Pathway and application value of exploration of the pulmonary artery by endobronchial ultrasound
Introduction
Pulmonary disease, especially pulmonary embolism is a common clinical disease. The standard diagnostic methods are pulmonary artery enhanced computed tomography (CT) scan and pulmonary angiography. But the contrast allergy and contrast associated nephropathy limit its applications in patients with allergic constitution or renal insufficiency. Additional inspection radiation is not suitable for pregnant women either. These patients with pulmonary artery disease are difficult to diagnose timely.
Endobronchial ultrasound (EBUS) has been used in clinical practice since 2002, and currently is used primarily for transbronchial needle aspiration (TBNA), or EBUS-TBNA, which has been widely used in the diagnosis of mediastinal and hilum occupying lesions and in the lymph node staging of lung cancer (1-3). EBUS has a function of color Doppler flow imaging, which avoids the penetration of the fine needle into the blood vessel. Detection of blood vessel diseases inside the thoracic cavity using EBUS has not been fully determined. EBUS has been used to detect pulmonary artery embolisms with case reports (4-6) and a small-sample study (7). It has also been reported that EBUS could be used to explore various rare pulmonary vascular diseases (8).
The presence of a tumor in the pulmonary vasculature is associated with a high risk for pulmonary embolism, the tumor itself can also cause vascular invasion, as well as the potential for thromboembolism in the blood vessels outside the airway. Therefore, tumor invasion status should be evaluated in patients with suspected chest tumors who have been evaluated using the EBUS test (9). However, EBUS is not routinely used for exploring the blood vessels outside the airway in clinical practice. Moreover, there is no standard process for pulmonary artery exploration, and most endoscopic physicians are not familiar with the vascular anatomy around the airways.
In order to explore the pulmonary arteries outside the airways in a more systematic, comprehensive and effective manner, we sought to establish a process and roadmap for EBUS exploration. The purpose of this study is to help the bronchoscopists to quickly grasp the anatomical structures and imaging characteristics of the pulmonary arteries outside the airways.
Methods
Subjects
The study cohort included patients who underwent EBUS examination between June 2015 and October 2016. The study protocol was approved by the Ethics Committee of Shengjing Hospital of China Medical University (No. 2015PS61J). Informed consent was obtained from each patient before EBUS examination.
All subjects were adults with occupying lesions in the mediastinum or the hilum of the lung initially identified by contrast-enhanced CT or positron emission tomography/computed tomography (PET/CT), and which required further diagnosis by the EBUS-TBNA technique. Patients were excluded if they could not tolerate conventional bronchoscopy and EBUS-TBNA.
Equipments
Contrast-enhanced chest CT
The types of CT machines used for the inspection included TOSHIBA Aquilion ONE, SIEMENS SOMATOM Definition, Philips Ingenuity Core 128 and Philips iCT 256 in the current study.
EBUS systems
For all subjects, the EBUS equipment (PENTAX EB-1970UK, Tokyo, Japan) and ultrasound system (HITACHI Hi-vision Avius®, Hitachi Medical Systems, Kashiwa, Japan) were used. Equipment parameters: the outer diameter of the insertion part was 7.4 mm, the diameter of the working channel was 2.0 mm, the oblique view angle was 45 degrees, the scanning frequency was 5–10 MHz, and the depth of field was 50 mm. The ultrasound system integrates color Doppler scanning function.
Research methods
The EBUS examination sites were selected according to the anatomical markers of the airway and the characteristics of the pulmonary artery distribution based on normal contrast-enhanced CT images. The sites of exploration and the route of scanning were established based on the brief pulmonary arteries exploration procedure previously described (7).
EBUS was performed at the Department of Endoscopic Diagnosis and Treatment Center, Shengjing Hospital, China Medical University, using the nasal or oral approach with the patient under local anesthesia and moderate sedation with 2 mg midazolam given intravenously (10). Heart rate and oxygen saturation were monitored continuously. Pulmonary artery exploration was carried out during the treatment of TBNA specimens. Based on the obtained CT images of subjects, we designed the scanning routes and then actual exploration was performed. The EBUS probe was placed first at the distal site of the left/right bronchus, then the pulmonary artery was explored along the line of the adjacent sites. The continuity and integrity of the pulmonary artery were observed. After the examination of one side, the probe was placed at the other side of the bronchus. The ultrasound images of the corresponding sites were saved and the information related to the pulmonary artery was recorded.
