
Chordal replacement versus quadrangular resection in degenerative posterior mitral leaflet repair
Introduction
Degenerative mitral regurgitation (MR) caused by posterior mitral leaflet (PML) prolapse is the major type of mitral valvular disorder and remains a medical problem worldwide (1,2). Mitral valve (MV) repair has been proven better than replacement in treating degenerative MV disease (2,3). Established and standardized by Carpentier, quadrangular resection (QR) and its derivative resectional techniques have long been the gold standard for treating MR with documented excellent long-term results (4,5). However, when the pathologies are extensive and multi-segmental, resection becomes less feasible without compromising the mobility of the PML and the subsequent MV function (6,7). Circumflex artery injury is among other known problems associated with resection techniques (8). Used primarily for AML repair (9), chordal replacement (CR) by expanded polytetrafluoroethylene (ePTFE) suture was later adopted for PML repair and has also delivered appealing long-term results (10,11). To date, albeit in different settings, a few studies have reported comparable outcomes of resectional versus neochordal techniques for MV repair (7,8,10-12). However, compared to QR, little is known for the potential of CR in treating isolated degenerative PML (idPML) prolapse, especially when regarding surgical approach, length of operation and hospital stay, propensity to incur complications and the recurrence of MR. The present study aims to assess mid- to long-term outcomes of CR versus QR for idPML repair in order to analyze the versatility, effectiveness, safety and durability between these two techniques.
Methods
Patients
From 4/2010 to 12/2015, 346 consecutive patients underwent degenerative MV repair at our center. MV pathology was confirmed myxomatous change in these patients. Fifteen patients were treated with both QR and CR and 136 patients with neither (e.g., annuloplasty only). Of the remaining population, patients were excluded if MV pathologies involved anterior mitral leaflet (AML) or commissures (n=83). A total of 112 patients were diagnosed with idPML prolapse with MV repaired by either CR (n=33, 29%) or QR (n=79, 71%) (Figure 1).

Surgical technique
Operative management
The technique for MV repair and the surgical approach (conventional median sternotomy versus right lateral minithoracotomy) were chosen by surgeon preference. Accordingly, cardiopulmonary bypass was established through either aortic or femoral cannulation. All patients received semirigid partial annuloplasty ring (Sorin Group, Saluggia, Italy) when repair was completed. The ring was sized according to the height of AML and the intercommissural distance.
CR with “loop” technique
The loop technique was applied as Seeburger et al. described (10). The length of the loop was determined either through preoperative transesophageal echocardiography (TEE) where the level of the normal anterior leaflet was measured, or by direct intraoperative measurement with a ruler. The common tail end with pledget of premade CV4 ePTFE Gore-Tex Suture (W. L. Gore & Associates, Inc., Flagstaff, AZ) loops was anchored to the tip of the papillary muscle. The free loop ends were attached in a fan fashion to the free margin of the prolapsed segment so as to support the whole area (12).
QR
A standard Carpentier QR technique was used to remove redundant leaflet tissue. Approximation of the leaflet remnants was completed by using either annular plication or sliding annuloplasty whenever necessary (13).
Follow-up
The median follow-up time was 26 months (95% CI: 21.9–30.1 months). All of the patients had postoperative transthoracic echocardiography (TTE) before and after surgery and every 6 months thereafter. MV regurgitation was graded on a scale from 0+ to 4+ (0 none, 1+ trace, 2+ mild, 2.5+ mild to moderate, 3+ moderate, 3.5+ moderate to severe and 4+ severe) (13). One UCG (ultrasonic cardiography) physician from the UCG department in our cardiac center conducted all TTE exams in this study. The semi-quantitative assessment was used in grading the MR severity, by which the regurgitant jet extension to the left atrium area was compared. And the final MR grading was obtained from at least two different views.
The primary endpoint was all-cause mortality, and the secondary endpoints were composite endpoints including cardiac death, re-intervention, cardiac complications, composite thrombosis, embolism, bleeding, renal failure and infections.
