Upper lobe anterior segment (S3): technique of fissureless uniportal VATS segmentectomy
Introduction
There is a growing interest for minimally invasive sublobar anatomic resections. Whereas some segmentectomies like lingulectomy or S6-resection appear trivial for experienced surgeons, other sublobar anatomic resections with large parenchymal surface remain challenging. In our video, we demonstrate our technique to separate a fused interlobar fissure between upper and middle lobe, safely allowing to proceed to S3-segmentectomy.
Case presentation
The patient is a 57-year-old male with no relevant past medical history. One year before he was incidentally found to have a 19 mm ground glass opacity in the right upper lobe on a computed tomography done for minor trauma. In the follow-up examination the solid part of the lesion thickened (Figure 1A) and positron emission tomography (PET) showed moderate radionuclide uptake with no other suspect lesions. Lung function tests were normal [FEV1 4.14 L (90% of predicted value)]. We decided to propose a segmentectomy for diagnostic and therapeutic purpose.
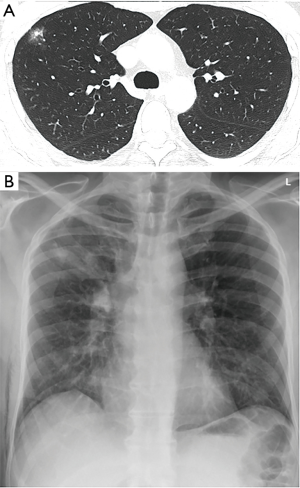
A uniportal VATS resection of the right upper lobe anterior segment was performed. Operative time was 150 minutes and the blood loss was 40 mL. The fresh frozen section showed no invasive carcinoma with free margins of more than 1 cm which was confirmed by the definitive histopathology results with the following tumor stage: pTis pN0 (0/7) R0. The chest tube was removed on post-operative day 2 and the patient was discharged the following day (Figure 1B).
Surgical technique (Figure 2)

General anesthesia with a double lumen endotracheal tube was used. The patient was placed in a left lateral decubitus position. A 3 cm incision in the 5th intercostal space was made in the anterior axillary line. We used a SurgiSleeveTM XS wound protector to avoid smearing of the scope. After entering the thoracic cavity with a 5 mm/30° camera an intercostal anesthesia was performed under sight with 20 mL of ropivacaine 0.75%.
Separating middle from upper lobe (5 steps)
Since the horizontal fissure was completely absent we needed to separate the middle from the upper lobe to have a good visual access to the bronchovascular pedicle of segment 3. The first step is to dissect the pulmonary artery in the oblique fissure at the point where it is crossed by the posterior vein branch of the upper lobe (V2). This will be the point where we intend to exit after tunneling alongside V2 from the hilum. Next comes the mediastinal preparation with identification of the upper lobe vein and its V2 branch, which is the path we will follow to reach the exit point we have already prepared the step before. For better visibility, the V3 branch can be sectioned at this stage if needed. Thirdly, we identify the main pulmonary artery and the middle lobe artery (A4) between the middle and upper lobe veins. It is important for a smooth tunneling with the dissecting clamp to open the vascular sheath of the aforementioned vessels. Subsequently the passage of the instrument is done along the V2-venous branch, taking meticulous care not to harm A4 and the ascending A2 arteries. Finally, after passing a silastic sling for better visualization, the parenchyma can be divided with a stapling device, which now offers perfect exposure of the bronchovascular pedicle of segment 3. It is possible to start the division of the parenchyma a few steps before if the visibility is disturbed by a large middle lobe.
Segmentectomy
We continue with the dissection of the vein. In this case V3b and V3a had a common trunk and were sectioned with a 35 mm powered vascular stapling device (Echelon Flex™ powered vascular stapler, Ethicon). We proceed with the A3 artery, which can arise from the anterior trunk or directly from the main pulmonary artery. After dissection of the segmental bronchus and placement of the powered vascular stapler at its base, the lung is inflated to define the plane between segment 3 and the remaining upper lobe. When stapling the parenchyma, one should take care not to let slip the lung out of the device. We found it helpful to lift and dissect away the bronchial stump from the remaining lung and to staple the parenchyma from different directions to diminish the tension on the suture line. The specimen is then removed using a retrieval bag. We use the time of frozen section analysis (diagnosis and resection margins) to perform the mediastinal lymphadenectomy (station 2R, 4R, 7 and 8). The operation is concluded by a lavage of the thoracic cavity, chest tube insertion and lung ventilation under sight.
Comments
Complex sublobar anatomic resections performed under minimally invasive techniques (uniportal, multiportal VATS or robotic) need a thorough knowledge of the anatomy. We can warmly recommend the lecture of the atlas from Nomori (2) to any interested surgeon.
Moreover, due to the various existing anatomic variations the study of a high resolution computed tomography of the chest, including three-dimensional reconstructions if available, is mandatory to properly plan the resection. The restricted level of freedom in uniportal VATS compared to open surgery makes the adaptation and the development of knew operative strategies necessary.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and the accompanying images and video.
References
- Lutz JA, Dorn P, Schmid RA, et al. Uniportal upper lobe anterior segmentectomy. Asvide 2018;5:581. Available online: http://www.asvide.com/article/view/25556
- Nomori H, Okada M. Illustrated Anatomical Segmentectomy for Lung Cancer. Tokyo: Springer, 2011.


