Statins may be beneficial for patients with pulmonary hypertension secondary to lung diseases
Introduction
Pulmonary hypertension (PH) is a serious and progressive vascular disease, which is yet incurable and generally results in end-stage heart failure and death. Its prevalence is estimated at 97 persons per million with a female/male ratio of 1.8, and the mortality rate ranges from 4.5 to 12.3 per 100,000 population (1). The classification of PH includes pulmonary arterial hypertension (PAH, Group 1), PH due to left heart disease (Group 2), PH due to pulmonary diseases and/or hypoxia (Group 3), chronic thromboembolic PH (Group 4), as well as PH with unclear multifactorial mechanisms (Group 5) (1,2). Throughout the past twenty years, several drugs aimed at selectively targeting of PAH have been developed and approved for clinical use, such as phosphodiesterase-5 inhibitors, endothelin receptor antagonists, prostaglandins, and soluble guanylate cyclase stimulators (3). However, despite the improvements brought by these new pharmaceutical interventions, long-term prognosis for PAH patients remains poor, and what is even worse is that few treatment options are currently available for the other types of PH.
Statins, also known as 3-Hydroxy-3-methylglutaryl (HMG)-CoA reductase inhibitors, are the most common medications used to treat hyperlipoidemia. Beside of their effectiveness in lowering cholesterol, the latest researches have highlighted the pleiotropic properties of statins, including antiproliferative and anti-inflammatory effects (4). There is evidence that this is at least partially achieved through inhibition of isoprenoids synthesis, which is essential for the activation of Rho and Ras GTPases pathways (5-7). Of interest, a series of animal studies have demonstrated both attenuation in the development and regression of experimental PH by statin treatment, by restoring endothelial function and inhibiting smooth muscle cell proliferation, thus, suggested it as a novel potential therapeutic option (8-10). However, in contrast to these encouraging discoveries, the recent findings from clinical trials and systematic reviews that assessed the efficacy of statin in PH population are much more controversial (11,12).
The limited life expectancy with few effective treatments is a gloomy truth for both the patients suffered from PH and their physicians. In these circumstances, statins have attracted attentions in recent years, however, there are still no answers to the most critical questions: are statins really beneficial for PH patients, and if so, for which specific population? In this study, we conducted the first meta-analysis of peer-reviewed RCTs to investigate the clinical impacts of statins on PH secondary to lung diseases (Group 3). Our pooled analysis might provide a better understanding of the potential therapeutic effects of this drug class.
Methods
Search strategy
This systematic review and meta-analysis followed the preferred reporting items for systematic reviews and meta-analyses (PRISMA) criteria (13). Relevant articles were identified and selected by searching the databases: Medline (1966 to April 2017), Embase (1980 to April 2017), Web of Science (1994 to April 2017), Cochrane controlled trials register (The Cochrane Library Issue 4, 2017), and PubMed (updated to April 2017). The detailed information of the electronic search strategy was provided in the supplement. We scanned bibliographies in relevant articles and conference proceedings. No limitations on language, date, patients’ race or age were imposed. Internet-based sources of information on the results of clinical trials in PH were also searched. We also contacted authors for supplemental data when important information was missing.
Selection criteria
The following selection criteria were applied: (I) RCTs; (II) trials with a direct comparison between statins and control in patients with PH due to pulmonary diseases; (III) the trials should report at least one outcome of interest; (IV) a given patient population was used only once, if the same population appeared in other publications, only the most recent or complete report of a clinical trial was incorporated.
Data extraction
Data were independently abstracted from each study with a predesigned review form, and disagreement was resolved by consensus. We extracted data on study design, study characteristics, patient clinical characteristics and demographics, treatment information, results, and duration of follow-up. The primary outcome was 6-minute walk distance and pulmonary artery systolic pressure. The additional outcomes were all-cause mortality, drug discontinuation, low-density lipoprotein, and the most common adverse event (liver dysfunction).
Assessment of study quality
The quality of each fully published trial was assessed according to “The Cochrane Collaboration’s tool for assessing risk of bias” and “Jadad score” (14,15). Any disagreement was resolved by consensus.
Statistical analysis
The data analysis was performed using random-effect model with Stata/SE 11.0 (StataCorp, College Station, TX, USA). For studies reporting zero events in a treatment or control arm, we applied a classic half-integer continuity correction to calculate the relative risk (RR) and variance. For all dichotomous data, the RR and 95% confidence intervals (CIs) were calculated for each independent study and for the summary statistic, with values of <1 favoring statins. The Std mean difference (SMD) and 95% CIs were calculated for continuous data. The RR or SMD for each clinical event was considered as significant if P value less than 0.05 (two sided).
