Selective lymph node dissection in early-stage non-small cell lung cancer
Introduction
Morbidity and mortality of lung cancer are the highest among all neoplastic diseases in China (1) and worldwide (2). Among all the lung cancer- therapeutic methods, surgery plays a pivotal role, especially in the early-stage non-small cell lung cancer (NSCLC). Nowadays, the standard surgical treatment of early-stage NSCLC is lobectomy with systematic lymph node dissection (LND) as recommended by the guidelines (3,4), which capable of providing accurate staging (5,6), detecting occult metastasis (7) and improving survival (5,8,9). However, randomized trials have not demonstrated that LND has more survival benefit than sampling (7,10). Since advanced radiographic techniques become available and regular medical examination grows popular, early-stage NSCLC patients have occupied a larger proportion. Accordingly, minimally invasive approaches may be more favorable for those patients. In general, there are three approaches: video-assisted thoracic surgery, parenchyma-preserving resection and selective lymph node dissection (SLND) (11). The research and practice of the first two are comprehensive and deeply (12-14) while SLND remains controversial. Based on the metastatic rules derived from lobe-specific lymphatic drainage pattern (15,16), histologic component, a tumor marker and so on, SLND may be valid and applicable for selected patients to minimize surgical trauma so that patients can benefit from shorter operation time, less blood loss and shorter length of hospital stay (17,18). Still, some questioned remain unsolved.
Lobe-specific lymphatic drainage pattern
The mediastinal lymph node map is based on the International Association for the Study of Lung Cancer (IASLC) node map in the Seventh Edition of the TNM Classification (19).
Upper lobes
Lymphatic drainage pattern has been found in the upper lobe. Okada (20) investigated the lymphatic drainage pattern in 406 upper lobe NSCLC patients (64.3% pN0, 16.5% pN1 and 19.2% pN2) and showed that none of them had subcarinal node (SCN) metastasis. Similarly, Aokage and colleagues (21) reviewed 1,099 consecutive upper lobe NSCLC patients (72.6% pN1, 12.7% pN2 and 14.7% pN3) and revealed that upper lobe NSCLC rarely metastasized to subcarinal node (1.8%, 20/1,099), especially among squamous cell patients (0.5%, 1/182). In addition, for patients with upper lobe NSCLC without superior mediastinal lymph nodes (SMN) involved, even rare skip SCN metastasis (0.2%, 2/941) was found and no patients with squamous cancer had SCN metastasis (21). Notably, SCN metastasis contributes to cancer staging, highly correlated with poor survival and recurrence, while SCN dissection did not improve the outcome of upper lobe NSCLC patients (17,21-23). In conclusion, it is valid to exclude SCN dissection for early-stage upper lobe NSCLC patients, especially for clinical-N0 patients with squamous cell (21).
Other findings have confirmed such rules in the right upper lobe (RUL). Shimada (15) showed that most SCN metastasis in pathological N2 RUL NSCLC patients was accompanied by simultaneous SMN or hilar lymph node involvement (92%, 11/12) and skip metastasis merely occurred (8%, 1/12). Based on this study, it might be unnecessary for upper lobe NSCLC patients without SMN or hilar metastasis on frozen sections to undergo SCN dissection.
As for the left upper lobe, the most common sites of lymph node metastasis were the SMN and aortic nodes. No skip metastasis, i.e., SCN metastasis without SMN or AN involvement, occurred in 41 pathological-N2 NSCLC patients (15). This study indicates that SCN can be spared during surgery when SMN and aortic nodes are tumor-free.
Lower lobes
Lower lobe has its unique lymphatic drainage pattern. A retrospective analysis indicated that SMN skip metastasis without hilar lymph node or SCN involved only occurred in 8% (3/40) pathological-N2 right lower lobe NSCLC patients (15). Similar results have been reported by Okada (20), only 2 of 47 pathological-N2 patients had skip metastasis to SMN without SCN involvement. Both SCN (24) and SMN metastasis (25) in the lower lobe indicated poor prognosis. Based on such findings, SMN dissection may be unnecessary for right lower lobe NSCLC patients when hilar lymph node and SCN are both intraoperatively intact (17,20,26).
