Robotic totally endoscopic coronary artery bypass for isolated ostial stenosis of the left coronary artery
Introduction
Isolated ostial stenosis (IOS) is an extremely rare disease of uncertain etiology. Incidence of 0.2% has been reported among 2,105 patients with angiographically defined coronary artery disease (1). IOS predominantly affects premenopausal young women with few risk factors for coronary heart disease. Most patients experience severe angina on exertion with short history, but preserve ventricular function even under high-grade ostial narrowing (2).
Prompt surgical revascularization is recommended to optimize myocardial salvage, which include coronary artery bypass grafting (CABG) (3) and saphenous vein patch angioplasty (4). With the advancement of robotic cardiac operations, totally endoscopic coronary artery bypass (TECAB) with sternum-sparing approach has been proved as a safe and reproducible alternative for coronary anastomosis (5-7). Here, we report a 40-year-old woman suffering from IOS of the left coronary artery. Robotic TECAB with left internal thoracic artery (LITA) graft was succeeded by five small incisions on the left chest.
Case presentation
A 40-year-old woman without coronary risk factors had experienced crescendo angina on exercise for 4 months. She was referred to our clinic because of positive treadmill test. Coronary computed tomographic angiography (CTA) disclosed an 85% stenosis of left main coronary ostium. She denied cocaine use, drugs, alcohol intake and oral contraceptive medication. In-hospital hematologic investigations and venereal disease research laboratory test were unremarkable. She underwent surgical revascularization a few days later.
After induction of general anesthesia, the patient was intubated for single-lung ventilation. She was placed in the supine position with the left chest slightly elevated using a small bolster. Percutaneous defibrillator pads were placed on the right anterior and left posterolateral chest. The da Vinci Si robotic patient cart (Intuitive Surgical Inc, Sunnyvale, CA, USA) approaches the patient perpendicular from the right side. A 12-mm camera port (ENDOPATH, Xcel Bladeless Trocar, Ethicon Inc, Somerville, NJ, USA) was initially introduced into the left 5th intercostal space (ICS) on the anterior axillary line. Carbon dioxide (5 mmHg) was insufflated to the left chest. The right and left robotic arm ports (8 mm) were introduced into the left third and seventh ICS on the anterior axillary line. A 11.5-mm working port (Thoracoport, Covidien Inc, Dublin, Ireland) was introduced into the left 4th ICS on the midaxillary line. With the use of EndoWrist instruments (Intuitive Surgical Inc, Sunnyvale, CA, USA), the LITA was securely detached from the chest wall in a skeletonized fashion
After systemic heparinization, cardiopulmonary bypass (CPB) was established with a 15-F superior vena cava cannula (Metronic, Minneapolis, MN, USA) in the right jugular vein and a 25-F inferior vena cava cannula in the left femoral vein. A 21-F arterial cannula was inserted in the left femoral artery for CPB inflows. Under CPB support, body temperature was lowered to 32 °C. The CPB flow index was maintained around 2.0 L/min/m2. Then, the heart was kept in empty and ventricular fibrillation under moderate hypothermia.
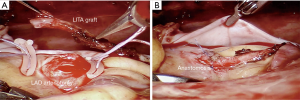
The LITA graft was divided from its distal end with robotic Pott’s scissors and secured clips. The left-assisted robotic arm was inserted through the left 6th ICS on the parasternal border to hold the epicardium and expose the left anterior descending (LAD) artery. A 6-mm-long arteriotomy was created by robotic bevel knife. Two silicone loops with blunt needle and pledget (DL0106-W, Wexler Surgical Inc, Houston, TX, USA) were applied at the both ends of arteriotomy for bleeding control (Figure 1A). The LITA graft was anastomosed to the LAD in an end-to-side fashion with a 7-0 polypropylene continuous suture (Ethicon Inc, Somerville, NJ, USA) (Figure 1B). Cardiac rhythm regained spontaneously after rewarming, and the patient was weaned from CPB. The total CPB time was 75 minutes. The total intraoperative blood loss was 100 mL. The LITA graft flow was 45 mL/min, identified by an intraoperative electromagnetic flowmeter measurement (Medistim VeriQ, Oslo, Norway). Two 10-mm C.W.V drainage tubes were placed through robotic ports into left pleural cavity. Finally, the port wounds and groin incisions were closed.
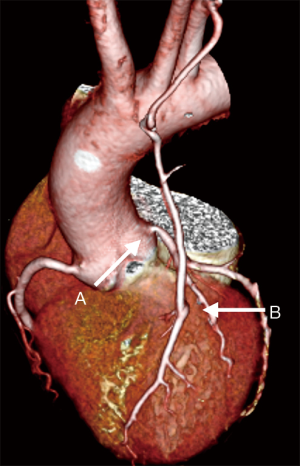
The patient was extubated 4 hours after the operation. Aspirin was commenced to prevent graft thrombosis. The length of hospital stay was 5 days. She resumed her daily tasks without difficulties on the next day after discharge. Postoperative CTA (Figure 2) revealed a high-grade stenosis on native left coronary ostium, and good opacification and distal runoff of the LITA graft.