Results
Search results
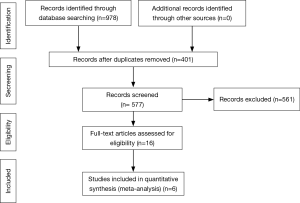
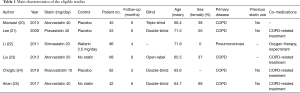
Our literature search yielded 978 potential relevant publications. From these, 10 RCTs comparing the treatment effects of statins with control in PH population were identified (16-25). As shown in Figure 1, 6 RCTs completely fulfilled the criteria for consideration and were further included in this meta-analysis (20-25). The general characteristics of the included trials were showed in Table 1. Each of the trials was performed in a separate single center. In addition, all of them were published as peer-reviewed articles, and the majority of them were in English, except for one (22). The selected studies were published between 2009 and 2017. These trials were conducted in 3 countries: China, Iran, and India.
Full table
Patients
The meta-analysis involved 366 participants with ultrasonically proven PH: 185 were randomized to the statin group and 181 to the control group. In our analysis, 5 trials assessed the therapeutic effects of statins in PH patients with chronic obstructive pulmonary disease (COPD), and the other study was based on PH due to pneumoconiosis (22). The statin medications investigated in the 6 trials included atorvastatin, pravastatin, simvastatin, and rosuvastatin.
Effects of intervention
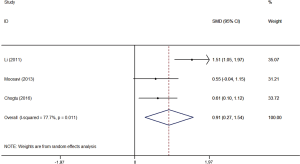
Six-minute walk distance
Figure 2 showed the change in 6-minute walk distance of patients with PH secondary to lung diseases after treatment with either statin or control. Our results showed that statin therapy significantly improved 6-minute walk distance in patients with PH due to pulmonary diseases, as compared to control (SMD, 0.91; 95% CI, 0.27–1.54; P=0.005). Additionally, another study which also determined the effect of statin on physical capacity but could not be included in this analysis, reported a prolonged exercise time in patients with COPD and PH, who were treated with pravastatin (21).
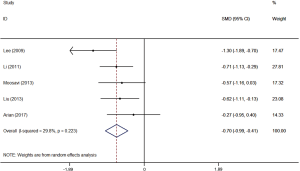
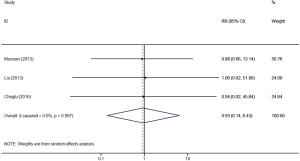
Pulmonary hemodynamics and mortality
In this study, non-invasive echocardiography was the solo method used to evaluate the change in pulmonary hemodynamics in the included patients. In agreement with our finding in 6-minute walk distance, statin treatment significantly reduced pulmonary artery systolic pressure in patients with PH due to lung diseases, as compared to statin non-users (SMD, –0.70; 95% CI, –0.99 to –0.41; P<0.001) (Figure 3). However, we found that the enhancements in exercise ability and pulmonary hemodynamics did not result in decreased mortality in patients with PH secondary to lung diseases (RR, 0.93; 95% CI, 0.14–6.43; P=0.94) (Figure 4).
Safety and side effects
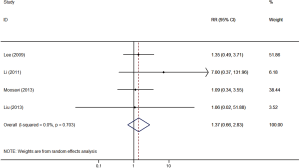
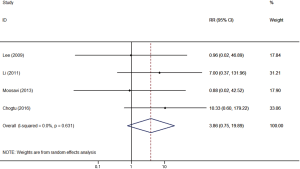
In general, statins were safe and well tolerated for patients with PH due to pulmonary diseases. Patient compliance with the treatment was confirmed by the significant impact of statins in reducing low-density lipoprotein (SMD, –1.17; 95% CI, –1.54 to –0.79; P<0.001). Our pooled results demonstrated that there was no statistical difference in withdrawal between statin users and control (RR, 1.37; 95% CI, 0.66–2.83; P=0.40) (Figure 5). All of the included trials reported no severe adverse events. In addition, as the most common side reaction, the incidence of liver dysfunction was comparable between the treatment and control groups (RR, 3.86; 95% CI, 0.75–19.89; P=0.11) (Figure 6).
