Semi-rigid single hook localization the best method for localizing ground glass opacities during video-assisted thoracoscopic surgery: re-aerated swine lung experimental and primary clinical results
Introduction
The widespread application of low-dose computed tomography (LDCT) has led to a great increase in the identification rate of small pulmonary nodules, especially small ground glass opacities (GGO). GGO is defined as a hazy opacity that does not obscure underlying bronchial structures or pulmonary vessels on CT scans (1). It has been reported that 33–60% GGO was malignant carcinoma when the nodules size ranges from 11–20 mm, while the malignant rate increase to 64–82% when the size grows up greater than 20 mm (2). Although the identification of pulmonary nodules could be effectively accomplished by many imaging modalities, including high-resolution CT, positron emission tomography (PET/CT), and bronchoscopy, whereas the identification of lesions with GGO remains difficult. Thus, more reliable diagnosis and therapeutic options for uncertain pulmonary nodules are still in need (3).
Video-assisted thoracoscopic surgery (VATS) is less invasive in diagnosing and treating thoracic lesions, thus how to locate and mark the nodules more precisely before the VATS becomes one of the most important issues, since GGO lesions on CT cannot be always palpated or visualized because of following factors: the texture of GGO is similar as the lung parenchyma thus hard to discern, too small, or too far from the visceral pleural surface (4). In decades, various techniques, including preoperative localization procedures, intraoperative localization using imaging modalities such as intraoperative ultrasonography, hook-wire, contrast media (5,6), dyes, microcoil, finger palpation, radio-guided, were used to overcome the aforementioned unfavorable factors, and the positive and negative aspects have been described (7). Along with the application of various localization methods and the accumulation of operating experience, numerous of doctors have been gradually recognized that physical methods such as hook wire localization showed excellent superiority (8-13). In addition, this method is also relatively safe, since the operating procedure takes shorter time. For example, pneumothorax, the most common complication, probably occurred due to the long procedure time (14), as well as the dislodgement (7). Preoperative localization of pulmonary nodules using combination of percutaneous CT-guided platinum microcoil insertion and operative fluoroscopic visualization is also a safer and more effective technique that increases the success rate of VATS excision (15-17).
The present study was designed to compare the effectiveness of double-thorn rigid hook wire, semi-rigid single hook wire and microcoil, the three most common methods in preoperative localization, using swine lung as an experimental model, followed by the observation of the efficacy and safety of the selected optimal method, semi-rigid single hook localization wire, in patients with small pulmonary nodules.
Methods
Localization experiment in swine lung
The swine experiment was reviewed and approved by the Animal Care Committee of the First Affiliated Hospital of Xiamen University. The swine was obtained from the Animal Facility of Xiamen University. The localization experiments were performed in fresh swine lungs using three location devices. The swine lung was intubated in trachea using aplastic pipe, 2 cm in diameter. A small household electric pump was used to make it most expansion. CT scanning was performed before and after the expansion respectively, and the difference was observed through the image (Figure 1).
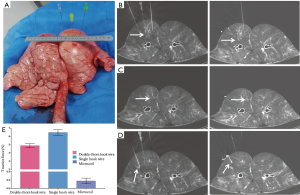
The localization devices we used were double-thorn hook wire (20-gauge needle, Dualok® Breast Lesion Localization needle, 10.7 cm of needle length), single semi-rigid hook wire (20-gauge needle, GHIATAS® Beaded Breast Localization Wire, 7 cm of needle length) and microcoil (diameter of 0.18, 7 cm of needle length Tornado® Embolization Micro-coil (Figure 1).