Regional mediastinal lymph nodes
Yoshimasu and colleagues (27) chose three mediastinal lymph nodes (MLN) for each lobe (Table 1) as regional mediastinal lymph nodes (RMLN), which are similar to sentinel lymph nodes of breast cancer. They propose that if the RMLN are tumor-free, the rest MLN should be preserved. After investigation of 58 patients, they suggested that limited MLN dissection is applicable to NSCLC patients whose RMLN are intact. Likewise, another Japanese team have defined regional lymph node stations: #2, #3, #4 and #10 for RUL, #7, #8 and #11 for RLL, #4, #5 and #6 for LUD, #5, #7 and #11 for LLD and #7, #8 and #11 for LLL (28). They believed that the intraoperative pathological examination on regional lymph node stations might lead to an appropriate choice between LND and SLND. Kawano (29) also selected several MLN for each lobe (Table 1) as target nodes. If metastasis found in these target nodes, LND was recommended. Shien and colleagues (30) assigned three stations (#5, #11, #12) as the regional lymph node stations for left lingular division (LLD). Based on their findings, the existence of pathological-N2 metastasis can be accurately predicted by intraoperative pathological examination and SLND or LND would be properly adopted in LLD-NSCLC patients with clinical-T2N1M0 or earlier stage (30). It is worth mentioning that only a few teams investigate in this area, and the reliability of RMLN should be further confirmed.

Full table
Predominant histological component
Despite the fact that upper lobe squamous cell patients rarely having SCN metastasis as mentioned above, adenocarcinoma patients showed dramatic difference. Above all, patients with adenocarcinoma were more likely to have N1 and N2 diseases compared with squamous cell patients (16). In regard of predominant histologic component of adenocarcinoma, lepidic predominant component was associated with node-negative while micropapillary and solid predominant components were correlated with node-positive (31). Hence, the specific relationship between predominant histological component and lymph node metastasis needs to be comprehensively revealed.
Tumor marker
Interestingly, Hattori (32) revealed that carcinoembryonic antigen (CEA) level was a significant predictor of lymph node metastasis. In addition, Haruki (26) elucidated that CEA elevation was highly associated with SMN metastasis in lower lobe clinical-stage I adenocarcinoma. Based on these studies, it is reasonable to preserve SMN for lower lobe clinical-stage I NSCLC patients with a normal level of CEA (26). However, we need more evidence to confirm the significance of CEA and elucidate the role of other tumor markers.
Strategies of lymph node dissection
Systematic lymph node dissection
When LND is operated in the right lobes, mediastinal lymph node stations #2R, #4R, #7, #8 and #9 should be dissected, while for the left lobes, mediastinal lymph node stations #4L, #5, #6, #7, #8 and #9 dissection is required. On both sides, N1 nodes are dissected as part of lung resection.
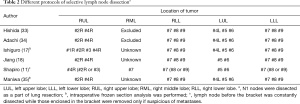
Protocols of SLND
Several retrospective studies have been carried out to determine whether SLND is an applicable option as a standard procedure and can provide clinical benefits. However, different groups selected various protocols of lobe-specific SLND. Hishida (33) chose the protocol as follows. For RUL, SMN (stations #2R and #4R) were dissected, while SMN and aortic nodes (stations #4L, #5 and #6) were dissected for left upper lobe. Inferior mediastinal nodes (station #7, #8 and #9) were preserved for both upper sides. For lower lobe on both sides, inferior mediastinal nodes (stations #7, #8 and #9) were dissected, while SMN and/or aortic nodes kept preserved. Adachi (34) shared the same protocol (Table 2). Intraoperative frozen section analysis was introduced in Futoshi Ishiguro’s protocol (17), where SMN for RUL, SMN and aortic nodes for LUL and inferior mediastinal nodes for lower lobe were removed. Intraoperative frozen section analyses were performed when dissected lymph node metastasis was suspected, and if positive, such patients would undergo LND. Protocols from other teams are similar to those above (Table 2).