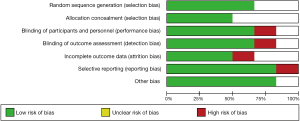
Study quality
Method of randomization and allocation concealment was described clearly in 4 trials (20,21,24,25). These trials were either double- or triple-blinded, except for two (22,23). All the included trials described withdrawals and drop-outs. Follow-up was completed in all the trials. The summary of the study quality assessment was presented in Figure 7.
Sensitivity analysis
A sensitivity analysis was conducted by using both random- and fixed-effect models, and practically the same outcomes were found, except the result of side effects, which favored the control group when under the fixed-effect model (RR, 4.76; 95% CI, 1.07–21.22; P=0.04). We performed two other sensitivity analyses by only including the placebo- or untreated-controlled studies, or RCTs based on patients with PH due to COPD, and no pooled results or the heterogeneity of this meta-analysis were significantly altered.
Discussion
To our knowledge, this is the first meta-analysis determining the potential therapeutic effects of statins in patients with PH secondary to lung diseases. Our results demonstrated that statin therapy is safe and well-tolerated in these patients. Furthermore, we found a possibly beneficial, statistically significant association between statin use and clinical outcomes of patients with PH due to pulmonary diseases.
Although being most widely prescribed as lipid-lowering agents, statins have attracted growing interests for the treatment of PH, with the underlying rationale related to the pathogenesis of PH and their pleiotropic functions (26). The well-known mechanisms for the occurrence and development of PH include pulmonary vascular remodeling, abnormal vasoconstriction, and thrombosis, which all lead to increased pulmonary arterial pressure and vascular resistance, as well as right heart failure. Seeming to aim at these pathophysiological alterations, statins have been shown to restrict vascular cell proliferation, improve endothelial function by increasing NO production, and inhibiting thrombogenic response, thus may exert a potential therapeutic benefit (27,28). Further molecular biology studies have revealed the related mechanisms, including downregulation of inflammatory genes, upregulation of p27Kip cell cycle inhibitor, and inhibition of Rho activity by suppressing isoprenoids synthesis (8,29,30).
The usefulness of various statins with different doses have been examined in the in vivo models for PAH and hypoxic PH. Although several studies indicated that statins, either alone or combined with other medications, were not really effective in reducing monocrotaline-induced PAH, most of the experimental researches reported that statins were able to reduce the pressure and resistance of pulmonary circulation, attenuate right ventricular hypertrophy, and reverse pulmonary vascular remodeling (9,10,31). Altogether, the results seemingly suggested a positive role of statin agents in the treatment for both PH classes.
In contrast to the encouraging evidences from the majority of animal researches, clinical data are more conflicting. Several observational studies have reported attenuation of PAH progression by statins, however, published meta-analysis of randomized trials demonstrated that statins may not be useful as a specific treatment for this disease (32-36). Among these statin-PAH RCTs, the only positive change in clinical outcomes was reported by Wilkins et al., who showed a small and early decrease in right ventricular mass with simvastatin use, but this is transient which was not maintained at 1 year (18). Another clinical trial showed reduced P-selectin concentration in PAH patients receiving rosuvastatin, however, this did not result in an advantage in exercise capacity (17). Kawut et al. even implied that simvastatin may have reduced the 6-minute walk distance and lead to more dyspnea (19).
Notably, unlike the disappointing findings from PAH trials and systematic reviews, we demonstrated that statins might be beneficial for patients with PH due to chronic pulmonary disease. Statin usage was associated with significantly enhanced exercise ability and improved pulmonary hemodynamics in this patient population. Although the exact mechanism was unknown, the inconsistency of therapeutic efficacy of statins in these two PH classes might lie in their different pathogenesis. Unlike PAH, Group 3 PH has determined etiology—pulmonary diseases and/or hypoxia, and mild PH is much more common in these patients (1,2). In addition, recent studies of statins have also suggested benefit in patients with COPD, which is the most common cause for Group 3 PH (37). Thus, we hypothesized that the efficient control of the primary disease by statins might be also helpful for treating the related PH.
