Correlation of triglycerides with myocardial infarction and analysis of risk factors for myocardial infarction in patients with elevated triglyceride
Introduction
Cardiovascular disease (CVD) is the leading cause of death worldwide, which has become a worldwide public health problem (1,2). Acute myocardial infarction (AMI) is a common clinical critical illness. In the past few decades, significant progress has been made in understanding, preventing and controlling this disease. In particular, the rise of reperfusion therapy significantly reduced mortality and improved the prognosis of AMI (3-6). In recent years, the role of low density lipoprotein density (LDL-C) in the pathogenesis of atherosclerosis (AS) has attracted much attention (7). However, more and more clinical trials have revealed that after controlling for deterministic risk factors such as LDL-C, the risk for coronary heart disease (CHD) remained, while the increase in triglycerides (TG) was significantly correlated with the increase in mortality, the incidence of myocardial infarction (MI) and the recurrence rate of coronary artery disease (8,9). Furthermore, elevated plasma TG level is an independent risk factor for CHD and AS (10-14). In the present study, the prevalence and risk factors of MI and its correlation with fasting plasma TG were investigated to provide basis for the effective prevention and treatment of MI.
Methods
Subjects
This research cohort study comprised of in-service and retired employees of the Kailuan Coal Mine Group, who participated in the health examination conducted in 11 hospitals in the Kailuan region from June 2006 to October 2007. A total of 100,271 employees were included into the study. Subjects without relevant data, or those who had a history of MI or stroke prior to enrollment were excluded. This research was reviewed and approved by the Ethics Committee of the Kailuan Medical Group (No. 2016-Sci.-101). The study population was divided into five groups, according to different TG levels: TG1 group, 0.01–0.81 mmol/L; TG2 group, 0.82–1.19 mmol/L; TG3 group, 1.20–1.46 mmol/L; TG4 group, 1.47–2.16 mmol/L; TG5 group, 2.17–19.95 mmol/L.
Survey method
Research questionnaire
Unified operating rules were first established. The questionnaire was sent to the employees, and was individually filled. Then, all questionnaire contents were verified item by item and face-to-face by a medical staff who received a unified training. The questionnaire included personal habits (including drinking, smoking, exercise, sleep time and quality) and related disease history (including hypertension, diabetes, MI, and hypertension family history), educational level, and economic income. The physical examinations were carried out by trained medical staff. On the day of the physical examination, fasting TG and other biochemical indexes were detected.
Physical examinations
Height and weight were measured using a calibrated mass balance (RGZ-120). The participants were asked to take off their hat and shoes, and wear light clothing. Height accuracy was set to 0.1 cm, and weight accuracy was set to 0.1 kg. Blood pressure was measured on the right brachial artery using a calibrated mercury sphygmomanometer. The subjects were prohibited from smoking or drinking tea or coffee within 30 minutes before the blood pressure measurement, and were instructed to seat quietly back against something for more than 15 minutes. The reading of systolic blood pressure (SBP) used the first phase of the Korotkoff sound, and diastolic blood pressure (DBP) used the fifth phase of the Korotkoff sound. Blood pressure was continuously measured three times, measurement interval was set at 1–2 minutes, and the average value was calculated.
Biochemical index detection
Subjects were given at least 8 hours of fasting, and approximately 5 mL of elbow vein blood was withdrawn on the morning of the same day. Blood was centrifuged, and the upper part of the serum was obtained for the detection of fasting blood glucose (FBG), TG, total cholesterol (TC), high density lipoprotein cholesterol (HDL-C), LDL-C, uric acid (UA), creatinine (Cr) and other biochemical indicators. The upper serum was transferred into vacuum tubes containing ethylenediaminetetraacetic acid (EDTA). All blood samples were processed and analyzed using an auto-analyzer (Hitachi747; Hitachi, Tokyo, Japan) at the central laboratory of Kailuan General Hospital. TC level in serum was measured using the endpoint test method. HDL-C and LDL-C were measured using the direct test method. TG was measured using the GPO method (inter-assay coefficient of variation <10%; Mind Bioengineering Co. Ltd., Shanghai, China). Non-HDL-C level was determined by subtracting serum HDL-C from serum TC.