After the swine lung was placed in a proper position (generally placed supine position), a 10.7-cm long, 20-gauge cannula needle housing the 20-cm long double-thorn hook wire was gradually inserted about 3-cm deep into the right swine lung. Afterward, the other two devices were carried out in the same way as the double-thorn hook wire does and try to make the three cannulas in a same horizontal plane. Immediate follow-up CT scans were performed to identify if the hook has been deployed rightly in a same plane and depth into the lung parenchyma respectively, so we can see the three positioning locations on the same scanning plane synchronously (Figure 1). When we had the outer cannula needle withdraw, the horn of the hook wire was released and it naturally anchored the lung parenchyma. After the three localizations were fixed right in the lung, a CT scan was conducted to identify the position and the shape (if they have all expended) of the hook wires and microcoil (Figure 1). After all devices were in right places, 0.2 mL methylene blue was injected into the lung parenchyma via the cannula of single hook wire, to see the diffusion in the lung (Figure 2), and only this hook wire can be withdrawn after the cannula was inserted into the lung.
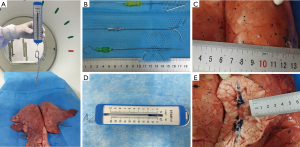
After identification, we pinched the semi-rigid wire and double-thorn wire with a spring dynamometer, for which we could make a relatively exact comparison about the tractions between them when we pushed them out from the lung parenchyma. And we pushed the micro-coil out of lung the same way as before. We have carried out such procedures 20 times in different position of lung parenchyma, and record the tractive force data obtained every time. The sizes of the wound which the devices leaved on the superior pleural were also measured by graduated scale (Figure 2). All the operations were done by the thoracic surgeon.
Patients
Between May 2016 and December 2016, 50 consecutive patients with 57 pulmonary nodules undergoing VATS resection for solitary pulmonary nodules (SPNs) with preoperative CT guided semi-rigid hook wire localization were prospectively reviewed.
Preoperative CT-guided hook wire localization was indicated when thoracic surgeons considered that detection of SPNs during VATS would be difficult (difficult to palpate). In case of solid nodules, hook wire localization was indicated for small nodules less than 10 mm or deeply located at a distance of >10 mm from the visceral pleura. Finally, five solid nodules were selected. Preoperative localization was also required for GGOs. All patients signed a written informed consent before localization and each case was discussed between the thoracic surgeon and radiologist prior to VATS.
Our selection for preoperative localization was based on at least one of the following CT findings: distance from the pleural surface >10 mm (solid nodules), a lesion diameter ≤10 mm, and a predominant ground-glass component.
CT-guided marker placement and thoracoscopic surgery
The CT-guided hook wire placements were performed on the day of operation. All procedures were performed under local anesthesia by an experienced radiologist and a thoracic surgeon. A CT scan was performed with the patient in a supine, prone, left or right lateral position depending on the site of the lesions to confirm the location. An initial CT examination was performed to identify the location of the tumor. After sterilization of skin around the puncture site and local anesthesia, a single semi-rigid hook wire was gradually inserted up to the pleura with sequential CT guidance (Figure 3) with the patient in breath-hold or inspiration. Then, when the outer cannula needle was withdrawn, the horn of the hook-wire would be released and anchor the parenchyma adjacent to the nodule instead of into it, to avoid the tumor from disseminating. A fourth image was obtained to confirm correct insertion of the localizer and check for if the needle has been inserted and advanced close to the nodule, but not into it. Procedure-related pneumothorax and hemorrhage were scrutinized after reading the immediate follow-up CT scans. Multiple marker placements were simultaneously performed in seven patients with 14 targeted lesions. The wire outside the skin surface was cut to about 1cm and covered with sterile gauze. Following the procedure, patients were moved to the operating room with a medical flat car as soon as possible (waited for about 0.5–1 hour before undergoing surgery).
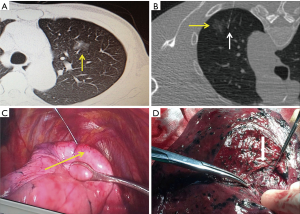
Thoracoscopic surgery was then performed under general anesthesia using single lung ventilation. VATS wedge resections were performed using a standardized three port approach with the camera placed in the seventh intercostal space on the mid axillary line. Fifty patients underwent 57 thoracoscopic wedge resection, for five of 50 patients, lobectomy and mediastinal lymph node dissection was conducted for invasive adenocarcinoma, seven patients underwent pulmonary wedge resection and lymph node sampling as the pathological results are micro-invasive adenocarcinoma. And the rest 38 patients were only performed wedge resection. The surgical method was determined on the basis of the National Comprehensive Cancer Network lung cancer guidelines (18).
