Thorax 2010;65:iii1-27. [PubMed]
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung Cancer Study Group. Ann Thorac Surg 1995;60:615-22; discussion 622-3. [PubMed]
- Martin-Ucar AE, Waller DA, Atkins JL, et al. The beneficial effects of specialist thoracic surgery on the resection rate for non-small-cell lung cancer. Lung Cancer 2004;46:227-32. [PubMed]
- Riaz SP, Linklater KM, Page R, et al. Recent trends in resection rates among non-small cell lung cancer patients in England. Thorax 2012;67:811-4. [PubMed]
- Griffin JP, Eastridge CE, Tolley EA, et al. Wedge resection for non-small cell lung cancer in patients with pulmonary insufficiency: prospective ten-year survival. J Thorac Oncol 2006;1:960-4. [PubMed]
- Yan TD, Black D, Bannon PG, et al. Systematic review and meta-analysis of randomized and nonrandomized trials on safety and efficacy of video-assisted thoracic surgery lobectomy for early-stage non-small-cell lung cancer. J Clin Oncol 2009;27:2553-62. [PubMed]
- Paul S, Altorki NK, Sheng S, et al. Thoracoscopic lobectomy is associated with lower morbidity than open lobectomy: a propensity-matched analysis from the STS database. J Thorac Cardiovasc Surg 2010;139:366-78. [PubMed]
- Petersen RP, Pham D, Burfeind WR, et al. Thoracoscopic lobectomy facilitates the delivery of chemotherapy after resection for lung cancer. Ann Thorac Surg 2007;83:1245-9; discussion 1250. [PubMed]
- Yim AP, Wan S, Lee TW, et al. VATS lobectomy reduces cytokine responses compared with conventional surgery. Ann Thorac Surg 2000;70:243-7. [PubMed]
- Walker WS, Carnochan FM, Pugh GC. Thoracoscopic pulmonary lobectomy. Early operative experience and preliminary clinical results. J Thorac Cardiovasc Surg 1993;106:1111-7. [PubMed]
- Hansen HJ, Petersen RH, Christensen M. Video-assisted thoracoscopic surgery (VATS) lobectomy using a standardized anterior approach. Surg Endosc 2011;25:1263-9. [PubMed]
- Onaitis MW, Petersen RP, Balderson SS, et al. Thoracoscopic lobectomy is a safe and versatile procedure: experience with 500 consecutive patients. Ann Surg 2006;244:420-5. [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [PubMed]
- Falcoz PE, Conti M, Brouchet L, et al. The Thoracic Surgery Scoring System (Thoracoscore): risk model for in-hospital death in 15,183 patients requiring thoracic surgery. J Thorac Cardiovasc Surg 2007;133:325-32. [PubMed]
- Kozower BD, Sheng S, O’Brien SM, et al. STS database risk models: predictors of mortality and major morbidity for lung cancer resection. Ann Thorac Surg 2010;90:875-81; discussion 881-3. [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [PubMed]
- Li W, Wang Y, He X, et al. Combination of CT-guided hookwire localization and video-assisted thoracoscopic surgery for pulmonary nodular lesions: analysis of 103 patients. Oncol Lett 2012;4:824-8. [PubMed]
- Molins L, Mauri E, Sánchez M, et al. Locating pulmonary nodules with a computed axial tomography-guided harpoon prior to videothoracoscopic resection. Experience with 52 cases. Cir Esp 2013;91:184-8. [PubMed]
- Vandoni RE, Cuttat JF, Wicky S, et al. CT-guided methylene-blue labeling before thoracoscopic resection of pulmonary nodules. Eur J Cardiothorac Surg 1998;14:265-70. [PubMed]
- Choi BG, Kim HH, Kim BS, et al. Pulmonary nodules: CT-guided contrast material localization for thoracoscopic resection. Radiology 1998;208:399-401. [PubMed]
- Stiles BM, Altes TA, Jones DR, et al. Clinical experience with radiotracer-guided thoracoscopic biopsy of small, indeterminate lung nodules. Ann Thorac Surg 2006;82:1191-6; discussion 1196-7. [PubMed]
- Piolanti M, Coppola F, Papa S, et al. Ultrasonographic localization of occult pulmonary nodules during video-assisted thoracic surgery. Eur Radiol 2003;13:2358-64. [PubMed]
- Wolf AS, Richards WG, Jaklitsch MT, et al. Lobectomy versus sublobar resection for small (2 cm or less) non-small cell lung cancers. Ann Thorac Surg 2011;92:1819-23; discussion 1824-5.