Follow-ups
Data on the new MI were collected every 6 months. The completion points of the health examination conducted between June 2006 and October 2007 was defined as the starting point of the follow-ups, while the endpoint events included MI and all-cause death. If endpoint events occurred, it was recorded as a total endpoint event, and the time and event of the first event was defined as the outcome. The endpoint events of the subjects were recorded by trained medical personnel in the hospital where the health examination was carried out. Medical records from 2010, which were filed in other medical units out of the health examination hospital, were collected by the Medical Insurance Center of Kailuan City once every 6 months, and the relevant hospitalization data of subjects who suffered from endpoint events were especially collected. All diagnoses were verified by professional doctors according to hospital admission records.
Relevant definitions and diagnostic criteria
Smoking: taking at least one cigarette a day for more than a year. The diagnosis of hypertension was based on the Guidelines of Prevention and Treatment of Hypertension in China (15) (SBP ≥140 mmHg and/or DBP ≥90 mmHg). The diagnosis of AMI was based on the diagnostic criteria developed by the Chinese Society of Cardiovascular Diseases of Chinese Medical Association (16). Exercise frequency: more than three times a week for at least 30 minutes each time was considered regular exercise. Otherwise, it was considered as less exercise.
Statistical analysis
Data were collected using the software Epidata 3.0 and analyzed using statistical software SPSS 18.0. Measurement data were expressed as mean ± standard deviation (SD). Intergroup comparison was conducted using analysis of variance. Count data were evaluated using χ2-test. Logistic regression analysis was used to analyze risk factors for MI in patients with elevated TG, and Cox proportional hazards regression analysis was used to analyze the effects of different TG levels on the endpoint events. P<0.05 (two-tailed test) was considered statistically significant.
Results
Comparison of the general conditions, biochemical indexes and outcomes of subjects with different TG levels
In the study population of the Kailuan region, the proportion of male subjects was higher in groups with high TG levels, while the difference in age was not statistically significant. With the increase in TG level, the proportion of people with a history of smoking increased, body mass index (BMI), SBP, DBP, FBG, UA and the rate of MI increased, while HDL-C level gradually decreased, and the differences were all statistically significant. Differences in TC and LDL-C levels were not statistically significant (Table 1).
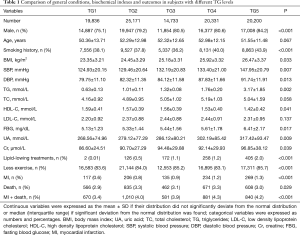
Full table
Multivariate logistic regression analysis results
The multivariate logistic regression analysis revealed that in a population with elevated TG, an age of ≥65 years old, BMI >25 kg/m2, FBG ≥6.1 mmol/L and HDL-C <1.5 mmol/L were risk factors for MI (Table 2).
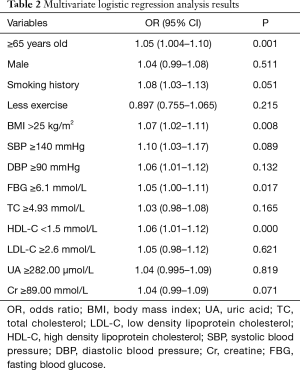
Full table
Effect of the Cox proportional hazards regression model on different endpoint events
After controlling for age, gender, BMI, UA, SBP, DBP, creatine (Cr), FBG, lipid-lowing treatments, smoking history, as the TG level increased, the relative risk of MI also increased. Compared to the TG1 group, the risk of MI increased to 1.32 folds in the TG4 group (95% CI: 1.05–1.66, P=0.018) and 1.61 folds in the TG5 group (95% CI: 1.21–1.93, P=0.004). In addition, the risks of MI combined with all-cause death and all-cause death also increased, but the differences were all not statistically significant (Table 3).
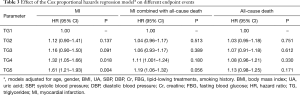
Full table
Discussion
With the changes in diet structures, the incidence of dyslipidemia continuously increases. Dyslipidemia, inflammation and immune reaction induced by abnormal lipid metabolism are the basis of the occurrence and development of CHD. A foreign study revealed that for patients with a TG level ≥1.13 mmol/L, the risk of major cardiovascular events significantly increased (17). As a predictor of cardiovascular events, TG has its instability, and it remains to be proven whether TG is its independent risk factor by a large number of studies (10-14). In addition, the results of a study revealed that plasma TG and HDL-C have a synergistic effect on the occurrence of CHD. When plasma LDL-C concentration was <3.36 mmol/L, the risk of CHD was 10 times as high in a population with high TG (>2.98 mmol/L) and low HDL-C (<0.67 mmol/L), compared with a population with low TG (<0.67 mmol/L) and high HDL-C (>1.66 mmol/L). This study revealed that with the increase in TG level, the rate of MI increased, the level of HDL-C gradually decreased, and the relative risk of MI also increased with the increase in TG level. Compared to the TG1 group, the risk of MI increased to 1.32 folds in the TG4 group and 1.61 folds in the TG5 group. This suggests that high TG level is a risk factor for MI, and the higher the TG level is, the greater the risk of MI.