Results
Results in swine experiment
All procedures the three localization systems that applied in the swine lung were successfully accomplished by CT guiding.
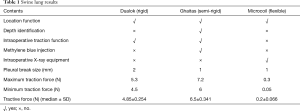
The semi rigid single hook wire had the largest force traction, the double-thorn hook wire ranked second, and the traction force of micro-coil was so such small that almost zero, which measured by a spring dynamometer, represented median ± SD tractive force “6.5±0.341 N”, “4.85±0.254 N” and “0.2±0.066 N” respectively. Of the 20 times we perform the procedures, maximum tractive force of the single semi-rigid, double-thorn hook wire and microcoil were 7.2, 5.3 and 0.3 N, and minimum tractive force of the two devices were 6, 4.5 and 0.05 N respectively. The comparisons between the three devices are clearly shown on Figure 1E and Table 1.
Full table
The sizes of the trauma in the superficial pleura that caused by unplugging the three needles were 2 mm in double-thorn hook wire, 1 mm in semi-rigid single hook and 1 mm in microcoil, respectively (Figure 2C). The double-thorn hook wire caused a greater damage to the pleura. All the three localizations were posted 3 cm deep into the lung parenchyma. The range of the methylene blues staining was 1.5 mm centered on the extremity of hook in the single hook wire test.
Single semi-rigid hook wire application in the clinical study and outcomes
The clinical study was conducted in 50 patients (18 men and 32 women) with their ages ranging from 44 to 66 years old, and the mean age is 55.8. Four patients underwent operations because of kidney malignancy, liver tumor, thyroid cancer and cervical cancer respectively, but there were no obvious surgical contra indications. The hook wires were successfully placed in all the nodules guiding by CT scan. Seven patients underwent two hook wire insertions simultaneously because of two nodules in the same lung. The mean diameter of the SPN at CT was 8.51 mm (range, 3–25 mm). The mean distance from the SPN to the pleura was 9.3 mm (range, 0–34.7 mm). Among all the nodules, the sizes of GGOs tend to be larger than 5 mm, whereas nodule diameter smaller than 5 mm were mostly be solid. The CT-feature of SPN showed GGO in 51 (89.5%) and solid nodules in 6 (10.5%). Forty-eight patients (96%) have no any complication in preoperative positioning. The patients and lesions characteristics are shown on Tables 2,3. The median and standard deviation of the size, distance and procedure time are detailed on Table 3.
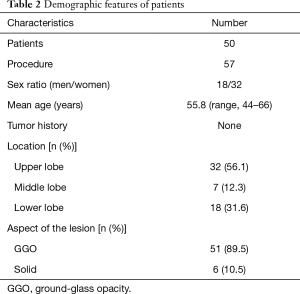
Full table
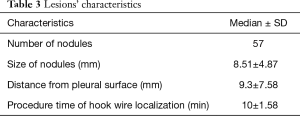
Full table
Dislodgment of the hook wire occurred in one patients (1.8%). However, VATS resection was successfully accomplished in the patients by locating the lung puncture site. After hook wire placement, CT-scan revealed the presence of pneumothorax and parenchymal bleeding in one patient (3.3%) with no respiratory symptoms. The mean operate time of the localization was 10 min (range, 10–14 min) per lesion. The time to operate the surgical procedures ranged from 35 to 120 min which was less than previously reported. The interval from localization to surgery was about half an hour. No dislodgement was observed during the procedures. In needlescopy, the hook wire was placed correctly and was helpful in locating the target lesion. The wire was smoothly pulled in the pleural cavity without dislodging when the lung collapsed. We used the injected hook wire not only as a handle for traction during surgery but also as a visible marker. Table 4 summarizes the results of the complications in preoperative procedures and histological examination of the excised GGO.
