Improved lymph node staging in early-stage lung cancer in the national cancer database: commentary
Commentary
Historical notes
In 1960, Cahan (1) was the first author to report 48 patients with lung cancer who successfully underwent lobectomy with regional lymph node (LN) dissection, termed as “radical lobectomy.” After over half-a-century later, this procedure still remains a universally accepted standard surgical strategy for lung cancer. Over the years, several pathological and/or biological markers have been evaluated according to their status and role in detecting patients with a high risk on poor prognosis of lung cancer. However, the primary tumor, LN, and metastasis (TNM) staging remains the critical determining system of outcomes. Thus, accurate LN assessment is crucial in determining a treatment strategy because the prognosis of lung cancer is directly proportional to the present status of LN metastasis.
The status of regional LNs is a critical factor for staging, therapeutical management, and assessing treatment efficacy in patients with lung cancer. In 1978, Naruke et al. (2) were the first to propose an anatomical map that encompassed the number of LN stations, which had been universally used for radiological LN assessment and surgical dissection. Mountain and Dresler (3), in 1997 introduced a novel classification for LN map, “MD-ATS map,” for the staging system of lung cancer, which was adopted by the American Joint Committee on Cancer and the Union Internationale Contre le Cancer. The MD-ATS map intended to unify into a single system the characteristics of the LN station proposed by Naruke and the schema developed in 1983 by the American Thoracic Society (ATS) and the North American Lung Cancer Study Group, which was preferred by both the ATS and the European Respiratory Society (4,5). Regional nodal dissection or sampling, including that in the superior and inferior mediastinum, has been widely performed in lung cancer surgery using these maps. However, the analyses of lung cancer treatment outcomes have been hindered by nomenclature discrepancies in different maps used by the Asian and Western countries. Recently, the International Association for the Study of Lung Cancer (IASLC) conducted a Lung Cancer Staging Project, which led to the development of an international lung cancer database. In addition, the IASLC proposed a new LN map, which considered differences among the several maps currently used and provided precise anatomic definitions for all LN stations, to attain uniformity and promote future assessment of a prospective international database (6).
Potential survival benefit of adequate nodal assessment
Research has established that proper nodal evaluation is the central tenet of quality surgical procedures for non-small cell lung cancer (NSCLC) and correlates with improved survival. Gajra et al. (7), Doddoli et al. (8), and Massard et al. (9) suggested that for accurate staging of lung cancer, systematic nodal dissection is superior to tissue sampling. In contrast, Keller et al. (10) and Gajra et al. (7) reported that the efficacy of both systematic sampling and systematic nodal dissection is analogous for accurate staging. However, the survival benefit of LN dissection has not been statistically confirmed for patients with lung cancer because LN dissection and sampling have been compared by only a few prospective randomized controlled trials (RCTs). To date, four RCTs have examined the survival assessment of LN dissection with sampling (Table 1). Thus, further systematic reviews and meta-analyses are required to resolve these differences and obtain accurate assessment providing stronger rationales. Takagi et al. (11) and Huang et al. (12) conducted a meta-analysis of pooled data from four existent RCTs and demonstrated a statistically non-significant reduction (but a relative trend toward a significant reduction) in all-cause mortality with mediastinal LN dissection relative to sampling in fixed-effects models (HR =0.86; 95% CI, 0.73–1.01; P=0.06; and HR =0.77; 95% CI, 0.55–1.08; P=0.13, respectively). These meta-analyses suggest that mediastinal LN dissection might not improve the long-term survival oversampling during lung surgery in patients with early-stage NSCLC. However, the American College of Surgery Oncology Group (ACOSOG) Z0030 trial (13) reported that 4% of patients demonstrated LN metastases after systematic nodal dissection, which were not detected by meticulous, systematic sampling. Since systematic nodal dissection can reveal “unexpected” N2 disease irrespective of the historical type, tumor size, location, and lobe of existing primary tumor, LN dissection remains a crucial investigative procedure in all patients who underwent surgical resection for lung cancer. Although guidelines detailing adequate resection vary considerably, appropriate LN assessment is a hallmark of quality curative intent operations for NSCLC.
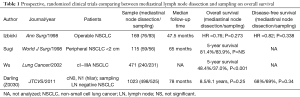
Full table
Current guidelines for adequate nodal assessment
The present National Comprehensive Cancer Network guidelines recommend sampling of at least three N2 stations or a complete mediastinal dissection. While, the CoC recommends that at least 10 LNs should be removed and pathologically reviewed, the European Society of Thoracic Surgeons suggests a complete mediastinal dissection of all LN stations with additional guidelines on the pathological dissection of specimens. However, these guidelines are poorly adhered to and do not necessarily reflect applicability in broader clinical practice (14). Recently, as aforementioned, a notable increase has been detected in the number of LNs assessed for clinical stage I lung cancer, and these developments have been observed across all hospital types, possibly because the impact of the z0030 trial might have been large enough to emphasize the importance of nodal assessment more broadly. Remarkably, variables, including increasing year, age >65 years, male sex, non-African American race, academic centers, lobectomy, and clinical T2 disease, have been shown to correlate with >15 nodes that were assessed. Furthermore, Yue et al. reported that increased adherence to these guidelines was associated with improved survival (15).