Although a study revealed that the onset age of AMI has become younger, the increase in TG and low-density lipoprotein was very often in young patients with AMI (18). The results of this study suggested that an age of ≥65 years was a risk factor for MI in a population with elevated TG, while the effect of gender was not statistically significant. The reason may be that the research population of this study was mainly male and comprised of northern occupational subjects.
A previous study revealed that the incidence of CVD in an obese population was significantly higher than that in a normal population, and obesity was a risk factor for cardiovascular events, which increased the risk of death induced by CVD (19). Another study revealed that in patients with chronic diseases, the prognosis of patients with obesity and overweight may be better, compared to patients with normal BMI. That is, BMI was negatively correlated with cardiovascular prognosis (20). This suggests that the relationship between BMI and cardiovascular events remains controversial. This study revealed that BMI >25 was a risk factor for MI in a population with elevated TG. This suggests that BMI remains to be associated with the occurrence of MI to a certain extent. Hypertension is one of the risk factors of AMI, which plays a certain role in the occurrence, development and prognosis of MI (21). The mechanism may be that hypertension increases coronary perfusion pressure in patients, and increases vessel wall tension, leading to vascular intimal injury and blood lipid deposits in the vascular endothelium, which makes the vascular lumen gradually become narrow or even occluded, inducing MI (22). In this study, SBP ≥140 mmHg and HBD ≥90 mmHg tended to be risk factors for MI in a population with elevated TG. This suggests that hypertension appear to be closely correlated to the occurrence of MI.
Abnormal glucose metabolism is a common risk factor for MI, and has an important influence on its prognosis (23). In this study, with the increase in TG level, fasting blood glucose level increased, and FBG ≥6.1 mmol/L was a risk factor for MI in a population with elevated TG. This suggests that hyperglycemia is correlated to the occurrence of MI. In recent years, a number of studies have suggested that serum UA is closely correlated to CVD, and is one of the independent risk factors for CVD (24,25). In this study, with the increase in TG level, UA level also increased, but it was not a risk factor for MI in a population with elevated TG. Hence, enough attention should be continuously provided to this, and measures should be taken to reduce the UA level under the control of other risk factors.
Conclusions
In summary, high TG levels have a serious impact on human life and health. It is a risk factor for MI. Therefore, more attention should be given to the control and management of blood lipid levels, in order to reduce the incidence of adverse cardiovascular events.
Acknowledgements
We are particularly grateful to all the people who have given us help on our article.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This research was reviewed and approved by the Ethics Committee of the Kailuan Medical Group (No. 2016-Sci.-101).
References
- Pagidipati NJ, Gaziano TA. Estimating deaths from cardiovascular disease: a review of global methodologies of mortality measurement. Circulation 2013;127:749-56. [Crossref] [PubMed]
- Lishu C, Yan J, Xianbin D, et al. Analysis on death trend of stroke and myocardial infarction in Chongqing during 2006-2010. Chongqing Med 2014;43:317-21.
- O'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/ American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:e78-140. [Crossref] [PubMed]
- Wallace EL, Abdel-Latif A, Charnig R, et al. Meta-analysis of long-term outcomes for drug-eluting stents versus bare-metal stents in primary percutaneous coronary interventions for ST-segment elevation myocardial infarction. Am J Cardiol 2012;109:932-40. [Crossref] [PubMed]
- Wan F, Zhang T, Shen L, et al. Early routine post-thrombolysis percutaneous coronary intervention vs. primary PCI in ST-segment elevated myocardial infarction: a comparative study. Chin J Inter Cardiol 2013;21:3-7.
