The intrepid adventure of early transcatheter mitral valve replacement
Thirty years ago, Andersen et al. first described the replacement of a native valve with a bioprosthetic valve mounted on a stent and delivered via a catheter (1). Since then, the field of transcatheter valve replacement has witnessed an unprecedented evolution, with transcatheter aortic valve replacement (TAVR) now occupying center stage in contemporary treatment of severe aortic stenosis (2). Inspired by this enormous triumph, and the unmet needs in the management of severe mitral regurgitation (MR), a soaring number of transcatheter mitral valve replacement (TMVR) systems have been developed in the last few years (3). However, only a handful of those have reached early feasibility study (EFS) investigational stages in humans (3). Recently, Bapat et al. laudably reported the first experience with the Intrepid valve (Medtronic Inc., Redwood City, CA, USA) that illustrated several unresolved challenging in the field of TMVR (4).
The Intrepid valve is a self-expanding, nitinol dual frame valve that is delivered via a 35-French transapical sheath (Figure 1). The valve is composed of an outer stent frame (also called the fixation frame) that has a flexible atrial portion, allowing conformability with the native mitral annulus, and a stiffer ventricular portion that is wider than the native annulus. The outer frame is available in three sizes (43, 46, 50 mm) that is accompanied by cleats designed to engage the native mitral leaflets and a flexible atrial brim to facilitate visualization with echocardiography. Finally, the inner stent frame houses a one-size 27 mm tri-leaflet bovine pericardium valve. Compared with other emerging TMVR systems, the Intrepid valve has three distinguishing features: (I) the unique design of the outer frame allows ‘wedging’ of the valve in the sub-annular mitral space and minimizes the risk of embolization; (II) the conformable symmetric design eliminates the need for rotational orientation, greatly simplifying valve deployment; (III) the valve profile (height) is reduced to <18 mm to mitigate the risk of left ventricular outflow (LVOT) obstruction.

The Intrepid TMVR pilot study enrolled 50 high-risk patients (Society of Thoracic Surgery predicted risk of mortality 6.4%±5.5%) with severe symptomatic MR. Key exclusion criteria included left ventricular ejection fraction <20%, severe mitral annular calcification, severe pulmonary hypertension, severe renal insufficiency, and prior mitral valve surgery or intervention. The mean age of the study patients was 73±9 years and 58% were men. The etiology of MR was secondary in 80% and primary in 20%, and 22 patients (44%) had moderate or severe tricuspid regurgitation. Procedural results were good: device implantation was successful in 48 patients (96%). Among these patients, there was no device embolization, conversion to open surgery, moderate to severe MR, or LVOT obstruction. However, there was a 16% concerning rate for peri-operative hemodynamic support need, and 6% rate of apical bleeding leading to death.
The 30-day operative mortality rate was 14% (n=7); 3 related to apical access bleeding, 1 due to valve malpositioning, and 3 as a result of refractory heart failure. In the surviving patients with implanted valves at 30 days (n=42 patients), valve performance remained excellent with no evidence of mitral stenosis, LVOT obstruction, or significant MR in any patients. This was accompanied complete resolution of symptoms reported in 33 patients (79%), and overall significant improvements in Minnesota Living with Heart Failure Questionnaire scores (56.2±26.8 vs. 31.7±22.1; P=0.011). Nonetheless, 6-minute walk distance did not significantly change (248.3±103.6 vs. 267.6±110.0 meters; P=0.31). At a median follow up of 173 days, total mortality has increased to 11 patients (22%). The 4 additional deaths beyond 30 days were a result of sudden cardiac arrest in 3 patients and intracranial hemorrhage in 1. A summary of the safety events in this trial compared with the largest reported TMVR trial to date (Tendyne early feasibility trial, Abbott, Roseville, MN, USA) is provided in Table 1 (4,6).
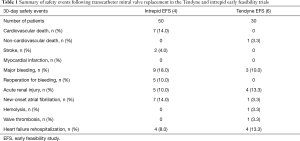
Full table
The principle findings of this pilot investigation were: (I) Intrepid TMVR was successfully achieved in 96% of patients with reduction in MR to mild or none in all; (II) no device malfunction or structural valve degeneration occurred acutely or during mid-term follow-up; (III) patients who survived the procedure had significant improvement in heart failure symptoms; (IV) certain procedural complications (e.g., access site bleeding) occurred at an unexpected high-rate; and (V) 30-day mortality was two-fold higher than predicted for surgical mitral valve replacement in this high-risk cohort.