Results
Fourteen subjects underwent pulmonary artery exploration using EBUS (8 males and 6 females) with a mean age of 54.8±11.2 years. These subjects were all conformed to the routine indications of EBUS-TBNA examination. In order to avoid detection errors, we only examined the unaffected side of pulmonary artery. B-mode ultrasound was used for 13 subjects, color Doppler ultrasound was used for 10 subjects, and both methods were used for 9 subjects successively. Bilateral pulmonary arteries were explored in 9 cases, and unilateral pulmonary artery was explored in 5 cases. The mean time of exploring each pulmonary artery was 41.95±12.46 s. The procedure leaded to coughing or coughing aggravation in 5 cases (35.7%), and resulted in small mucosal bleeding in 2 cases (14.3%) . Adverse reactions (cough, bleeding, etc.) were mild and examinations were not affected. The procedure was well tolerated (Table 1).
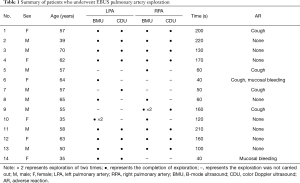
Full table
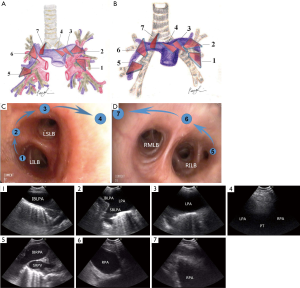
To summarize the procedure of exploring the pulmonary artery by EBUS, a flowchart of pulmonary artery exploration was developed (Table 2) with an anatomical map and related ultrasound images corresponding to the different exploration sites (Figure 1). The present study explored normal pulmonary arteries and as expected no significant abnormalities were found during the procedure, which is consistent with the result of preoperative CT imaging.

Full table
Discussion
The clinical application of EBUS is principally guiding TBNA (11-15). Some investigators used EBUS as a tool for detecting pulmonary vascular abnormalities, including the pulmonary thromboembolism and non-thromboembolic pulmonary vascular diseases. A prospective, multicenter pilot study investigated the ability of EBUS in the diagnosis of the pulmonary embolism. For central thromboembolism patients with stable haemodynamics, at least one pulmonary embolism is detected by EBUS for each enrolled patient (7). Non-thromboembolic pulmonary vascular lesions include pulmonary artery sarcoma (16-20), pulmonary artery metastasis of tumors (21-24) or septic pulmonary artery embolisms (25,26). Considering the high sensitivity and specificity of EBUS-TBNA in the diagnosis of mediastinal and hilar tumors, and the high risk associated with these tumors for pulmonary embolism, the exploration and evaluation of the pulmonary artery to identify possible pulmonary embolism when performing EBUS-TBNA has potentially important clinical significance. In addition, EBUS pulmonary artery exploration may have value for patients who cannot undergo contrast-enhanced chest CT or ECT scan due to renal insufficiency or pregnancy (27).
Aumiller et al. (7) described pulmonary artery exploration by EBUS briefly and mentioned that pulmonary artery exploration started from the right lower pulmonary artery to the pulmonary trunk along with the right pulmonary artery, and vice-versa on the left pulmonary artery. However, no further details or illustrations of the procedure were reported. In the present study, we referred to Aumiller et al. and started our exploration from the left lower pulmonary artery, passed four markers continuously, and then started again from the right lower pulmonary artery, and passed three markers continuously to complete pulmonary artery exploration. We drew two anatomical illustrations (Figure 1A,B) to help identify the structures of the tissues outside the airway during ultrasound examination. We also drew bronchoscopic roadmap illustrations (Figure 1C,D) to help understand the route of exploration. In this way, we hope to make clinical application of EBUS more efficient and standardized.
After establishing the markers and roadmaps of pulmonary artery exploration, we tried to observe the pulmonary artery continuously in patients who underwent EBUS-TBNA, and found that this method could identify the status of the pulmonary artery, as well as observe continuously the blood flow of pulmonary artery by color Doppler mode. We also demonstrated that the results of EBUS exploration are in good agreement with the results of enhanced CT, which suggested it was feasible to explore and study pulmonary artery by EBUS. As for the first exploration of the left or right pulmonary artery, it could be determined according to the operator’s habit and didn’t affect the evaluation of the pulmonary artery. In the present study, some patients (6/14) had small amounts of mucosal bleeding and mild coughing during the procedure, and overall patient response were well tolerated. It took a short time to explore the pulmonary artery, and we can insert the exploration work during handling TBNA specimens (28). Therefore, there is no significant increase in the operating time of the EBUS-TBNA.