Statistical analysis
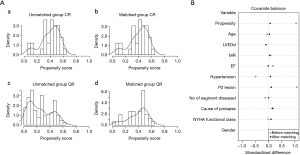
Propensity score matching (PSM)
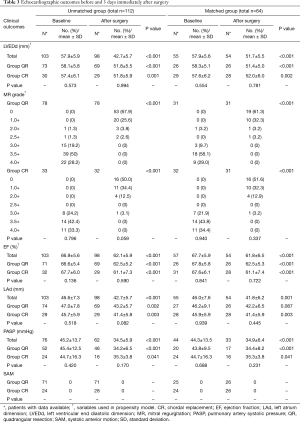
Although baselines between group CR and group QR were generally similar, PSM (PSMATCHING 3.03, Thoemmes, F, Cornell University) was performed to even the minor differences in patient characteristics for fair comparisons (Table 1). Based on previously reported preoperative factors (7) and factors which may influence surgeons to perform CR for PML repair, we recruited 10 key variables (including valve morphology, c-statistic of the regression model =0.748) to run a 1:1 PSM between groups. Through a greedy matching strategy for the probability of having CR, patients were well matched across the propensity score spectrum (Figure 2).

Full table
Presentation
Median follow-up was calculated following the reverse Kaplan-Meier method. Continuous variables are expressed as mean ± SD and categorical variables as frequencies. Continuous data were compared by Wilcoxon rank-sum test, categorical data by the χ2 test or Fisher’s exact test when frequency <5, and time-to-event outcomes by Kaplan-Meir analysis. Cox regression was performed to spot independent predictors for time-to-event outcomes. Statistical significance was considered as P<0.050. All data analysis was performed using SPSS software for Windows, version 22 (IBM Corporation, Armonk, NY) and Prism 6 (GraphPad Software, Inc., La Jolla, CA).
This study was conducted from 12/2016 to 5/2017. The results are compiled from multiple surgeons in our cardiac center. It was approved by the Ruijin Hospital Ethics Committee as an exempt research (NO. 2016-126). All personally identifiable information was coded and protected against inappropriate use and disclosure.
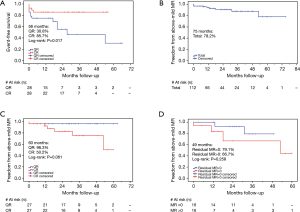
Results (Figures 3,4)
Versatility
Although annulus plication or sliding annuloplasty were often and only carried out with QR, there was no significant difference in the size of annuloplasty rings implanted between group QR and group CR (P=0.412) (Table 2). Median sternotomy was chosen more frequently with QR than with CR (P<0.001). By contrast, group CR used minimally invasive one more often (P<0.001). No conversion from mini-invasive procedure to sternotomy occurred. The myocardial ischemic time between groups was statistically insignificant in both unmatched and matched comparisons (Table 2).
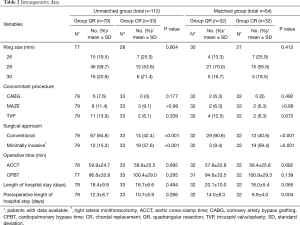
Full table
Effectiveness
MV repair was accomplished successfully in both groups, with no cross over between groups or shift from valve repair to valve replacement. By TTE 3 days after surgery, both groups had significant decreases in MR grading, left ventricular end-diastolic diameter (LVEDd), and left ventricular ejection factor (EF). Remarkable decreases in left atrium diameter (LAd) and pulmonary artery systolic pressure (PASP) were also observed in both groups. No significant difference was found in postoperative echocardiographic outcomes between groups (Table 3). The overall residual MR (rMR) (by UCG acquired 3 days immediately after surgery) between group CR and QR was statistically insignificant, but CR tend to leave more rMR than group QR under minimally invasive approach rather than under conventional one (P=0.058 vs. P=0.571).