This meta-analysis has several limitations. Not all the included RCTs described methods of randomization and adequate allocation concealment, and several of them did not apply blinded procedure. Furthermore, trials included in this analysis used varied types of statins with different doses. These potentially confounding factors might impact the analysis, and made it difficult to analyze the primary intervention of our interest. However, the inclusion of only studies with randomized controlled design and the use of random-effect model might be helpful to overcome this limitation. In addition, the robustness of this study was ascertained by our sensitivity analyses, which demonstrated that pooling the data on 6-minute walk distance and pulmonary hemodynamics did not alter the results of the analysis significantly by using different effect models, excluding the RCT involving pneumoconiosis patients, or the trial using warfarin as control. It should also be noted that, the diagnosis of PH and the assessment of pulmonary artery pressure during follow-up were made by using non-invasive echocardiographic method in all the included trials, which was normally associated a limited accuracy of measurement.
In conclusion, we found that statin therapy was associated with better exercise capacity and improved pulmonary hemodynamics in patients with PH due to pulmonary diseases. The current evidences do not support the routine use of statins in PAH; however, they seem to be a potential therapeutic option for patients with PH due to chronic lung diseases, although larger RCTs with more patients and longer observational duration are needed.
Acknowledgments
Funding: This work was supported by the National Natural Science Foundation of the People’s Republic of China (81570051).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS Guidelines for the Diagnosis and Treatment of Pulmonary Hypertension. Rev Esp Cardiol (Engl Ed) 2016;69:177. [Crossref] [PubMed]
- Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol 2013;62:D34-41. [Crossref] [PubMed]
- Fraidenburg D, Yuan J. Current and future therapeutic targets for pulmonary arterial hypertension. High Alt Med Biol 2013;14:134-43. [Crossref] [PubMed]
- Young RP, Hopkins R, Eaton TE. Pharmacological actions of statins: potential utility in COPD. Eur Respir Rev 2009;18:222-32. [Crossref] [PubMed]
- Wierzbicki AS, Poston R, Ferro A. The lipid and non-lipid effects of statins. Pharmacol Ther 2003;99:95-112. [Crossref] [PubMed]
- Takemoto M, Liao JK. Pleiotropic effects of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibitors. Arterioscler Thromb Vasc Biol 2001;21:1712-9. [Crossref] [PubMed]
- Oka M, Fagan KA, Jones PL, et al. Therapeutic potential of RhoA/Rho kinase inhibitors in pulmonary hypertension. Br J Pharmacol 2008;155:444-54. [Crossref] [PubMed]
- Nishimura T, Vaszar LT, Faul JL, et al. Simvastatin rescues rats from fatal pulmonary hypertension by inducing apoptosis of neointimal smooth muscle cells. Circulation 2003;108:1640-5. [Crossref] [PubMed]
- Nishimura T, Faul JL, Berry GJ, et al. Simvastatin attenuates smooth muscle neointimal proliferation and pulmonary hypertension in rats. Am J Respir Crit Care Med 2002;166:1403-8. [Crossref] [PubMed]
- Hsu HH, Ruan T, Ko WJ, et al. Effects of simvastatin on pulmonary C-fiber sensitivity in rats with monocrotaline-induced pulmonary hypertension. J Heart Lung Transplant 2011;30:332-40. [Crossref] [PubMed]
- Reed RM, Iacono A, DeFilippis A, et al. Statin therapy is associated with decreased pulmonary vascular pressures in severe COPD. COPD 2011;8:96-102. [Crossref] [PubMed]
- Zhang Y, Zeng W, Cheng S, et al. Efficacy and Safety of Statins for Pulmonary Hypertension: A Meta-Analysis of Randomised Controlled Trials. Heart Lung Circ 2017;26:425-32. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006-12. [Crossref] [PubMed]
- Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [Crossref] [PubMed]
- Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 1996;17:1-12. [Crossref] [PubMed]
- Zeng WJ, Xiong CM, Zhao L, et al. Atorvastatin in pulmonary arterial hypertension (APATH) study. Eur Respir J 2012;40:67-74. [Crossref] [PubMed]