Full table
Discussion
Some retrospective studies have demonstrated SLND is an alternative to LND for selected clinical-stage I–II patients and has the potential to become a standard procedure in surgical treatment for NSCLC (11,33,34,36,37). Meanwhile, Izbicki (10) and Graham (38) argued that LND should be routinely operated for resectable NSCLC. On one hand, whether LND would increase postoperative morbidity associated with complications is not clear (10,36) and the influence on outcome such as overall survival and disease-free survival remains controversial (5,8,17,33,34). On the other hand, the reported benefit that SLND can shorten the entire medical period along with its validity, reliability and applicability are still not very clear. Moreover, SLND was reported increasing the possibility of recurrence (35). In order to provide unambiguous answer, multi-institutional randomized clinical trials are expected to carry out in the future.
Although some doubt exists (39), lobe-specific lymphatic drainage pattern becomes increasingly credible and practical with more literature published (11,15,16,33,34). Still, several important questions remain to be answered. The complicated impacts of tumor location, size, mutation, differentiation and significant tumor markers have on lymph node metastasis are not well understood. As we all know, pathological classification is closely related to oncological characteristics and behaviors. It is really crucial to clarify the association between pathological classification and SLND. Importantly, only with a comprehensive understanding of lymphatic drainage pattern can we design an optimal protocol for SLND, which is the key to a well-designed clinical trial. Meanwhile, the positron emission computed tomography-computed tomography (PET-CT) and intraoperative frozen section analysis (12) should be considered for accurate clinical stage and precise intraoperative diagnosis.
A minimally invasive approach is the trend of surgical treatment for early-stage NSCLC and SLND is a vital component of it. Also, it is another solid step towards precision medicine.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin 2016;66:115-32. [Crossref] [PubMed]
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Howington JA, Blum MG, Chang AC, et al. Treatment of stage I and II non-small cell lung cancer: Diagnosis and management of lung cancer, 3rd ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest 2013;143:e278S-313S.
- De Leyn P, Lardinois D, Van Schil P, et al. European trends in preoperative and intraoperative nodal staging: ESTS guidelines. J Thorac Oncol 2007;2:357-61. [Crossref] [PubMed]
- Gajra A. Effect of Number of Lymph Nodes Sampled on Outcome in Patients With Stage I Non-Small-Cell Lung Cancer. J Clin Oncol 2003;21:1029-34. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS, Minnich DJ. Complete Thoracic Mediastinal Lymphadenectomy Leads to a Higher Rate of Pathologically Proven N2 Disease in Patients With Non-Small Cell Lung Cancer. Ann Thorac Surg 2012;94:902-6. [Crossref] [PubMed]
- Darling GE, Allen MS, Decker PA, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non–small cell carcinoma: Results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg 2011;141:662-70. [Crossref] [PubMed]
- Doddoli C, Aragon A, Barlesi F, et al. Does the extent of lymph node dissection influence outcome in patients with stage I non-small-cell lung cancer? Eur J Cardiothorac Surg 2005;27:680-5. [Crossref] [PubMed]