- Czarnecki A, Welsh RC, Yan RT, et al. Reperfusion strategies and outcomes of ST-segment elevation myocardial infarction patients in Canada: observations from the Global Registry of Acute Coronary Events (GRACE) and the Canadian Registry of Acute Coronary Events (CANRACE). Can J Cardiol 2012;28:40-7. [Crossref] [PubMed]
- Ridker PM. LDL Cholesterol: controversies and future therapeutic directions. Lancet 2014;384:607-17. [Crossref] [PubMed]
- Chapman MJ, Ginsberg HN, Amarenco P, et al. Triglyceriderich lipoproteins and high-density lipoprotein cholesterol in patients at high risk of cardiovascular disease: evidence and guidance for management. Eur Heart J 2011;32:1345-61. [Crossref] [PubMed]
- Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet 2014;384:626-35. [Crossref] [PubMed]
- Tenenbaum A, Klempfner R, Fisman EZ. Hypertriglyceridemia: a too long unfairly neglected major cardiovascular risk factor. Cardiovasc Diabetol 2014;13:159. [Crossref] [PubMed]
- Kolovou GD, Mikhailidis DP, Kovar J, et al. Assessment and clinical relevance of non-fasting and postprandial triglycerides: an expert panel statement. Curr Vasc Pharmacol 2011;9:258-70. [Crossref] [PubMed]
- Matsumoto S, Gotoh N, Hishinuma S, et al. The role of hypertriglyceridemia in the development of atherosclerosis and endothelial dysfunction. Nutrients 2014;6:1236-50. [Crossref] [PubMed]
- Borén J, Matikainen N, Adiels M, et al. Postprandial hypertriglyceridemia as a coronary risk factor. Clin Chim Acta 2014;431:131-42. [Crossref] [PubMed]
- Wanezaki M, Watanabe T, Nishiyama S, et al. Trends in the incidences of acute myocardial infarction in coastal and inland areas in Japan: The Yamagata AMI Registry. J Cardiol 2016;68:117-24. [Crossref] [PubMed]
- China Hypertension Prevention Guidelines Revision Committee. 2010 Chinese Guidelines for the Management of Hypertension. Zhonghua Xin Xue Guan Bing Za Zhi 2011;39:579-616. [PubMed]
- Chinese College of Emergency Physicans, Chinese Society of Cardiology, Chinese Society of Laboratory Medicine. Acute coronary syndrome emergency rapid diagnosis and treatment guide. Chin J Emerg Med 2011;39:579-616.
- Soeiro Ade M, Fernandes FL, Soeiro MC, et al. Clinical characteristics and long-term progression of young patients with acute coronary syndrome in Brazil. Einstein (Sao Paulo) 2015;13:370-5. [Crossref] [PubMed]
- Huang J, Qian HY, Li ZZ, et al. Comparison of clinical features and outcomes of patients with acute myocardial infarction younger than 35 years with those elder than 65 years. Am J Med Sci 2013;346:52-5. [Crossref] [PubMed]
- Haridasan V, Rajesh KF, Sajeev CG, et al. Study on correlation of obesity with short-term prognosis in acute myocardial infarction. Indian Heart J 2016;68:306-10. [Crossref] [PubMed]
- Janszky I, Romundstad P, Laugsand LE, et al. Weight and weight change and risk of acute myocardial infarction and heart failure - the HUNT Study. J Intern Med 2016;280:312-22. [Crossref] [PubMed]
- Zhang JX, Dong HZ, Chen BW, et al. Characteristics of coronary arterial lesions in patients with coronary heart disease and hypertension. Springerplus 2016;5:1208. [Crossref] [PubMed]
- Tam WC, Hsieh MH, Lin YK, et al. Silent and Malignant Early Repolarization Syndrome Mimicking Hyper-Acute ST Elevation Myocardial Infarction. Acta Cardiol Sin 2016;32:506-10. [PubMed]
- Koracevic GP. Proposal of a New Approach to Study and Categorize Stress Hyperglycemia in Acute Myocardial Infarction. J Emerg Med 2016;51:31-6. [Crossref] [PubMed]
- Hajizadeh R, Ghaffari S, Salehi R, et al. Association of serum uric acid level with mortality and morbidity of patients with acute ST-elevation myocardial infarction. J Cardiovasc Thorac Res 2016;8:56-60. [Crossref] [PubMed]
- Shacham Y, Gal-Oz A, Flint N, et al. Serum Uric Acid Levels and Renal Impairment among ST-Segment Elevation Myocardial Infarction Patients Undergoing Primary Percutaneous Intervention. Cardiorenal Med 2016;6:191-7. [Crossref] [PubMed]