There are some limitations in the exploration of the pulmonary artery by EBUS. (I) In this study, the imaging quality of the probe could not be closely fitted to the airway sometime because of no water sac used, and the imaging quality would be improved if the water sac was applied (29). (II) The diameter of the EBUS probe is generally about 7 mm, which is larger than the ordinary bronchoscope, and thereby the probe is difficult to enter the lobar bronchus. One study reported that EBUS could explore a bronchus with a diameter ≥4.5 mm (30). EBUS probe entering each of the finer bronchus will increase mucosal damage and patient discomfort, so its advantages and disadvantages need further study. Because of the limitations mentioned above, the pulmonary embolism located in the pulmonary artery around the lobar and finer bronchus might be missed. (III) Due to the limitation in the flexibility of the EBUS equipment, exploration of some bronchi, such as the bilateral upper lobe bronchi, is difficult. The probe is often unable to fit tightly against the wall of the airway, which results in failed imaging of the pulmonary artery outside the airway. (IV) The pulmonary trunk is not located near the airway, and imaging of it was not clear under the EBUS, and thereby embolism in pulmonary trunk may be missed. (V) Similar to other ultrasound probes, the EBUS probe may induce artifacts during the exploration. Especially, multiple reflections and side lobe artifacts are easily misdiagnosed as pulmonary artery abnormalities, and beginners should pay enough attention to that.
Conclusions
In conclusion, EBUS pulmonary artery exploration has value in the diagnosis of pulmonary artery abnormalities, especially for patients who cannot tolerate contrast-enhanced chest CT examination—a prospective study should be designed for these patients to further evaluate. In the near future, the EBUS equipment may become smaller and the ultrasound probe functions more powerful, such as contrast-enhanced ultrasound (31), thereby enhancing its usefulness in the diagnosis and treatment of pulmonary artery diseases.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the ethics committee of Shengjing Hospital of China Medical University (No. 2015PS61J). Written informed consent was obtained from all patients.
References
- Varela-Lema L, Fernández-Villar A, Ruano-Ravina A. Effectiveness and safety of endobronchial ultrasound-transbronchial needle aspiration: a systematic review. Eur Respir J 2009;33:1156-64. [Crossref] [PubMed]
- Grigorescu AC. Chemotherapy for elderly patients with advanced cancer: A pilot study in Institute of Oncology Bucharest. J Transl Int Med 2015;3:24-8. [Crossref] [PubMed]
- Erer OF, Erol S, Anar C, et al. Contribution of cell block obtained by endobronchial ultrasound-guided transbronchial needle aspiration in the diagnosis of malignant diseases and sarcoidosis. Endosc Ultrasound 2017;6:265-8. [Crossref] [PubMed]
- Şentürk A, Argüder E, Babaoğlu E, et al. Diagnostic imaging of pulmonary embolism using endobronchial ultrasound. Arch Bronconeumol 2013;49:268-71. [Crossref] [PubMed]
- Goyal R, Chachra V, Gogia P. Diagnosis of pulmonary embolism by endobronchial ultrasound. Lung India 2015;32:606-8. [Crossref] [PubMed]
- Dhillon SS, Harris K. Endobronchial ultrasound for the detection of chronic pulmonary artery thrombus. Endosc Ultrasound 2016;5:272-3. [Crossref] [PubMed]
- Aumiller J, Herth FJ, Krasnik M, et al. Endobronchial ultrasound for detecting central pulmonary emboli: a pilot study. Respiration 2009;77:298-302. [Crossref] [PubMed]
- Li P, Zheng W, Zhao L. Convex probe endobronchial ultrasound: applications beyond conventional indications. J Thorac Dis 2015;7:E289-97. [PubMed]
- Harris K, Modi K, Kumar A, et al. Endobronchial ultrasound-guided transbronchial needle aspiration of pulmonary artery tumors: A systematic review (with video). Endosc Ultrasound 2015;4:191-7. [Crossref] [PubMed]
- Aswanetmanee P, Limsuwat C, Kabach M, et al. The role of sedation in endobronchial ultrasound-guided transbronchial needle aspiration: Systematic review. Endosc Ultrasound 2016;5:300-6. [Crossref] [PubMed]
