Intrepid steps towards clinical prime time
Mitral regurgitation (MR) is the most common valvular disorder and its prevalence is increasing in the aging population. MR is classically managed surgically or conservatively depending on its etiology and patient characteristics, however severe comorbidities preclude surgery in up to 50% of patients with severe MR (1). The development and widespread acceptance of transcatheter aortic valve replacement for patients with severe aortic stenosis over the past two decades has created a paradigm shift in the management of valvular heart disease. The mitral valve has quickly become the focus of emerging transcatheter technologies. However, challenges inherent to the mitral valve apparatus have made the development of transcatheter mitral valve replacement (TMVR) a more difficult endeavor (2).
The mitral valve apparatus is a complex structure comprising the mitral annulus, anterior and posterior mitral leaflets, and sub-valvular structures including the papillary muscles and tendinous chords. The mitral annulus is a dynamic, large, oval saddle-shaped structure. Its anterior edge is linear and formed by the stiff aortic-mitral curtain, whereas its posterior aspect is curved, predominantly muscular and prone to dilatation (3). The distinctive morphology of the mitral annular represents one of the most significant challenges for emerging transcatheter technologies. Other potential challenges include (I) lack of a calcified annulus to serve as a stabilizing landing zone for the prosthesis, (II) risk of left ventricular outflow tract (LVOT) obstruction due to encroachment of the device into the LVOT or displacement of the anterior mitral leaflet, (III) exposure of the prosthetic valve to high pressures which can impact valve stability and durability, and (IV) the high profile of current delivery systems (due to large valve prosthesis) which complicates access selection and device delivery (2,4).
Transcatheter mitral valve repair with the use of MitraClip (Abbott Vascular, Santa Clara, CA, USA) is an effective alternative for patients with primary MR who have a prohibitive surgical risk (5,6). Nevertheless, patients frequently require surgery to treat residual MR (7) and its role in secondary MR remains controversial despite apparent benefit from observational data (8). Multiple TMVR devices have been successfully implanted in humans and are currently undergoing early feasibility clinical trials (9,10). In this editorial, we refer to the initial experience of the Intrepid TMVR System (Medtronic, Minneapolis, MN, USA) published in the Journal of American College of Cardiology by Bapat et al. (11). The Intrepid TMVR System consists of a trileaflet bovine pericardial valve supported by a self-expanding nitinol frame with an outer fixation frame. Fixation is achieved through oversizing, conformation of the outer frame to the mitral annulus, and small cleats on the outer frame that engage the native mitral leaflets. The dual-frame structure allows the inner frame to remain independent of the shape and motion of the outer frame throughout the cardiac cycle. The system is delivered via transapical approach by using a 35-F access sheath.
In their study, Bapat et al. presented outcomes of 50 consecutive patients with symptomatic MR and a prohibitive surgical risk who underwent TMVR with the Intrepid TMVR System at 14 hospitals in Australia, Europe and the United States. Patients were mostly men (58%), with a mean age of 73±9 years, 84% had secondary MR, mean ejection fraction was 43.4±11.8, and mean STS score was 6.4±5.5. New York Heart Association (NYHA) functional class III or IV was common (86%) and 58% of patients had a heart failure hospitalization within the past year. Successful implantation occurred in 48 of 50 patients with one procedure aborted due to bleeding during apical access and one failure to implant device due to sizing miscalculation leading to device malposition. There were no instances of device malfunction or conversion to open surgery. Eight patients required hemodynamic support with intra-aortic balloon pump or extracorporeal membrane oxygenation. At 30 days, mortality was 14% (n=7), stroke was seen in 4%, major bleeding was present in 18%, and re-hospitalization for heart failure in 8% of cases. The seven early deaths were related to access site bleeding (n=3), device malposition (n=1), and refractory heart failure (n=3). Four additional patients died after 30 days due to sudden cardiac arrest (n=3) or intracranial hemorrhage (n=1). Absence of valve degeneration was documented among the four late deaths. In the 42 patients alive at 30 days, MR was absent or mild in all cases and there were no significant cases of LVOT obstruction or mitral stenosis. Mild para-prosthetic MR occurred in three patients and mild prosthetic MR in eight patients. There were no instances of hemolysis, device embolization, or thrombosis. Most patients had a NYHA functional class I or II at 30 days (79%).
Limitations of the study include the small number of patients who were able to undergo the procedure (only 50 out of 166 patients screened, primarily due to anatomical reasons) and the lack of long-term information on device durability and thromboembolic risk. Regardless of these limitations, the authors are to be congratulated for presenting the largest series of patients undergoing TMVR to date demonstrating the feasibility of the Intrepid TMVR system. The device was successfully implanted in most patients resulting in a significant reduction of MR and improvement of symptoms. Furthermore, there were no cases of LVOT obstruction, mitral stenosis, or device embolization, highlighting some of the properties of the valve and rigorous patient selection. The high rate of major bleeding and early deaths related to access site bleeding underscore the limitations of the transapical approach. The high rates of refractory heart failure could be potentially explained by two mechanisms. First, the use of transapical access is associated with myocardial injury and poor outcomes in patients undergoing transapical TAVR (12,13). This effect is likely amplified in patients undergoing TMVR who often have reduced systolic function and in which a higher system profile is used when compared to transapical TAVR (32- to 40- vs. 18-Fr) (9). Second, following TMVR the left ventricle is faced with a high-pressure system (aortic pressure) instead of the lower-pressure of the left atrium. This can lead to acute systolic dysfunction and a further drop in left ventricular ejection fraction in an already dysfunctional and remodeled left ventricle.