Discussion
IOS has a unique feature that involve one or both main trunks of coronary artery without evidence of distal vessel obstruction. In addition, collateral circulation from ipsilateral or contralateral vessels is absent in angiography findings (1,2). The etiology remains unclear, but Takayasu arteritis (8), syphilitic aortitis (9), and iatrogenic causes (10) have been reported before. Despite early atheroma, which originates from the aortic wall and encroaches on aorto-coronary junction, are considered to cause ostial stenosis (1,2). The high incidence in premenopausal young women with few coronary risk factors and the different clinical characteristics cannot be entirely explained. Consequently, unknown inflammatory process possibly involves aorto-coronary junction and results in ostial stenosis (2,3).
Previous studies have presented high rates of restenosis and in-hospital mortality in both stenting and endarterectomy of ostial lesion (8). Therefore, CABG is a reasonable option for revascularization to prevent from the atherosclerotic plaque disruption, and the platelet aggregation. A long-term clinical review and angiographic follow-up of nine patients, by Arima and colleagues, has proved that CABG with LITA graft is safe and effective in treating IOS of the left coronary artery (3). Besides, saphenous vein patch angioplasty was also reported with acceptable long-term outcomes (4). However, these operations should be performed through full sternotomy.
With the development of robotic cardiac operations, series reports have demonstrated good reproducible results of TECAB for coronary revascularization, achieved either by beating heart (BH-TECAB) or arrested heart (AH-TECAB) (5-7). In our limited experiences, robotic TECAB for congenital coronary abnormalities takes great advantages of cosmetic appearance and speedy recovery, with equally high patency rates (11). In present case, we successfully perform robotic TECAB with LITA graft for IOS. CPB assistance with moderate hypothermic fibrillating heart could provide a steadily clear field for coronary anastomosis.
Although long-term follow-up are needed, robotic TECAB is a potentially feasible alternative for IOS patients, particularly in premenopausal young woman, with obvious benefits of tiny surgical wounds (Figure 3) and speedy recovery.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Thompson R. Isolated coronary ostial stenosis in women. J Am Coll Cardiol 1986;7:997-1003. [Crossref] [PubMed]
- Koh KK, Hwang HK, Kim PG, et al. Isolated left main coronary ostial stenosis in Oriental people: operative, histopathologic and clinical findings in six patients. J Am Coll Cardiol 1993;21:369-73. [Crossref] [PubMed]
- Arima M, Kanoh T, Okazaki S, et al. Long-term clinical and angiographic follow-up in patients with isolated ostial stenosis of the left coronary artery. Circ J 2009;73:1271-7. [Crossref] [PubMed]
- Botsios S, Maatz W, Sprengel U, et al. Patch angioplasty for isolated ostial stenosis of the left main coronary artery. J Card Surg 2008;23:743-6. [Crossref] [PubMed]
- Bonaros N, Schachner T, Lehr E, et al. Five hundred cases of robotic totally endoscopic coronary artery bypass grafting: predictors of success and safety. Ann Thorac Surg 2013;95:803-12. [Crossref] [PubMed]
- Srivastava S, Gadasalli S, Agusala M, et al. Beating heart totally endoscopic coronary artery bypass. Ann Thorac Surg 2010;89:1873-9; discussion 1879-80.
- Gao C, Yang M, Wu Y, et al. Early and midterm results of totally endoscopic coronary artery bypass grafting on the beating heart. J Thorac Cardiovasc Surg 2011;142:843-9. [Crossref] [PubMed]
- Rigatelli G, Zuin M, Picariello C, et al. Aortitis-related isolated bilateral coronary artery ostial stenosis in a young woman with acute coronary syndrome. Int J Cardiol 2016;223:111-2. [Crossref] [PubMed]
- Machado MN, Trindade PF, Miranda RC, et al. Bilateral ostial coronary lesion in cardiovascular syphilis: case report. Rev Bras Cir Cardiovasc 2008;23:129-31. [Crossref] [PubMed]
- Caus T, Canavy I, Mesana T, et al. Rescue revascularization for acute coronary occlusion late after radiotherapy. Ann Thorac Surg 1999;67:236-8. [Crossref] [PubMed]
- Kuo CC, Hsing CH, Cheng BC. Totally Endoscopic Coronary Artery Bypass for Anomalous Origin of Right Coronary Artery. Ann Thorac Surg 2017;103:e35-7. [Crossref] [PubMed]