Specific number of nodes removed and survival outcome
At present, extensive cohort studies have focused on the effect of specific number of resected LNs on survival outcomes (16-19) because the prominence of proper staging might have an even higher impact with increasingly effective adjuvant therapy. Apparently, a higher removal of nodes is related to more precise staging, which eventually improves the overall and cancer-specific survival. As addressed by authors in this article, when comparing groups based on 14 nodes, patients with >14 nodes assessed demonstrated better survival in both upstaged and non-upstaged cohorts. However, the effect of specific number of nodes removed on survival outcome remains controversial. Thus, further extensive, prospective clinical studies are needed for lymph nodal assessment. Recently, a randomized phase III trial of lobe-specific versus systematic nodal dissection for clinical stage I–II NSCLC (JCOG1413) is being conducted, which has been enrolling patients since 2017 (20); while the primary endpoint of the trial is the overall survival, the primary objective is to validate the non-inferiority of lobe-specific systematic nodal dissection based on lobectomy. In addition, the trial intends to enroll approximately 1,700 patients from 44 Japanese institutions within the next 5 years. Perhaps, this comprehensive and quality data will provide useful information on the specific number of nodes that should be removed to improve the survival outcome.
Acknowledgements
Medical English writing assistance was provided by Crimson Interactive Pvt. Ltd. The authors are fully responsible for the content and editorial decisions for this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cahan WG. Radical lobectomy. J Thorac Cardiovasc Surg 1960;39:555-72. [PubMed]
- Naruke T, Suemasu K, Ishikawa S. Lymph node mapping and curability at various levels of metastasis in resected lung cancer. J Thorac Cardiovasc Surg 1978;76:832-9. [PubMed]
- Mountain CF, Dresler CM. Regional lymph node classification for lung cancer staging. Chest 1997;111:1718-23. [Crossref] [PubMed]
- American Thoracic Society. Medical section of the American Lung Association. Clinical staging of primary lung cancer. Am Rev Respir Dis 1983;127:659-64. [Crossref] [PubMed]
- Pretreatment evaluation of non-small-cell lung cancer. The American Thoracic Society and The European Respiratory Society. Am J Respir Crit Care Med 1997;156:320-32. [Crossref] [PubMed]
- Rusch VW, Asamura H, Watanabe H, et al. The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009;4:568-77.
- Gajra A, Newman N, Gamble GP, et al. Effect of number of lymph nodes sampled on outcome in patients with stage I non-small-cell lung cancer. J Clin Oncol 2003;21:1029-34. [Crossref] [PubMed]
- Doddoli C, Aragon A, Barlesi F, et al. Does the extent of lymph node dissection influence outcome in patients with stage I non-small-cell lung cancer? Eur J Cardiothorac Surg 2005;27:680-5. [Crossref] [PubMed]
- Massard G, Ducrocq X, Kochetkova EA, et al. Sampling or node dissection for intraoperative staging of lung cancer: a multicentric cross-sectional study. Eur J Cardiothorac Surg 2006;30:164-7. [Crossref] [PubMed]
- Keller SM, Adak S, Wagner H, et al. Mediastinal lymph node dissection improves survival in patients with stages II and IIIa non-small cell lung cancer. Eastern Cooperative Oncology Group. Ann Thorac Surg 2000;70:358-65; discussion 65-6. [Crossref] [PubMed]
- Takagi H, Matsui M, Umemoto T. Alice in wonderland of mediastinal lymph nodes. J Thorac Cardiovasc Surg 2011;142:477-8; author reply 8-9. [Crossref] [PubMed]
- Huang X, Wang J, Chen Q, et al. Mediastinal lymph node dissection versus mediastinal lymph node sampling for early stage non-small cell lung cancer: a systematic review and meta-analysis. PLoS One 2014;9:e109979. [Crossref] [PubMed]
- Darling GE, Allen MS, Decker PA, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg 2011;141:662-70. [Crossref] [PubMed]
- Allen JW, Farooq A, O'Brien TF, et al. Quality of surgical resection for nonsmall cell lung cancer in a US metropolitan area. Cancer 2011;117:134-42. [Crossref] [PubMed]
- Yue D, Gong L, You J, et al. Survival analysis of patients with non-small cell lung cancer who underwent surgical resection following 4 lung cancer resection guidelines. BMC Cancer 2014;14:422. [Crossref] [PubMed]
- Ludwig MS, Goodman M, Miller DL, et al. Postoperative survival and the number of lymph nodes sampled during resection of node-negative non-small cell lung cancer. Chest 2005;128:1545-50. [Crossref] [PubMed]
- Ou SH, Zell JA. Prognostic significance of the number of lymph nodes removed at lobectomy in stage IA non-small cell lung cancer. J Thorac Oncol 2008;3:880-6. [Crossref] [PubMed]
- Saji H, Tsuboi M, Yoshida K, et al. Prognostic impact of number of resected and involved lymph nodes at complete resection on survival in non-small cell lung cancer. J Thorac Oncol 2011;6:1865-71. [Crossref] [PubMed]
- Osarogiagbon RU, Yu X. Mediastinal lymph node examination and survival in resected early-stage non-small-cell lung cancer in the surveillance, epidemiology, and end results database. J Thorac Oncol 2012;7:1798-806. [Crossref] [PubMed]
- Hishida T, Saji H, Watanabe SI, et al. A randomized Phase III trial of lobe-specific vs. systematic nodal dissection for clinical Stage I-II non-small cell lung cancer (JCOG1413). Jpn J Clin Oncol 2018;48:190-4. [Crossref] [PubMed]