- Lardinois D, Suter H, Hakki H, et al. Morbidity, Survival, and Site of Recurrence After Mediastinal Lymph-Node Dissection Versus Systematic Sampling After Complete Resection for Non-Small Cell Lung Cancer. Ann Thorac Surg 2005;80:268-74; discussion 274-5. [Crossref] [PubMed]
- Izbicki JR, Passlick B, Pantel K, et al. Effectiveness of radical systematic mediastinal lymphadenectomy in patients with resectable non-small cell lung cancer: results of a prospective randomized trial. Ann Surg 1998;227:138-44. [Crossref] [PubMed]
- Shapiro M, Kadakia S, Lim J, et al. Lobe-specific mediastinal nodal dissection is sufficient during lobectomy by video-assisted thoracic surgery or thoracotomy for early-stage lung cancer. Chest 2013;144:1615-21. [Crossref] [PubMed]
- Liu S, Wang R, Zhang Y, et al. Precise Diagnosis of Intraoperative Frozen Section Is an Effective Method to Guide Resection Strategy for Peripheral Small-Sized Lung Adenocarcinoma. J Clin Oncol 2016;34:307-13. [Crossref] [PubMed]
- Zhang Y, Sun Y, Wang R, et al. Meta-analysis of lobectomy, segmentectomy, and wedge resection for stage I non-small cell lung cancer. J Surg Oncol 2015;111:334-40. [Crossref] [PubMed]
- Zhang Y, Yuan C, Zhang Y, et al. Survival following segmentectomy or lobectomy in elderly patients with early-stage lung cancer. Oncotarget 2016;7:19081-6. [Crossref] [PubMed]
- Shimada Y, Saji H, Kakihana M, et al. Retrospective Analysis of Nodal Spread Patterns According to Tumor Location in Pathological N2 Non-small Cell Lung Cancer. World J Surg 2012;36:2865-71. [Crossref] [PubMed]
- Cerfolio RJ, Bryant AS. Distribution and Likelihood of Lymph Node Metastasis Based on the Lobar Location of Nonsmall-Cell Lung Cancer. Ann Thorac Surg 2006;81:1969-73. [Crossref] [PubMed]
- Ishiguro F, Matsuo K, Fukui T, et al. Effect of selective lymph node dissection based on patterns of lobe-specific lymph node metastases on patient outcome in patients with resectable non–small cell lung cancer: A large-scale retrospective cohort study applying a propensity score. J Thorac Cardiovasc Surg 2010;139:1001-6. [Crossref] [PubMed]
- Jiang W, Chen X, Xi J, et al. Selective Mediastinal Lymphadenectomy Without Intraoperative Frozen Section Examinations for Clinical Stage I Non-Small-Cell Lung Cancer: Retrospective Study of 403 Cases. World J Surg 2013;37:392-7. [Crossref] [PubMed]
- Rusch VW, Asamura H, Watanabe H, et al. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009;4:568-77.
- Okada M, Tsubota N, Yoshimura M, et al. Proposal for reasonable mediastinal lymphadenectomy in bronchogenic carcinomas: role of subcarinal nodes in selective dissection. J Thorac Cardiovasc Surg 1998;116:949-53. [Crossref] [PubMed]
- Aokage K, Yoshida J, Ishii G, et al. Subcarinal lymph node in upper lobe non-small cell lung cancer patients: Is selective lymph node dissection valid? Lung Cancer 2010;70:163-7. [Crossref] [PubMed]
- Sun Y, Gao W, Zheng H, et al. Mediastinal Lymph-nodes Metastasis beyond the Lobe-specific: An Independent Risk Factor toward Worse Prognoses. Ann Thorac Cardiovasc Surg 2014;20:284-91. [Crossref] [PubMed]
- Casali C, Stefani A, Natali P, et al. Prognostic factors in surgically resected N2 non-small cell lung cancer: the importance of patterns of mediastinal lymph nodes metastases. Eur J Cardiothorac Surg 2005;28:33-8. [Crossref] [PubMed]
