Renal denervation with ultrasound therapy (paradise device) is an effective therapy for systemic hypertension
Hypertension is the most important risk factor for cardiovascular events associated morbidity and mortality, affecting more than one billion people worldwide (1). Although anti-hypertensive drug therapy is very effective in reducing the risk of cardiovascular disease and death, approximately 10% of patients suffer from resistant hypertension despite at least three maximally tolerated doses of anti-hypertensive drugs including a diuretic (2). Endovascular renal denervation has been investigated as a new treatment strategy, and prior unblinded, randomized trials have shown promising results with reduction of systolic and diastolic blood pressure (BP) (3,4). However, SYMPLICITY HTN-3 trial, a randomized, blinded, sham-controlled trial failed to show a significant reduction in office systolic blood pressures (SBPs) after renal denervation as compared to sham control (5). Post-hoc analysis revealed that variable adherence to anti-hypertensive medications, and incomplete renal denervation were the likely causes of the unexpected failure to reduce BP (6).
Recently, Townsend et al. reported 3 months results of the SPYRAL HTN OFF-MED trial, that demonstrated a significant reduction in 24-hr ambulatory BP in patients receiving Spyral multielectrode radiofrequency ablation (Medtronic, Galway, Ireland), compared with sham control non-medicated patients with mild to moderate hypertension (office systolic-BP ≥150 but <180 mmHg, office diastolic-BP ≥90 mmHg; a 24-hr ambulatory systolic-BP of between 140 and 170 mmHg at second screen) (7). Subsequent to the OFF-MED trial, the efficacy of renal denervation for patients with moderate, uncontrolled hypertension despite anti-hypertensive drugs was evaluated in the SPYRAL HTN ON-MED trial with similar study design—with the exception that patients were on 1 to 3 anti-hypertensive medications. Similar to the OFF-MED trial, office and 24-hr ambulatory BP decreased significantly in the renal denervation group (difference of −6.8 mmHg, 95% CI: −12.5 to −1.1, P=0.0205) compared to sham control. The extent of BP reduction with renal denervation increased over the follow-up period to 6 months (8).
In The Lancet, Azizi et al. reported the results of the RADIANCE HTN SOLO trial (9) using endovascular ultrasound renal denervation system (Paradise renal denervation system, ReCor, CA, USA) with ambulatory SBP equal to or greater than to 135 but less than 170 mmHg or diastolic blood pressure (DBP) equal or greater than of 85 but less than 105 mmHg after a 4-week of discontinuation of up to two anti-hypertensive medications. A total of 146 patients were randomized to undergo renal denervation (n=74) or a sham control (n=72) and the primary effectiveness endpoint was statistically significant BP reduction based on daytime ambulatory BP from baseline to 2 months, between test and sham controls. To prevent unmasking all patients were sedated and wore headphones and eye covers. Endovascular ultrasound renal denervation achieved a significantly greater reduction in daytime ambulatory systolic-BP (–8.5±9.3 mmHg) than sham procedure (–2.2±10.0 mmHg); baseline-adjusted difference between groups: –6.3 mmHg, 95% CI: –9.4 to –3.1, P=0.0001). No major adverse events were observed in either group. However, the major limitation of the study was the lack of robustness in anti-hypertensive medications. According to the pre-defined protocol, all patients were considered to discontinue anti-hypertensive medications until 2 months after the procedure 4 of 74 (5%) patients in the renal denervation group and 10 of 72 (14%) patients in the sham group took anti-hypertensive medications during the 2-month follow up, on the basis of the physician’s decision or patient preference, and therefore didn’t meet protocol-defined criteria. In addition, drug surveillance was not performed, therefore the Hawthorne effect could not be ruled out.
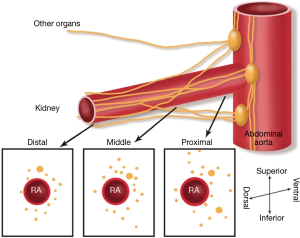
Despite several endovascular renal denervation devices having been shown to be clinically safe and effective prior to 2013 (3,10), the human anatomy of peri-arterial renal nerves had not been thoroughly investigated, as most of the devices advocated denervation of the proximal renal arteries close to the ostium. In 2014, we reported the anatomic distribution of peri-arterial renal nerves surrounding the renal arteries from the ostium to the bifurcation (11). We showed that the distal regions of renal artery prior to bifurcation had sympathetic peri-renal nerves located closer to the renal artery as compared to proximal and middle segments, however the nerves were far smaller and fewer in the distal regions compared to proximal and middle (Figure 1). The distribution of the distance of nerves from the renal artery varied considerably, from <1 to >10 mm, and the 75th and 90th percentile of nerve were located at a distance from renal artery was 4.28 and 6.39 mm, respectively. However, the distal nerves had the shortest distance from the artery lumen with 75th and 90th percentile of nerves was 3.24 and 5.27 mm, respectively. This data suggests it is possible that some of the nerves may not have been affected by the radiofrequency ablation procedure, as the depth of injury would have to exceed 5mm to have affected 80% of the nerves.