- Landreneau RJ, Sugarbaker DJ, Mack MJ, et al. Wedge resection versus lobectomy for stage I (T1 N0 M0) non-small-cell lung cancer. J Thorac Cardiovasc Surg 1997;113:691-8; discussion 698-700. [PubMed]
- Rocco G, Cicalese M, La Manna C, et al. Ultrasonographic identification of peripheral pulmonary nodules through uniportal video-assisted thoracic surgery. Ann Thorac Surg 2011;92:1099-101. [PubMed]
- Jones DR, Stiles BM, Denlinger CE, et al. Pulmonary segmentectomy: results and complications. Ann Thorac Surg 2003;76:343-8; discussion 348-9. [PubMed]
- Okada M, Mimura T, Ikegaki J, et al. A novel video-assisted anatomic segmentectomy technique: selective segmental inflation via bronchofiberoptic jet followed by cautery cutting. J Thorac Cardiovasc Surg 2007;133:753-8. [PubMed]
- D’Amico TA. Thoracoscopic segmentectomy: technical considerations and outcomes. Ann Thorac Surg 2008;85:S716-8. [PubMed]
- Jensik RJ, Faber LP, Milloy FJ, et al. Segmental resection for lung cancer. A fifteen-year experience. J Thorac Cardiovasc Surg 1973;66:563-72. [PubMed]
- Yang CF, D’Amico TA. Thoracoscopic segmentectomy for lung cancer. Ann Thorac Surg 2012;94:668-81. [PubMed]
- Lau KK, Martin-Ucar AE, Nakas A, et al. Lung cancer surgery in the breathless patient--the benefits of avoiding the gold standard. Eur J Cardiothorac Surg 2010;38:6-13. [PubMed]
- Schuchert MJ, Pettiford BL, Pennathur A, et al. Anatomic segmentectomy for stage I non-small-cell lung cancer: comparison of video-assisted thoracic surgery versus open approach. J Thorac Cardiovasc Surg 2009;138:1318-25.e1.
- Shiraishi T, Shirakusa T, Iwasaki A, et al. Video-assisted thoracoscopic surgery (VATS) segmentectomy for small peripheral lung cancer tumors: intermediate results. Surg Endosc 2004;18:1657-62. [PubMed]
- Gonzalez-Rivas D, Fieira E, Mendez L, et al. Single-port video-assisted thoracoscopic anatomic segmentectomy and right upper lobectomy. Eur J Cardiothorac Surg 2012;42:e169-71. [PubMed]
- Martin-Ucar AE, Nakas A, Pilling JE, et al. A case-matched study of anatomical segmentectomy versus lobectomy for stage I lung cancer in high-risk patients. Eur J Cardiothorac Surg 2005;27:675-9. [PubMed]
- Date H, Andou A, Shimizu N. The value of limited resection for “clinical” stage I peripheral non-small cell lung cancer in poor-risk patients: comparison of limited resection and lobectomy by a computer-assisted matched study. Tumori 1994;80:422-6. [PubMed]
- Okada M, Yoshikawa K, Hatta T, et al. Is segmentectomy with lymph node assessment an alternative to lobectomy for non-small cell lung cancer of 2 cm or smaller? Ann Thorac Surg 2001;71:956-60; discussion 961. [PubMed]
- Atkins BZ, Harpole DH Jr, Mangum JH, et al. Pulmonary segmentectomy by thoracotomy or thoracoscopy: reduced hospital length of stay with a minimally-invasive approach. Ann Thorac Surg 2007;84:1107-12; discussion 1112-3. [PubMed]
- Shapiro M, Weiser TS, Wisnivesky JP, et al. Thoracoscopic segmentectomy compares favorably with thoracoscopic lobectomy for patients with small stage I lung cancer. J Thorac Cardiovasc Surg 2009;137:1388-93. [PubMed]
- Yamashita S, Chujo M, Kawano Y, et al. Clinical impact of segmentectomy compared with lobectomy under complete video-assisted thoracic surgery in the treatment of stage I non-small cell lung cancer. J Surg Res 2011;166:46-51. [PubMed]
- Soukiasian HJ, Hong E, McKenna RJ Jr. Video-assisted thoracoscopic trisegmentectomy and left upper lobectomy provide equivalent survivals for stage IA and IB lung cancer. J Thorac Cardiovasc Surg 2012;144:S23-6. [PubMed]
- Zhong C, Fang W, Mao T, et al. Comparison of thoracoscopic segmentectomy and thoracoscopic lobectomy for small-sized stage IA lung cancer. Ann Thorac Surg 2012;94:362-7. [PubMed]
- Zhao X, Qian L, Luo Q, et al. Segmentectomy as a safe and equally effective surgical option under complete video-assisted thoracic surgery for patients of stage I non-small cell lung cancer. J Cardiothorac Surg 2013;8:116. [PubMed]
- Keenan RJ, Landreneau RJ, Maley RH Jr, et al. Segmental resection spares pulmonary function in patients with stage I lung cancer. Ann Thorac Surg 2004;78:228-33; discussion 228-33. [PubMed]
(译者:王道威;校对:阎石)
(本译文仅供学术交流,实际内容请以英文原文为准。)