This blend of promising and concerning findings is intriguing and merit more scrutiny based on the following:
- The high implant success rate and the excellent valve performance support an added value of the unique features of the Intrepid valve. The low valve profile and case selection navigated LVOT obstruction in all cases [although a strict eligibility criterion for neo-LVOT (>1.3 cm2) was applied in this study]. The conformable outer frame design allowed quick deployment (median device deployment time was 14 minutes) with no incidence of device embolization and only one incident of valve malposition. Nevertheless, the high access related bleeding rate highlights a potential deficiency of the current valve design. Contrary to the Tendyne TMVR system in which apical hemostasis is seamlessly achieved with a built in apical pad, the Twelve Intrepid valve has no specific mechanism for secure apical access closure. In the Tendyne EFS trial, no patients died or needed reoperation due to access site bleeding despite the comparable required sheath size (34 French);
- The early post-operative mortality was higher-than-expected, but most concerning was the high occurrence of non-procedural cardiovascular deaths (three patients died within 30 days due to worsening heart failure, and three died between 2–4 months due to sudden cardiac arrest). These deaths may be due to high-risk clinical profiles of the study patients, but other plausible causes need to be considered to optimize patient selection in future TMVR trials. One potential explanation is the intolerance of apical access-associated myocardial injury in patients with severely reduced left ventricular function, especially those with decompensated heart failure (16% of patients required peri-operative hemodynamic support with intra-aortic balloon pumps or extracorporeal oxygenation). Since the majority of TMVR systems are currently designed to be delivered via transapical access, further studies are needed to investigate potential negative impact of this access rout in patients with advanced cardiomyopathy;
- The valve maintained an excellent performance at mid-term follow-up, and showed no evidence of valve thrombosis or structural deterioration. However, similar to what was observed in the Tendyne EFS, a modest decrement in left ventricular ejection fraction was noted (43.3%±11.8% to 37.1%±11.4%). The clinical significance of this finding is yet to be determined;
- An apparent symptomatic improvement in surviving patients was observed with subjective parameters (Minnesota Living with Heart Failure Questionnaire score and New-York Heart Association class), but objective measures (e.g., 6-minute walk distance) did not demonstrate a similar improvement. This may be related to the inclusion of very high-risk or frail patients in this trial, and the lack of long-term follow-up data. Yet these findings do illustrate the potential utility of TMVR in producing meaningful symptom amelioration in patients with severe MR.
This study provides a pioneering snapshot of information that confirm the feasibility of TMVR as a treatment for severe symptomatic MR while highlighted the significant remaining challenges in the TMVR field at large. Nonetheless, the provocative findings of this pilot study will certainly inform further innovation in transcatheter mitral valve modeling and refinement, and aid clinicians in their search for the optimal candidates of TMVR.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Andersen HR, Knudsen LL, Hasenkam JM. Transluminal implantation of artificial heart valves. Description of a new expandable aortic valve and initial results with implantation by catheter technique in closed chest pigs. Eur Heart J 1992;13:704-8. [Crossref] [PubMed]
- Vahl TP, Kodali SK, Leon MB. Transcatheter Aortic Valve Replacement 2016: A Modern-Day "Through the Looking-Glass" Adventure. J Am Coll Cardiol 2016;67:1472-87. [Crossref] [PubMed]
- Alkhouli M, Alqahtani F, Aljohani S. Transcatheter mitral valve replacement: an evolution of a revolution. J Thorac Dis 2017;9:S668-72. [Crossref] [PubMed]
- Bapat V, Rajagopal V, Meduri C, et al. Early Experience with New Transcatheter Mitral Valve Replacement. J Am Coll Cardiol 2018;71:12-21. [Crossref] [PubMed]
- Meredith I, Bapat V, Morriss J, et al. Intrepid transcatheter mitral valve replacement system: technical and product description. EuroIntervention 2016;12:Y78-80. [Crossref] [PubMed]
- Muller DWM, Farivar RS, Jansz P, et al. Transcatheter Mitral Valve Replacement for Patients With Symptomatic Mitral Regurgitation: A Global Feasibility Trial. J Am Coll Cardiol 2017;69:381-91. [Crossref] [PubMed]