- Turna A, Solak O, Kilicgun A, et al. Is Lobe-Specific Lymph Node Dissection Appropriate in Lung Cancer Patients Undergoing Routine Mediastinoscopy? Thorac Cardiovasc Surg 2007;55:112-9. [Crossref] [PubMed]
- Asamura H, Nakayama H, Kondo H, et al. Lobe-specific extent of systematic lymph node dissection for non–small cell lung carcinomas according to a retrospective study of metastasis and prognosis. J Thorac Cardiovasc Surg 1999;117:1102-11. [Crossref] [PubMed]
- Haruki T, Aokage K, Miyoshi T, et al. Mediastinal Nodal Involvement in Patients with Clinical Stage I Non–Small-Cell Lung Cancer: Possibility of Rational Lymph Node Dissection. J Thorac Oncol 2015;10:930-6. [Crossref] [PubMed]
- Yoshimasu T, Miyoshi S, Oura S, et al. Limited mediastinal lymph node dissection for non-small cell lung cancer according to intraoperative histologic examinations. J Thorac Cardiovasc Surg 2005;130:433-7. [Crossref] [PubMed]
- Miyoshi S, Shien K, Toyooka S, et al. Validity of using lobe-specific regional lymph node stations to assist navigation during lymph node dissection in early stage non-small cell lung cancer patients. Surg Today 2014;44:2028-36. [Crossref] [PubMed]
- Kawano R, Hata E, Ikeda S, et al. Lobe-specific skip nodal metastasis in non-small cell lung cancer patients. Ann Thorac Cardiovasc Surg 2008;14:9-14. [PubMed]
- Shien K, Toyooka S, Soh J, et al. Clinicopathological characteristics and lymph node metastasis pathway of non-small-cell lung cancer located in the left lingular division. Interact Cardiovasc Thorac Surg 2015;20:791-6. [Crossref] [PubMed]
- Wang L, Jiang W, Zhan C, et al. Lymph node metastasis in clinical stage IA peripheral lung cancer. Lung Cancer 2015;90:41-6. [Crossref] [PubMed]
- Hattori A, Suzuki K, Matsunaga T, et al. Is Limited Resection Appropriate for Radiologically “Solid” Tumors in Small Lung Cancers? Ann Thorac Surg 2012;94:212-5. [Crossref] [PubMed]
- Hishida T, Miyaoka E, Yokoi K, et al. Lobe-Specific Nodal Dissection for Clinical Stage I and II NSCLC: Japanese Multi-Institutional Retrospective Study Using a Propensity Score Analysis. J Thorac Oncol 2016;11:1529-37. [Crossref] [PubMed]
- Adachi H, Sakamaki K, Nishii T, et al. Lobe-Specific Lymph Node Dissection as a Standard Procedure in Surgery for Non-Small Cell Lung Cancer: A Propensity Score Matching Study. J Thorac Oncol 2017;12:85-93. [Crossref] [PubMed]
- Maniwa T, Okumura T, Isaka M, et al. Recurrence of mediastinal node cancer after lobe-specific systematic nodal dissection for non-small-cell lung cancer. Eur J Cardiothorac Surg 2013;44:e59-64. [Crossref] [PubMed]
- Okada M, Sakamoto T, Yuki T, et al. Selective Mediastinal Lymphadenectomy for Clinico-Surgical Stage I Non–Small Cell Lung Cancer. Ann Thorac Surg 2006;81:1028-32. [Crossref] [PubMed]
- Ichinose J, Kohno T, Fujimori S, et al. Locoregional Control of Thoracoscopic Lobectomy With Selective Lymphadenectomy for Lung Cancer. Ann Thorac Surg 2010;90:235-9. [Crossref] [PubMed]
- Graham AN, Chan KJ, Pastorino U, et al. Systematic nodal dissection in the intrathoracic staging of patients with non-small cell lung cancer. J Thorac Cardiovasc Surg 1999;117:246-51. [Crossref] [PubMed]
- Riquet M, Rivera C, Pricopi C, et al. Is the lymphatic drainage of lung cancer lobe-specific? A surgical appraisal. Eur J Cardiothorac Surg 2015;47:543-9. [Crossref] [PubMed]