Full table
Safety
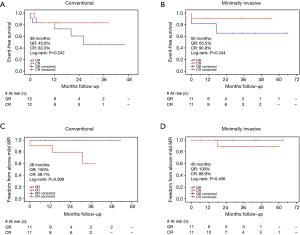
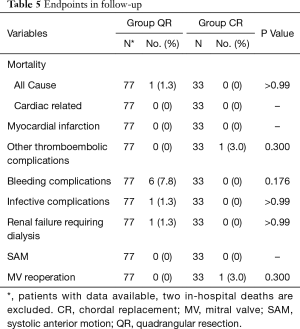
No systolic anterior motion (SAM) happened during the entire study. Group CR showed much shorter postoperative (CR 9.9±4.0 vs. QR 14.0±8.3 days, P<0.004) and total (CR 16.0±5.4 vs. QR 20.1±10.0 days, P=0.065) in-hospital time. This trend of difference stayed even when add surgical approach into the propensity score model as covariate to reduce the bias possibly brought by minimally invasive versus conventional approaches. The morbidity and mortality were quite low in both two groups, yet, with significant difference, more adverse events (composite endpoints) such as death, stroke, bleeding, infective complications, mediastinal reexploration, etc., occurred in group QR [56 months: CR 85.7% vs. QR 30.8%, P (log-rank) =0.017] (Figure 3A). This difference remained between matched patients under same surgical approach [conventional approach: 38 months: CR 83.3% vs. QR 45.6%, P (log-rank) =0.242; minimally invasive approach: 55 months: CR 90.9% vs. QR 65.5%, P (log-rank) =0.244] (Figure 4A,B). Although no death occurred in patients after PSM during the study, there were 2 in-hospital deaths from the entire patient cohort (unmatched) with the 30-day mortality at 1.8%, and both deaths were in group QR (2.5%). The causes of mortality were massive cerebral infarction (n=1) and pneumonia (n=1).
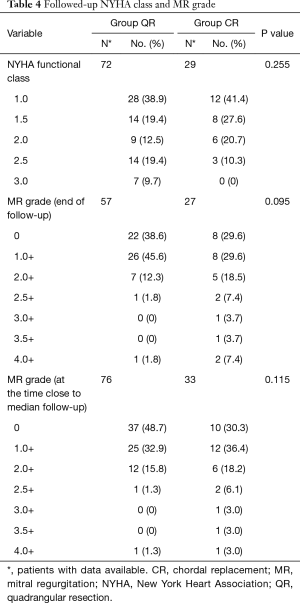
Durability
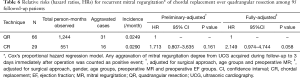
At the latest follow-up, the majority of patients showed satisfactory improvements in clinic symptoms associated with cardiac function. There was no significant difference in NYHA functional class between groups (Table 4). Overall freedom from above-mild recurrent MR (MR ≥2.5+) at 75 months was 78.2% (95% CI: 50.5–91.5%), whereas no recurrent MR at such early stage has been reported so far (Figure 3B). More above-mild recurrent MR between matched patients was shown in group CR than group QR at 20, 40 and 60 months [CR: 82.8%, 75.3%, 50.2% vs. QR: 96.3%, 96.3%, 96.3%, respectively, P (log-rank) =0.061] (Figure 3C). This trend was unchanged regardless of surgical approach between matched patients [conventional approach: 38 months: CR 59.7% vs. QR 100%, P (log-rank) =0.098; minimally invasive approach: 45 months: CR 88.9% vs. QR 100%, P (log-rank) =0.456] (Figure 4C,D). One valve-related reoperation (valve replacement) occurred because of severe recurrent MR developed 14 months after CR (Table 5). In group CR, no significant difference between 16 patients with no rMR (rMR =0) and 16 patients with rMR (rMR >0) was found for developing above-mild recurrent MR over time [49 months: rMR =0, 79.1% vs. rMR >0, 66.7%, P (log-rank) =0.258] (Figure 3D). Cox regression analysis might suggest that CR technique was a risk factor for recurrent MR (CR over QR, HR 2.149; 95% CI: 0.974–4.744; P=0.058; adjusted for approach, gender, age, preoperative MR and EF) (Table 6).
Full table
Full table
Full table
Discussion
MV repair aims to restore the physiological structure and function of the MV. The fundamental principles of MV reconstruction include: (I) to create a large enough coaptation surface; (II) to preserve or restore the native leaflet mobility; (III) to remodel and stabilize the annulus; (IV) to keep the mitral orifice as large as normal (13). CR with ePTFE suture is now often used as an alternative to conventional resectional techniques in MV repair, not only because chordal elongation and/or rupture is the major cause for degenerative mitral disease (14), which can be directly corrected through neochordal replacement, but also because the emerging paradigm of “respect rather than resect” in degenerative MV repair becomes popular in recent years (15) and the limitations for resectional techniques like extensive pathologies do not contraindicate the use of CR (7,16,17). However, when insights are needed to make rational surgical choices for treating individual patients with idPML prolapse, reports on outcome comparisons between CR and QR regarding their versatility, effectiveness, safety and durability within matched populations were few.