- Barreto AC, Maeda NY, Soares RP, et al. Rosuvastatin and vascular dysfunction markers in pulmonary arterial hypertension: a placebo-controlled study. Braz J Med Biol Res 2008;41:657-63. [Crossref] [PubMed]
- Wilkins MR, Ali O, Bradlow W, et al. Simvastatin as a treatment for pulmonary hypertension trial. Am J Respir Crit Care Med 2010;181:1106-13. [Crossref] [PubMed]
- Kawut SM, Bagiella E, Lederer DJ, et al. Randomized clinical trial of aspirin and simvastatin for pulmonary arterial hypertension: ASA-STAT. Circulation 2011;123:2985-93. [Crossref] [PubMed]
- Moosavi SA, Raji H, Faghankhani M, et al. Evaluation of the Effects of Atorvastatin on the Treatment of Secondary Pulmonary Hypertension due to Chronic Obstructive Pulmonary Diseases: A Randomized Controlled Trial. Iran Red Crescent Med J 2013;15:649-54. [Crossref] [PubMed]
- Lee TM, Chen CC, Shen HN, et al. Effects of pravastatin on functional capacity in patients with chronic obstructive pulmonary disease and pulmonary hypertension. Clin Sci (Lond) 2009;116:497-505. [Crossref] [PubMed]
- Li DH, Wang CJ, Zhang SS, et al. Clinical study on simvastatin treatment of pulmonary hypertension in patients with coal worker's pneumoconiosis. Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 2011;29:230-1. [PubMed]
- Liu HF, Qi XW, Ma LL, et al. Atorvastatin improves endothelial progenitor cell function and reduces pulmonary hypertension in patients with chronic pulmonary heart disease. Exp Clin Cardiol 2013;18:e40-43. [PubMed]
- Chogtu B, Kuriachan S, Magazine R, et al. A prospective, randomized study: Evaluation of the effect of rosuvastatin in patients with chronic obstructive pulmonary disease and pulmonary hypertension. Indian J Pharmacol 2016;48:503-8. [Crossref] [PubMed]
- Arian A, Moghadam SG, Kazemi T, et al. The Effects of Statins on Pulmonary Artery Pressure in Patients with Chronic Obstructive Pulmonary Disease: A Randomized Controlled Trial. J Res Pharm Pract 2017;6:27-30. [Crossref] [PubMed]
- Dewachter L, Dewachter C, Naeije R. New therapies for pulmonary arterial hypertension: an update on current bench to bedside translation. Expert Opin Investig Drugs 2010;19:469-88. [Crossref] [PubMed]
- Athyros VG, Kakafika AI, Tziomalos K, et al. Pleiotropic effects of statins--clinical evidence. Curr Pharm Des 2009;15:479-89. [Crossref] [PubMed]
- Katsiki N, Tziomalos K, Chatzizisis Y, et al. Effect of HMG-CoA reductase inhibitors on vascular cell apoptosis: beneficial or detrimental? Atherosclerosis 2010;211:9-14. [Crossref] [PubMed]
- Laufs U, Liao JK. Post-transcriptional regulation of endothelial nitric oxide synthase mRNA stability by Rho GTPase. J Biol Chem 1998;273:24266-71. [Crossref] [PubMed]
- Loirand G, Guerin P, Pacaud P. Rho kinases in cardiovascular physiology and pathophysiology. Circ Res 2006;98:322-34. [Crossref] [PubMed]
- McMurtry MS, Bonnet S, Michelakis ED, et al. Statin therapy, alone or with rapamycin, does not reverse monocrotaline pulmonary arterial hypertension: the rapamcyin-atorvastatin-simvastatin study. Am J Physiol Lung Cell Mol Physiol 2007;293:L933-940. [Crossref] [PubMed]
- Kao PN. Simvastatin treatment of pulmonary hypertension: an observational case series. Chest 2005;127:1446-52. [PubMed]
- King WT, Day RW. Treatment of pediatric pulmonary hypertension with simvastatin: an observational study. Pediatr Pulmonol 2011;46:261-5. [Crossref] [PubMed]
- Rysz-Górzynska M, Gluba-Brzózka A, Sahebkar A, et al. Efficacy of Statin Therapy in Pulmonary Arterial Hypertension: A Systematic Review and Meta-Analysis. Sci Rep 2016;6:30060. [Crossref] [PubMed]
- Anand V, Garg S, Duval S, et al. A systematic review and meta-analysis of trials using statins in pulmonary arterial hypertension. Pulm Circ 2016;6:295-301. [Crossref] [PubMed]
- Wang L, Qu M, Chen Y, et al. Statins Have No Additional Benefit for Pulmonary Hypertension: A Meta-Analysis of Randomized Controlled Trials. PLoS One 2016;11:e0168101. [Crossref] [PubMed]
- Maneechotesuwan K, Wongkajornsilp A, Adcock IM, et al. Simvastatin Suppresses Airway IL-17 and Upregulates IL-10 in Patients With Stable COPD. Chest 2015;148:1164-76. [Crossref] [PubMed]