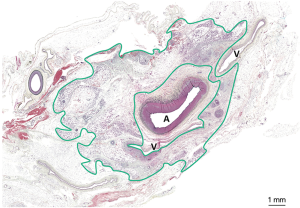
Paradise catheter consists of a through lumen shaft that delivers ultrasound energy via piezoelectric ceramic transducer located at the distal end of the balloon catheter which uses sterile circulating water to protect the renal artery approximately 1 mm around the balloon (11). In a previous swine preclinical study, Paradise catheter demonstrated nearly 360-degree circumferential ablation, while preventing renal artery medial damage and the maximum and minimum depth of ablation was 11.9 and 1.2 mm (Figure 2) (12). In the RADIANCE HTN SOLO trial, the duration of the ablation was 7 seconds and the mean number of ablations was 5.4±1.0 and they were performed at a distance 5 mm apart with an average total time of treatment 37.9±6.7 seconds, and total procedure time of 72 minutes. On the other hand, Spyral catheter, used in the SPYRAL HTN OFF-MED and ON-MED trials, has 4 electrodes, which enables to apply radiofrequency energy circumferentially at a distance from one another in four quadrants of the renal artery. Distal renal artery, branches, as well as accessory arteries were treated. In the SPYRAL HTN ON-MED trial, mean total denervation time was 60.8±25.3 minutes, and the mean number of ablations was 45.9±13.7 times (19.3±8.9 times for main arteries, and 26.6±11.7 times for branch vessels) with a total procedure time of 92.5±38.4 minutes.
Endovascular renal denervation with the two latest generation catheter devices has shown safety and both are associated with significant reductions in BP compared with a sham procedure. We believe the latest generation of renal ablation devices are effective in reducing moderately high systolic and diastolic BP. Although the site of ablation was different in the two procedures one proximal and mid and the other distal renal artery and branches using two different modalities, ultrasound and radiofrequency ablation techniques. However, several clinical questions still remain unresolved. Firstly, why were 13/74 (18%) patients in RADIANCE HTN SOLO and 9/36 (25%) in SPYRAL HTN ON-MED non-responder? Second, is renal ablation effective long-term? Lastly does it reduce the risk of cardiovascular death? Further studies with larger numbers of patients and longer follow-up duration will be required prior to acceptance of this therapy as stand alone or with anti-hypertensive medications, especially in patients who are noncompliant.
Acknowledgements
None.
Footnote
Conflicts of Interest: Sho Torii receives research grants from SUNRISE lab. Renu Virmani and Aloke V. Finn have received institutional research support from Abbott Vascular, Boston Scientific, Cook Medical, Cardiovascular Systems, Inc., Medtronic, ReCor Medical, and Terumo Corporation; Renu Virmani is a consultant for 480 Biomedical, Abbott Vascular, Medtronic, and W.L. Gore. The other authors have no conflicts of interest to declare.
References
- Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957-67. [Crossref] [PubMed]
- Kumbhani DJ, Steg PG, Cannon CP, et al. Resistant hypertension: a frequent and ominous finding among hypertensive patients with atherothrombosis. Eur Heart J 2013;34:1204-14. [Crossref] [PubMed]
- Esler MD, Krum H, Sobotka PA, et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 2010;376:1903-9. [Crossref] [PubMed]
- Krum H, Schlaich MP, Sobotka PA, et al. Percutaneous renal denervation in patients with treatment-resistant hypertension: final 3-year report of the Symplicity HTN-1 study. Lancet 2014;383:622-9. [Crossref] [PubMed]
- Bhatt DL, Kandzari DE, O’Neill WW, et al. A controlled trial of renal denervation for resistant hypertension. N Engl J Med 2014;370:1393-401. [Crossref] [PubMed]
- Kandzari DE, Bhatt DL, Brar S, et al. Predictors of blood pressure response in the SYMPLICITY HTN-3 trial. Eur Heart J 2015;36:219-27. [Crossref] [PubMed]
- Townsend RR, Mahfoud F, Kandzari DE, et al. Catheter-based renal denervation in patients with uncontrolled hypertension in the absence of antihypertensive medications (SPYRAL HTN-OFF MED): a randomised, sham-controlled, proof-of-concept trial. Lancet 2017;390:2160-70. [Crossref] [PubMed]
- Kandzari DE, Bohm M, Mahfoud F, et al. Effect of renal denervation on blood pressure in the presence of antihypertensive drugs: 6-month efficacy and safety results from the SPYRAL HTN-ON MED proof-of-concept randomised trial. Lancet 2018;391:2346-55. [Crossref] [PubMed]
- Azizi M, Schmieder RE, Mahfoud F, et al. Endovascular ultrasound renal denervation to treat hypertension (RADIANCE-HTN SOLO): a multicentre, international, single-blind, randomised, sham-controlled trial. Lancet 2018;391:2335-45. [Crossref] [PubMed]
- Krum H, Schlaich M, Whitbourn R, et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 2009;373:1275-81. [Crossref] [PubMed]
- Sakakura K, Ladich E, Cheng Q, et al. Anatomic assessment of sympathetic peri-arterial renal nerves in man. J Am Coll Cardiol 2014;64:635-43. [Crossref] [PubMed]
- Sakakura K, Roth A, Ladich E, et al. Controlled circumferential renal sympathetic denervation with preservation of the renal arterial wall using intraluminal ultrasound: a next-generation approach for treating sympathetic overactivity. EuroIntervention 2015;10:1230-8. [Crossref] [PubMed]