In this study, we did not find any preferential difference for the number of diseased mitral segments in carrying out QR or CR. This is largely because most cases enrolled were not multi-segmental, mainly due to the improvement in early diagnosis and referral for surgical intervention in our community. The simplicity of CR has been shown particularly relevant in small access incisions where resection may prove challenging (16), and we do observe most CRs were performed by our surgeons under such approach, however in our study, its merit was not expressed by the difference of surgical time but by the length of hospital stay and the morbidity and mortality rate between two techniques, even when taken the surgical approaches into concern.
In contrast to some reports that QR results in implantation of smaller annuloplasty rings than CR, which may or may not lead to smaller mitral orifice area as well as higher transvalvular gradients (10,11), our results did not show a significant difference between QR and CR regarding the ring size. According to Carpentier-standardized method, the size of MV annuloplasty ring is determined by intraoperatively measuring the height of AML and the intercommissural distance (13). In our present study of idPML repair, with few cases of extensive lesions enrolled, the changes of AML and annulus morphology after QR were minor, thus the sizing of rings for QR was not significantly affected by PML resection. Such findings are also in line with other published data (8,12).
The postoperative decline of EF by TTE shown in Table 3 in both groups is due to the physiological change of a successful MV repair. MV repair decreases the loading condition of the left ventricle and enlarges its systolic dimension (18). Also, the baseline EF is potentially masked (overvalued) as MR is characterized by pumping blood fore- and back-ward, and the backward flow is rectified after repair (19). The apparent improvements in clinical symptoms and NYHA functional class clearly suggested a corrected stroke volume, and the myocardial contractility would improve over time.
In David’s 25-year experience on CR for treating degenerative mitral disease, the recurrence of MR has been noticed as common, of which freedom from moderate or severe recurrent MR (MR ≥3.0+) at 1, 10, and 18 years was 98.5%, 87.8%, and 67.5%, respectively (20). There is data suggesting that in CR for AML repair, the intensity of recurrent MR after surgery would increase over time, which was not seen in patients with a thorough repair from surgery (rMR =0) (21). Park also reported that group CR had an insignificantly higher volume of residual regurgitation than group QR under standard median sternotomy (8). In our study regarding idPML repair, group CR was shown to leave relatively more rMR than group QR under minimally invasive approach but not under conventional one, implicating that CR is technically more demanding with small incision than with standard median sternotomy. Furthermore, whereas no recurrent MR has been reported at the above-mild stage (MR ≥2.5+) so far, which we believed is an early sign of the ongoing deterioration of MV competence, CR was observed in this study to develop such recurrent MR over time, regardless of whether the MV competence was fully corrected or not during surgery. These results explain well why CR was found to be a possible risk factor for recurrent MR. The long-term clinical relevance of above findings warrants further investigation.
Limitations
This is a single-institution, observational study of patients who underwent PML repair with CR or QR techniques by limited surgeons under limited follow-up time. While all surgeons in this study were familiar with abovementioned surgical techniques, a selection bias that was caused by surgeon preference still might exist. Although PSM aided much fair comparisons between groups as there were differences in baselines, e.g., differences in diseased valve morphology and MR grade, which were important factors that governed whether a patient received one surgical technique as opposed to another and clinical prognosis, the decrease in sample size after matching might dampen the power of statistics and the generalization of results. Additional randomized trials are warranted to eliminate those limitations.
Conclusions
Both techniques were of excellent mid- to long-term clinical results for PML repair in this study. Less post-surgery complications and shorter hospital stay revealed the superiority of CR for its well adaptation to the minimally invasive approach. Nonetheless, QR better retains the MV competence over time. Overall observations implicate that CR in good hands with small incision might be more preferable for those with high surgical risks and/or short life expectancy. Further investigations are warranted to determine whether retaining of MV competence prolongs long-term survival and if yes, how to improve it in CR technique.
Acknowledgements
We thank Lei Shi, MD, for the maintenance of important medical and operational records, and Jiayin Wu, for his invaluable support and consultation on statistical analysis of this work.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Ruijin Hospital Ethics Committee as an exempt research (NO. 2016-126). All personally identifiable information was coded and protected against inappropriate use and disclosure.