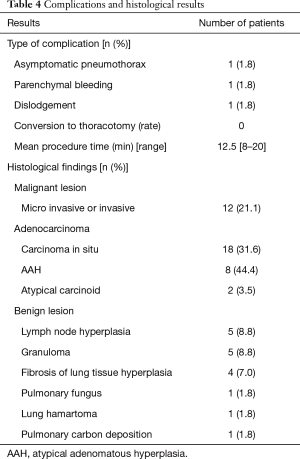
Full table
No patient was needed to convert to thoracotomy. Small pulmonary nodules were localized in the upper, lower and middle lobe in 56.1%, 31.6% and 12.3% respectively. Table 4 summarizes results of the histological findings of the resected SPN. Malignant disease was found in 40 nodules (70.2%) including micro invasive and invasive adenocarcinoma and 17 benign nodules (29.8%) including lymphnode hyperplasia tissue, granuloma, fibrosis of lung tissue hyperplasia and lung hamartoma and so on.
Discussion
Invasive positioning techniques were widely used in locating pulmonary nodules before operation, and it inevitably cause a risk of complications such as pneumothorax, pulmonary hemorrhage, and cough. Hook-wire position is one of the invasive locating techniques, it has been reported that the hook-wire locating device may cause multiple complications, particularly dislodgement. In the present study, we chose the double-thorn, single semi-rigid hook wire and microcoil to make a comparison between them through swine lung. An interesting result came to us that the double-thorn hook wire didn’t have a greater traction as it generally supposed to be. We also found that the wound sizes, caused by unplugging of the needle in the superficial pleura, were different. This happens in the human lungs as well, and we could deduce that the single semi-rigid hook wire may lead to a low probability of complication including pneumothorax or pulmonary hematoma. Thus, the semi-rigid hook wire could have a better feasibility and a lower dislodgement rate in the preoperative localization for patients in VATS resection. Thus, we choose semi-rigid single hook wire in locating the lung nodules for lower dislodgement and better operability.
There are several reasons that the results came to the experiment as the following points: (I) the hook in the distal of double-thorn hook wire is semicircle so that as we push it out, the resistance generated from lung parenchyma is relatively smaller because the radian of the double-thorn is easy to change; (II) whether semi-rigid hook wire, the distal end of the hook showed an acute angel, as we push wire out, the hook is much harder to up straight so that it can produce greater resistance against the drag force we performed; (III) furthermore, its characteristic of relatively soft make it more easy to use in the operation when the surgeon tug the collapse lung.
In recent years, with the development of minimally invasive thoracic surgery, VATS has been widely accepted for providing a minimally invasive way to the patients with lung lesions, but conversion thoracotomy was sometime necessary because preoperative localization of small pulmonary nodules was inadequate. There have been several techniques used in locating the lung nodules during the VATS resection already. Methylene blue injection carries the risk of spreading the colorant on the pleural surface and the chest cavity during application, which renders subsequent operation difficult, especially in patients with extensive anthracotic swine mentation (7,19). Finger palpation for millimeter nodules is also difficult depending on the composition of the lesion and the distance from the pleura (7). Davini et al. and Gonfiotti et al. introduced the method of radio-guided localization of SPN, the disadvantages of this technique are the requirement of radionuclide injection, a magnetic probe connected to a gamma camera, and increased exposure to radiation (20,21). Intraoperative ultrasound localization of SPN prefers more operator compliance and requires complete collapse of the assessed lung, which is difficult to apply in emphysematous lung.