- Konge L, Colella S, Vilmann P, et al. How to learn and to perform endoscopic ultrasound and endobronchial ultrasound for lung cancer staging: A structured guide and review. Endosc Ultrasound 2015;4:4-9. [Crossref] [PubMed]
- Grouse L. Translational genetic research of complex diseases. J Transl Int Med 2015;3:137-43. [Crossref] [PubMed]
- Dincer HE, Gliksberg EP, Andrade RS. Endoscopic ultrasound and/or endobronchial ultrasound-guided needle biopsy of central intraparenchymal lung lesions not adjacent to airways or esophagus. Endosc Ultrasound 2015;4:40-3. [Crossref] [PubMed]
- Kheir F, Itani A, Assasa O, et al. The utility of endobronchial ultrasound-transbronchial needle aspiration in lymphoma. Endosc Ultrasound 2016;5:43-8. [Crossref] [PubMed]
- Hou G. Bronchoscopic lung volume reduction in chronic obstructive pulmonary disease: History and progress. J Transl Int Med 2015;3:147-50. [Crossref] [PubMed]
- Huo L, Moran CA, Fuller GN, et al. Pulmonary artery sarcoma: a clinicopathologic and immunohistochemical study of 12 cases. Am J Clin Pathol 2006;125:419-24. [Crossref] [PubMed]
- Shingyoji M, Ikebe D, Itakura M, et al. Pulmonary artery sarcoma diagnosed by endobronchial ultrasound-guided transbronchial needle aspiration. Ann Thorac Surg 2013;96:e33-5. [Crossref] [PubMed]
- Modi K, Dhillon S, Kumar A, et al. Leiomyosarcoma of the pulmonary artery diagnosed by endobronchial ultrasound-guided transbronchial needle aspiration. Endosc Ultrasound 2014;3:249-51. [Crossref] [PubMed]
- Kamaleshwaran KK, Pattabiraman V, Mehta S, et al. Spindle cell sarcoma of pulmonary artery mimicking thromboembolism with lung metastasis detected in fluorine-18 fluorodeoxyglucose positron emission tomography/computed tomography. Indian J Nucl Med 2014;29:249-51. [Crossref] [PubMed]
- Caraway NP, Salina D, Deavers MT, et al. Pulmonary artery intimal sarcoma diagnosed using endobronchial ultrasound-guided transbronchial needle aspiration. Cytojournal 2015;12:3. [Crossref] [PubMed]
- Horowitz JC, Kleaveland K, Arenberg D. Endobronchial biopsy of an intrapulmonary arterial mass. J Bronchology Interv Pulmonol 2013;20:93-5. [Crossref] [PubMed]
- Dusemund F, Schneider T, Zeisel C, et al. Endobronchial ultrasound-guided transbronchial needle aspiration of an intravascular sarcoma metastasis. Respiration 2013;86:430-2. [Crossref] [PubMed]
- Lee SJ, Lee J, Yu SJ, et al. Timely diagnosis of pulmonary artery tumor embolism by ultrasound-guided transbronchial needle aspiration. Thorac Cancer 2014;5:184-7. [Crossref] [PubMed]
- Al-Saffar F, Ibrahim S, Seeram V, et al. Use of endobronchial ultrasound to evaluate nonthrombotic endovascular lesions in pulmonary arteries: a systematic review. J Bronchology Interv Pulmonol 2015;22:28-32. [Crossref] [PubMed]
- Ye R, Zhao L, Wang C, et al. Clinical characteristics of septic pulmonary embolism in adults: a systematic review. Respir Med 2014;108:1-8. [Crossref] [PubMed]
- Schuuring MJ, Bonta PI, van Vugt M, et al. Endosonography of a Pulmonary Artery Obstruction in Echinococcosis. Respiration 2016;92:425-7. [Crossref] [PubMed]
- Raikou VD. Metabolic acidosis status and mortality in patients on the end stage of renal disease. J Transl Int Med 2016;4:170-7. [Crossref] [PubMed]
- Harris K, Maroun R, Attwood K, et al. Comparison of cytologic accuracy of endobronchial ultrasound transbronchial needle aspiration using needle suction versus no suction. Endosc Ultrasound 2015;4:115-9. [Crossref] [PubMed]
- Haas AR, Vachani A, Sterman DH. Advances in diagnostic bronchoscopy. Am J Respir Crit Care Med 2010;182:589-97. [Crossref] [PubMed]
- Kurimoto N, Inoue T, Miyazawa T, et al. The usefulness of endobronchial ultrasonography-guided transbronchial needle aspiration at the lobar, segmental, or subsegmental bronchus smaller than a convex-type bronchoscope. J Bronchology Interv Pulmonol 2014;21:6-13. [Crossref] [PubMed]
- Wang L, Mohan C. Contrast-enhanced ultrasound: A promising method for renal microvascular perfusion evaluation. J Transl Int Med 2016;4:104-8. [Crossref] [PubMed]