References
- Virmani R, Atkinson JB, Forman MB. The pathology of mitral valve prolapse. Herz 1988;13:215-26. [PubMed]
- Madesis A, Tsakiridis K, Zarogoulidis P, et al. Review of mitral valve insufficiency: repair or replacement. J Thorac Dis 2014;6 Suppl 1:S39-51. [PubMed]
- Oliveira JM, Antunes MJ. Mitral valve repair: better than replacement. Heart 2006;92:275-81. [Crossref] [PubMed]
- Nardi P, Pellegrino A, Scafuri A, et al. Survival and durability of mitral valve repair surgery for degenerative mitral valve disease. J Card Surg 2011;26:360-6. [Crossref] [PubMed]
- Carpentier A. Cardiac valve surgery--the "French correction". J Thorac Cardiovasc Surg 1983;86:323-37. [PubMed]
- Tomita Y, Yasui H, Iwai T, et al. Extensive use of polytetrafluoroethylene artificial grafts for prolapse of posterior mitral leaflet. Ann Thorac Surg 2004;78:815-9. [Crossref] [PubMed]
- Mihaljevic T, Pattakos G, Gillinov AM, et al. Robotic posterior mitral leaflet repair: neochordal versus resectional techniques. Ann Thorac Surg 2013;95:787-94. [Crossref] [PubMed]
- Park KJ, Woo JS, Yi JH, et al. Outcomes of Mitral Valve Repair: Quadrangular Resection versus Chordal Replacement. Korean J Thorac Cardiovasc Surg 2013;46:124-9. [Crossref] [PubMed]
- Frater RW. 10th Goretex chorda anniversary. J Heart Valve Dis 1996;5:348-51. [PubMed]
- Seeburger J, Falk V, Borger MA, et al. Chordae replacement versus resection for repair of isolated posterior mitral leaflet prolapse: a egalite. Ann Thorac Surg 2009;87:1715-20. [Crossref] [PubMed]
- Lange R, Guenther T, Noebauer C, et al. Chordal replacement versus quadrangular resection for repair of isolated posterior mitral leaflet prolapse. Ann Thorac Surg 2010;89:1163-70; discussion 1170. [Crossref] [PubMed]
- Falk V, Seeburger J, Czesla M, et al. How does the use of polytetrafluoroethylene neochordae for posterior mitral valve prolapse (loop technique) compare with leaflet resection? A prospective randomized trial. J Thorac Cardiovasc Surg 2008;136:1205-discussion 1205-6. [Crossref] [PubMed]
- Carpentier A, Adams DH, Filsoufi F. Carpentier's reconstructive valve surgery. Elsevier Health Sciences, 2011.
- Turri M, Thiene G, Bortolotti U, et al. Surgical pathology of disease of the mitral valve, with special reference to lesions promoting valvar incompetence. Int J Cardiol 1989;22:213-9. [Crossref] [PubMed]
- Perier P, Hohenberger W, Lakew F, et al. Toward a new paradigm for the reconstruction of posterior leaflet prolapse: midterm results of the "respect rather than resect" approach. Ann Thorac Surg 2008;86:718-25; discussion 718-25. [Crossref] [PubMed]
- Adams DH, Rosenhek R, Falk V. Degenerative mitral valve regurgitation: best practice revolution. Eur Heart J 2010;31:1958-66. [Crossref] [PubMed]
- Perier P, Hohenberger W, Lakew F, et al. Prolapse of the posterior leaflet: resect or respect. Ann Cardiothorac Surg 2015;4:273-7. [PubMed]
- Quintana E, Suri RM, Thalji NM, et al. Left ventricular dysfunction after mitral valve repair--the fallacy of "normal" preoperative myocardial function. J Thorac Cardiovasc Surg 2014;148:2752-60. [Crossref] [PubMed]
- Witkowski TG, Thomas JD, Delgado V, et al. Changes in left ventricular function after mitral valve repair for severe organic mitral regurgitation. Ann Thorac Surg 2012;93:754-60. [Crossref] [PubMed]
- David TE, Armstrong S, Ivanov J. Chordal replacement with polytetrafluoroethylene sutures for mitral valve repair: a 25-year experience. J Thorac Cardiovasc Surg 2013;145:1563-9. [Crossref] [PubMed]
- Kasegawa H, Shimokawa T, Shibazaki I, et al. Mitral valve repair for anterior leaflet prolapse with expanded polytetrafluoroethylene sutures. Ann Thorac Surg 2006;81:1625-31. [Crossref] [PubMed]