Previous study has also shown that methylene blue staining of the nodules produced high sensitivities. The use of methylene blue may also be limited in patients with anthracotic swine mentation for it is difficult to see during VATS. While, hook wires, do not require intraoperative fluoroscopy to detect targets, perform better in resecting small pulmonary nodules via VATS for the short procedure time, precise wedge resection and a better intraoperative manipulation (lift up the lung for wedge resection) (9,10,12,13,22,23). Kastl (8) hold the point that hook wires are easily dislodged, resulting in high failure rates. Some researchers have reported that dislodgement rate in VATS resection with CT-guided single hook wire localization ranging from 0.4–4.9% (22,24,25). Compared to other reviews, the dislodgement rate in double-thorn hook wire applied by Chen (26) is up to 7%, whose incidence is within the 8–20% range reported in the literature (27,28). While, our clinical experience, only one patient (1.8%) presented dislodgement of the hook wire, much lesser than reported above. The single semi-rigid hook wire applied in our series had a promising result. In order to prevent such incidents from occurring, we took the following measures such as telling patients to breathe calmly and keep the upper body stationary after the localization. With the forementioned situation, we deduce that dislodgement of the hook wire is mostly related to the size and depth of the nodule. The larger and deeper it occurs, the greater the traction force that is required to raising the lung, accordingly the risk of dislodgement increased. The advantage of the single semi-rigid hook wire over other devices is the acute angel distal at the end of the hook. Its ability to be repositioned is also superior to double-thorn hook wire.
Pneumothorax and pulmonary hemorrhage are reportedly as primary complications of hook wire method. Studies have showed that pneumothorax and pulmonary hemorrhage, with an incidence of 32.1–68% and 10.3–36%, respectively, in preoperative hook wire placement (22,29,30). Ichinose and colleagues represented similar result, of 500 lesions underwent CT-guided localization, pneumothorax was observed in 49% of the patients immediately after location, only 4.6% require intervention (22), much higher than other study (apply double-thorn hook wire) reported (18.6% and 24.4%) (23). While the pneumothorax induced by double-thorn hook wire is lower than the single semi-rigid hook wire mentioned above. However, because of our experienced radiologist and surgeon, patients without basic lung disease (for example marked emphysema) and the soft features of the device in our situation, only one patient underwent asymptomatic pneumothorax and pulmonary hemorrhage after localization. Pulmonary hemorrhage could possibly be caused by temporary piercing between the bronchiole and adjacent pulmonary vein. Venous air embolism has been reported to be the most serious complication of CT-guided needle biopsy and localization previously. The incidence of venous air embolism during CT-guided needle biopsy has been reported lower than other complications (0.21% to 0.49%) (31,32). It was not observed in the present study which might be associated with the following reasons: (I) shortest trajectory was chosen and pulmonary vasculature was avoided as far as possible during localization procedure; (II) patients were told to avoid breathing deeply during and after localization procedure.
Previous study (30) showed that the malignancy rates were 63% for part-solid GGO, 18% for pure GGO, and only 7% for solid nodules, similar to ours. Because of the small number cases, our data just can’t reflect the probability well despite the fact that the malignancy rate is up to 60%.
The swine model used in our study may have difference with human in biological behavior. In addition, the animal experiments are ex vivo, therefore, how the wires and microcoil were placed is not the same as in the humans. Furthermore, the number of cases in our study is limited, well-designed clinical trials with larger patient populations are ongoing.
Conclusions
In summary, our findings indicate that the preoperative single semi-rigid hook wire localization has excellent feasibility and operability in preoperative localization, with higher success rate and lower dislodgement, compared the other two commonly used methods, double-thorn hook wire and microcoil. Further studies are needed to confirm the efficacy and safety of semi-rigid single hook localization wire in VATS in GGO with large sample sizes.
Acknowledgements
Funding: This work was supported by Xiamen City Major Joint Research Project (No.3502Z201590 13), Fujian Science and Technology Department (No.2014D020, 2015J01546, 2016J01636).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the institutional review board of the first affiliated Hospital of Xiamen University (No. 3502Z20159013).
