Successful repair of neonatal tricuspid regurgitation due to chordae rupture
Introduction
Functional tricuspid regurgitation (TR) is transient and benign in stressed infants. In contrast, severe TR caused by a flail leaflet is a rare cause of neonatal cyanosis. The outcome may be fatal if not recognized early (1,2). We report on a full-term female neonate presented with cyanosis caused by severe TR due to anterior leaflet chordal rupture. After initial stabilization by prostaglandin E1 infusion for keeping ductal patency, successful early repair was achieved with polytetrafluoroethylene artificial chordae implantation. Early diagnosis and timely surgery can be lifesaving.
Case presentation
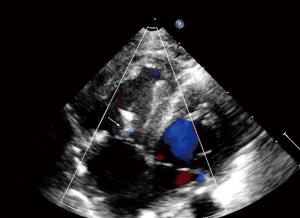
A 3,044-gm full term female was born by Cesarean section because of fetal distress and meconium stain. The first and fifth minutes Apgar score was 5 and 9. On physical examination, a grade III/VI pansystolic murmur was noted diffusely. She was cyanotic and the oxygen saturation was 85%. A two-dimensional echocardiography showed severe TR due to a flail and thickened anterior leaflet (Figure 1A,B) with the calculated tricuspid Z score of 1.28, and large patent ductus arteriosus. The antegrade pulmonary flow was compromised and a right-to-left shunt through the patent foramen ovale was noted. The hemodynamic characteristics were quite similar to that of the pulmonary atresia with intact ventricular septum.

At 6-day-old, cyanosis got worse due to impending ductal closure. She was intubated and prostaglandin E1 was infused (0.2 µg/kg/min), then the condition was stabilized and surgery was carried. Under mild hypothermia with cold crystalloid cardioplegic cardiac arrest, the patent ductus was ligated and the right atrium was opened. A flail tricuspid anterior leaflet due to extensive marginal chordae rupture was confirmed. The papillary muscle showed no ischemic change. The length of the septal leaflet chordae was measured as the reference and two loops of 6-0 expanded polytetrafluoroethylene artificial chordae were implanted over the unsupported margin of the anterior leaflet. A tricuspid annuloplasty was not necessary because the annulus was not dilated. The patent foramen ovale was not closed for pop-off purpose. Nitric oxide was not needed and under minimal inotrope support, the patient was recovered uneventfully. She was extubated 7 days after the operation and was discharged at 26th postoperative day. The two-dimensional echocardiography performed at 7-month-old showed competent tricuspid valve (Figure 2).
Discussion
Transient neonatal TR related to the perinatal hypoxia has been well known. In contrast, severe TR caused by rupture of papillary muscle or chordae in new born is rare and potentially fatal (1,2). The patient may be suffered from severe cyanosis and profound distress when associated with ductal closure because of the unique hemodynamic characteristics mimic to that of the pulmonary atresia with intact ventricular septum (3). When the ductus closed abruptly, extracorporeal membranous oxygenation support is necessary with subsequent emergent surgical intervention for life-saving (3-5). Alternatively, the ductus arteriosus can be maintained by timely prostaglandin E1 infusion to stabilize the baby.
Potential causes of chordae or papillary muscle rupture of tricuspid valve in the neonate include myocardial ischemia due to birth asphyxia, premature ductal closure, congenital endocarditis, maternal autoimmune disease, thromboembolism, traumatic rupture during birth process, or other obscure causes (4,5). In general, the anterior papillary muscle of the tricuspid valve is susceptible to the ischemia because of its high oxygen demand, diastolic coronary perfusion during high right ventricular pressure, and its distal extreme of the coronary circulation. In our patient, the history of perinatal distress and meconium staining was obvious. There was no autoimmune disease or relevant drug history during the late gestation period in the mother. Therefore, the most possible cause of tricuspid chordal rupture in our patient could be the temporary ischemia due to perinatal distress.
Although the desaturation can be temporarily improved by the prostaglandin E1 infusion, early repair of tricuspid valve is still mandatory. The reparative technique of polytetrafluoroethylene artificial chordae implantation in congenital tricuspid valve abnormalities has been reported with satisfactory short-term result in neonate. However, considering the lack of growth potential of the artificial material, careful evaluation of the long-term results is mandatory.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Witten informed consent was obtained from the patient for the writing of this manuscript.
References
- Alkalay AL, Ferry DA, Pepkowitz SH, et al. Critical tricuspid insufficiency due to papillary muscle rupture. A result of prenatal hypoxic insult. Am J Dis Child 1988;142:753-5. [Crossref] [PubMed]
- Benvenuti LA, Aiello VD, Cury AJ, et al. Post-ischemic rupture of the anterior papillary muscle of the right ventricle associated with persistent pulmonary hypertension of the newborn: a case report. Am J Cardiovasc Pathol 1992;4:79-84. [PubMed]
- Sachdeva R, Fiser RT, Morrow WR, et al. Ruptured tricuspid valve papillary muscle: a treatable cause of neonatal cyanosis. Ann Thorac Surg 2007;83:680-2. [Crossref] [PubMed]
- Anagnostopoulos PV, Alphonso N, Nölke L, et al. Neonatal mitral and tricuspid valve repair for in utero papillary muscle rupture. Ann Thorac Surg 2007;83:1458-62. [Crossref] [PubMed]
- Loftus PD, Arrington CB, Kaza AK. Neonatal flail tricuspid valve: diagnosis and management. Ann Thorac Surg 2014;98:1098-101. [Crossref] [PubMed]