Other TMVR systems undergoing clinical investigation include the Tendyne (Tendyne Holdings LLC, Abbott Vascular, Roseville, MN, USA), CardiaAQ-Edwards (Edwards Lifesciences, Irvine, CA, USA), Tiara (Neovasc Inc., Richmond, B.C., Canada), Caisson (Caisson Interventional LLC, Maple Grove, MN, USA), and HighLife (HighLife SAS, Paris, France) systems. All have different features and potential advantages and disadvantages (Table 1) (4,9,10). Muller et al. published their experience with the first 30 patients undergoing TMVR with the Tendyne system (14). The valve was successfully implanted in 93% of patients with only one death at 30 days for a non-cardiac cause (hospital-acquired pneumonia). Residual MR was seen in only one patient (mild) and there was one case of valve thrombosis which resolved with anticoagulation. Early clinical experiences with all systems are currently underway. We suspect that particular features of each system will make them suitable for a specific subset of patients, thus providing the operator with more options to approach complex interventions.
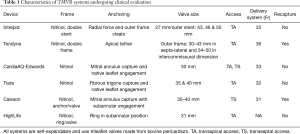
Full table
In summary, TMVR with the use of the Intrepid TMVR System proved to be technically feasible and associated with a reduction of MR and heart failure symptomatology in selected patients with symptomatic MR and a prohibitive surgical risk. Further experience in larger cohorts is needed to inform on device durability and long-term outcomes. Development of TMVR systems with lower profile and that can be safely delivered via the transseptal approach will presumably lead to lower procedural complications and thus represent the next step towards the clinical introduction of this technology.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mirabel M, Iung B, Baron G, et al. What are the characteristics of patients with severe, symptomatic, mitral regurgitation who are denied surgery? Eur Heart J 2007;28:1358-65. [Crossref] [PubMed]
- Patel A, Bapat V. Transcatheter mitral valve replacement: device landscape and early results. EuroIntervention 2017;13:AA31-9. [Crossref] [PubMed]
- Hoffman J, Fullerton D. Surgical anatomy of the aortic and mitral valves. In: Iribarne A, Stefanescu A, Nguyen TC. Transcatheter Heart Valve Handbook: A Surgeons’ and Interventional Council Review. Washington, DC: American College of Cardiology, 2018.
- Regueiro A, Granada JF, Dagenais F, et al. Transcatheter Mitral Valve Replacement: Insights From Early Clinical Experience and Future Challenges. J Am Coll Cardiol 2017;69:2175-92. [Crossref] [PubMed]
- Feldman T, Foster E, Glower DD, et al. Percutaneous repair or surgery for mitral regurgitation. N Engl J Med 2011;364:1395-406. Erratum in: N Engl J Med 2011;365:189. [Crossref] [PubMed]
- Nishimura RA, Otto CM, Bonow RO, et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014;63:e57-185. Erratum in: J Am Coll Cardiol 2014;63:2489. [Crossref] [PubMed]
- Mauri L, Foster E, Glower DD, et al. 4-year results of a randomized controlled trial of percutaneous repair versus surgery for mitral regurgitation. J Am Coll Cardiol 2013;62:317-28. [Crossref] [PubMed]
- Mendirichaga R, Singh V, Blumer V, et al. Transcatheter Mitral Valve Repair With MitraClip for Symptomatic Functional Mitral Valve Regurgitation. Am J Cardiol 2017;120:708-15. [Crossref] [PubMed]
- Zaid S, Tang G, El-Eshmawi A. Future Transcatheter Mitral Valve Repair/Replacement Technologies. In: Iribarne A, Stefanescu A, Nguyen TC. Transcatheter Heart Valve Handbook: A Surgeons’ and Interventional Council Review. Washington, DC: American College of Cardiology, 2018.
- Guerrero ME, Salinger MH, Levisay JP, et al. Transcatheter Mitral Valve Replacement Therapies. American College of Cardiology Expert Analysis 2017. Available online: http://www.acc.org/latest-in-cardiology/articles/2017/04/28/09/32/transcatheter-mitral-valve-replacement-therapies
- Bapat V, Rajagopal V, Meduri C, et al. Early Experience With New Transcatheter Mitral Valve Replacement. J Am Coll Cardiol 2018;71:12-21. [Crossref] [PubMed]
- Ribeiro HB, Nombela-Franco L, Muñoz-García AJ, et al. Predictors and impact of myocardial injury after transcatheter aortic valve replacement: a multicenter registry. J Am Coll Cardiol 2015;66:2075-88. [Crossref] [PubMed]
- Urena M, Webb JG, Eltchaninoff H, et al. Late cardiac death in patients undergoing transcatheter aortic valve replacement: incidence and predictors of advanced heart failure and sudden cardiac death. J Am Coll Cardiol 2015;65:437-48. [Crossref] [PubMed]
- Muller DWM, Farivar RS, Jansz P, et al. Transcatheter Mitral Valve Replacement for Patients With Symptomatic Mitral Regurgitation: A Global Feasibility Trial. J Am Coll Cardiol 2017;69:381-91. [Crossref] [PubMed]