References
- Austin JH, Müller NL, Friedman PJ, et al. Glossary of terms for CT of the lungs: recommendations of the Nomenclature Committee of the Fleischner Society. Radiology 1996;200:327-31. [Crossref] [PubMed]
- Gould MK, Fletcher J, Iannettoni MD, et al. Evaluation of patients with pulmonary nodules: when is it lung cancer?: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 2007;132:108S-30S.
- Ng YL, Patsios D, Roberts H, et al. CT-guided percutaneous fine-needle aspiration biopsy of pulmonary nodules measuring 10 mm or less. Clin Radiol 2008;63:272-7. [Crossref] [PubMed]
- Nakashima S, Watanabe A, Obama T, et al. Need for Preoperative Computed Tomography-Guided Localization in Video-Assisted Thoracoscopic Surgery Pulmonary Resections of Metastatic Pulmonary Nodules. Ann Thorac Surg 2010;89:212-8. [Crossref] [PubMed]
- Iwasaki Y, Nagata K, Yuba T, et al. Fluoroscopy-guided barium marking for localizing small pulmonary lesions before video-assisted thoracic surgery. Respir Med 2005;99:285-9. [Crossref] [PubMed]
- Watanabe K, Nomori H, Ohtsuka T, et al. Usefulness and complications of computed tomography-guided lipiodol marking for fluoroscopy-assisted thoracoscopic resection of small pulmonary nodules: experience with 174 nodules. J Thorac Cardiovasc Surg 2006;132:320-4. [Crossref] [PubMed]
- Zaman M, Bilal H, Woo CY, et al. In patients undergoing video-assisted thoracoscopic surgery excision, what is the best way to locate a subcentimetre solitary pulmonary nodule in order to achieve successful excision? Interact Cardiovasc Thorac Surg 2012;15:266-72. [Crossref] [PubMed]
- Kastl S, Langwieler TE, Krupski-Berdien G, et al. Percutaneous localization of pulmonary nodules prior to thoracoscopic surgery by CT-guided hook-wire. Anticancer Res 2006;26:3123-6. [PubMed]
- Hanauer M, Perentes JY, Krueger T, et al. Pre-operative localization of solitary pulmonary nodules with computed tomography-guided hook wire: report of 181 patients. J Cardiothorac Surg 2016;11:5. [Crossref] [PubMed]
- Pittet O, Christodoulou M, Pezzetta E, et al. Video-assisted Thoracoscopic Resection of a Small Pulmonary Nodule after Computed Tomography–guided Localization with a Hook-wire System. World J Surg 2007;31:575-8. [Crossref] [PubMed]
- Iguchi T, Hiraki T, Gobara H, et al. Simultaneous Multiple Preoperative Localizations of Small Pulmonary Lesions Using a Short Hook Wire and Suture System. Cardiovasc Intervent Radiol 2015;38:971-6. [Crossref] [PubMed]
- Xu X, Yao Y, Shen Y, et al. Clinical Analysis of Percutaneous Computed Tomography–Guided Hook Wire Localization of 168 Small Pulmonary Nodules. Ann Thorac Surg 2015;100:1861-7. [Crossref] [PubMed]
- Miyoshi K, Toyooka S, Gobara H, et al. Clinical outcomes of short hook wire and suture marking system in thoracoscopic resection for pulmonary nodules. Eur J Cardiothorac Surg 2009;36:378-82. [Crossref] [PubMed]
- Iguchi T, Hiraki T, Gobara H, et al. CT fluoroscopy-guided preoperative short hook wire placement for small pulmonary lesions: evaluation of safety and identification of risk factors for pneumothorax. Eur Radiol 2016;26:114-21. [Crossref] [PubMed]
- Powell TI, Jangra D, Clifton JC, et al. Peripheral lung nodules: fluoroscopically guided video-assisted thoracoscopic resection after computed tomography-guided localization using platinum microcoils. Ann Surg 2004;240:481-8; discussion 488-9. [Crossref] [PubMed]
- Su TH, Fan YF, Jin L, et al. CT-guided localization of small pulmonary nodules using adjacent microcoil implantation prior to video-assisted thoracoscopic surgical resection. Eur Radiol 2015;25:2627-33. [Crossref] [PubMed]
- Sui X, Zhao H, Yang F, et al. Computed tomography guided microcoil localization for pulmonary small nodules and ground-glass opacity prior to thoracoscopic resection. J Thorac Dis 2015;7:1580-7. [PubMed]
- Ettinger DS, Wood DE, Aisner DL, et al. Non-Small Cell Lung Cancer, Version 5.2017, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2017;15:504-35. [Crossref] [PubMed]
- Kerrigan DC, Spence PA, Crittenden MD, et al. Methylene blue guidance for simplified resection of a lung lesion. Ann Thorac Surg 1992;53:163-4. [Crossref] [PubMed]
- Davini F, Gonfiotti A, Vaggelli L, et al. Thoracoscopic localization techniques for patients with solitary pulmonary nodule: radioguided surgery versus hookwire localization. J Cardiovasc Surg (Torino) 2006;47:355-9. [PubMed]
- Gonfiotti A, Davini F, Vaggelli L, et al. Thoracoscopic localization techniques for patients with solitary pulmonary nodule: hookwire versus radio-guided surgery. Eur J Cardiothorac Surg 2007;32:843-7. [Crossref] [PubMed]
- Ichinose J, Kohno T, Fujimori S, et al. Efficacy and complications of computed tomography-guided hook wire localization. Ann Thorac Surg 2013;96:1203-8. [Crossref] [PubMed]
- Chen S, Zhou J, Zhang J, et al. Video-assisted thoracoscopic solitary pulmonary nodule resection after CT-guided hookwire localization: 43 cases report and literature review. Surg Endosc 2011;25:1723-9. [Crossref] [PubMed]
- Lenglinger FX, Schwarz CD, Artmann W. Localization of pulmonary nodules before thoracoscopic surgery: value of percutaneous staining with methylene blue. Ajr American Journal of Roentgenology 1994;163:297-300. [Crossref] [PubMed]
- Li W, Zhai CB, Guan YJ, et al. Preoperative computed tomography-guided hook-wire positioning of pulmonary nodules. Genet Mol Res 2015;14:3798-806. [Crossref] [PubMed]
- Chen YR, Yeow KM, Lee JY, et al. CT-guided Hook Wire Localization of Subpleural Lung Lesions for Video-assisted Thoracoscopic Surgery (VATS). J Formos Med Assoc 2007;106:911-8. [Crossref] [PubMed]
- Mack MJ, Shennib H, Landreneau RJ, et al. Techniques for localization of pulmonary nodules for thoracoscopic resection. J Thorac Cardiovasc Surg 1993;106:550-3. [PubMed]
- Thaete FL, Peterson MS, Plunkett MB, et al. Computed tomography-guided wire localization of pulmonary lesions before thoracoscopic resection: results in 101 cases. J Thorac Imaging 1999;14:90-8. [Crossref] [PubMed]
- Dendo S, Kanazawa S, Ando A, et al. Preoperative Localization of Small Pulmonary Lesions with a Short Hook Wire and Suture System: Experience with 168 Procedures1. Radiology 2002;225:511-8. [Crossref] [PubMed]
- Seo JM, Lee HY, Kim HK, et al. Factors determining successful computed tomography-guided localization of lung nodules. J Thorac Cardiovasc Surg 2012;143:809-14. [Crossref] [PubMed]
- Kuo HL, Cheng L, Chung TJ. Systemic air embolism detected during percutaneous transthoracic needle biopsy: report of two cases and a proposal for a routine postprocedure computed tomography scan of the aorto-cardiac region. Clin Imaging 2010;34:53-6. [Crossref] [PubMed]
- Freund MC, Johannes P, Goder KC, et al. Systemic air embolism during percutaneous core needle biopsy of the lung: frequency and risk factors. BMC Pulm Med 2012;12:2. [Crossref] [PubMed]


