Three common exposures of the chest wall for rib fixation: anatomical considerations
Introduction
Open reduction and internal fixation of bony structures has not historically been in the armamentarium of the trauma surgeon; however, with the advent of new rib fixation technology such as the anterior osteosynthesis plate in the beginning of the last decade, surgical approaches have become more common and, increasingly, trauma and thoracic surgeons are operating on the chest wall (1). While thoracotomies, sternotomies and thoracoscopic procedures have been the purview of all general surgery trainees, the focus has always been on entering the thoracic cavity, not on the chest wall itself. Thus, the musculoskeletal anatomy outside of the thoracic cavity and exposure strategy for bony reduction are completely novel concepts to most surgeons first deciding to operate in this fashion. Furthermore, there is currently a significant paucity of information and published guidelines or surgical atlases focused on this area to enable surgeons to adequately prepare for these types of procedures.
In our institution we struggled with these challenges and learned through experience how best to treat this patient surgically when indicated. Techniques evolved and novel tools were utilized as our approaches became more sophisticated. In retrospect however, there are a few basic principles that, when followed, make approaches to the chest wall for rib fracture fixation much more straightforward than initially believed. What follows is a description of our experience with surgical fixation and analysis of the anatomy based on functional approaches to common injury patterns corroborated by information gleaned by cadaveric dissections.
Our chest wall injury program grew out of the recognition for improved methods of treating the most severely affected patients. Initially, we focused on those with devastating crush injuries of the chest involving multiple rib levels with extreme displacement. These injuries resulted in respiratory failure such that surgical fixation seemed necessary. Over the past seven years, as we became more comfortable with the surgical approaches, numerous publications came to the forefront touting the benefits of surgical fixation for both “flail” and non-flail rib fracture patterns, regardless of the need for mechanical ventilation. Simultaneously, our indications for rib fixation expanded as well. Eventually we would include patients with unstable chest wall injuries who had debilitating, intractable pain from these injuries. Our approaches became more dependent on the natural planes and spaces while our fixation technique grew more sophisticated along with the available technology. We steered away from large-scale division of muscles in favor of muscle-sparing, smaller incisions. We also were better able to safely access sections of the chest wall that had previously been avoided.
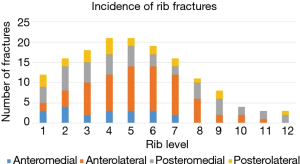
As part of a broader, IRB-approved retrospective chart review analyzing these injuries, we examined the electronic medical records in our level 1 trauma center of patients admitted for flail chest injuries over two years who had undergone rib fracture fixation (n=18). The number of ribs, locations of fractures, and severity were all mapped out utilizing Excel (Microsoft corp.) to identify the most common rib fracture patterns.
Next, we obtained un-embalmed adult cadavers from the anatomy department at Louisiana State University Health Science Center, New Orleans. Three approaches were selected based on the most frequent fracture patterns identified on our clinical database and our surgical experience to date. The anterolateral longitudinal approach was the first and most frequently used, followed by the posterolateral longitudinal approach, followed by a subscapular/modified posterior thoracotomy approach. The traditional anterolateral thoracotomy incision was also utilized but not described here as it is an approach well-known to most surgeons.
It should be mentioned that ribs 1 and 2 rarely require fixation and are exceedingly difficult to access safely while contributing relatively little to the overall instability of the chest wall. Similarly, ribs 11 and 12 do not contribute significantly to the action of respiration and are rarely fixed. Furthermore, ribs 11 and 12 are often exceedingly short and do not offer sufficient purchase on either side of the fracture to allow adequate placement of hardware. Another point of caution is that the intercostal nerves at this level contribute to lateral abdominal wall muscular tone and function. Care must be taken if this rib segment is to be manipulated in any way because injuring the intercostal nerve can result in a flank pseudo-hernia that can be disfiguring, painful, and exceedingly challenging to treat (2). Furthermore, it can create lower thoracic instability that may compromise repair of the adjacent plated ribs which may result in hardware failure.
Operative techniques
Anterolateral longitudinal incision
Surgical approach
- Incise from the inferior edge of the axillary hair-bearing area caudad to expose the fracture line;
- Orient the incision over the majority of the rib fractures;
- Dissect along the anterior border of the latissimus dorsi and elevate that muscle;
- Identify the serratus anterior muscle, noting the approximate location of the long thoracic nerve in the midaxillary line (if not visible);
- Divide the serratus anterior along its anterior portion approximately 2–3 cm from the muscle insertion onto the rib;
- Using a finger-sweep, bluntly elevate the serratus anterior from underlying ribs.
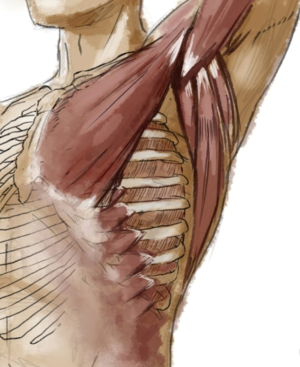
Anterolateral approach—discussion
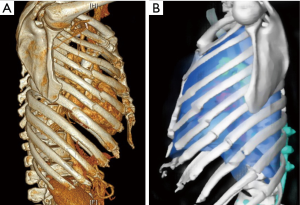
Fractures of ribs 4–8 on the anterolateral ribcage are the most common injury pattern we identified (Figure 1). The reasons for this may be that typical forces sufficient to cause significant injury most often result from facing forward on a motorized vehicle and experiencing an anteroposterior vector of impact causing compression failure of the lateral elements. This is often termed “compression force” and helps explain the injury pattern noted in many patients whose injuries were sustained in a high-speed collision where the point of impact was the anterior or posterior torso (3). The location of the insertion of the serratus anterior may partially explain this as well given the forces that it exerts on that particular location of the rib cage when, for example, a person braces for impact and the serratus acts as a fulcrum for the forces at play (4). Anecdotally, it appears that anterolateral fractures most frequently occur either just posterior to the insertion of the serratus or at the precise point of insertion on the rib and the fracture line often follows the contour of the serratus insertion, curving posteriorly as it inserts on subsequent inferior ribs (Figure 2).
Isolated anterolateral fractures can be repaired in the supine position with the arm abducted to 90 degrees. This allows the surgeon to perform the procedure in the most natural position for the patient and allows two surgeons to operate simultaneously on both sides in the case of a bilateral anterolateral fracture pattern. In the event that anterior and ipsilateral posterior rib fracture patterns are present and require fixation, the lateral decubitus position may be preferred in order to access both segments without re-draping and allow simultaneous repairs.
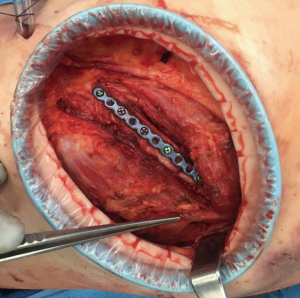
The serratus anterior, naturally, is the main obstacle in accessing fractures in the anterolateral location. Its function is to stabilize the scapula and, in turn, the entire shoulder girdle during extremity abduction, particularly forward abduction. Failure of this action, commonly referred to as “winging of the scapula,” results in significant weakness of the upper extremity in this position and even pain with routine activity. It is imperative, therefore, that the serratus remain both attached and innervated. The innervation of the serratus anterior is the Long Thoracic Nerve of Bell (LTN), emanating from the ventral rami of C5–C7, descending superficial to the external surface of the serratus anterior, and emitting branches to each of the muscular digitations (5). Division of the LTN anywhere but at its lowest point on the serratus anterior may result in significant weakness of the muscle. Division, or more likely crush injury from traction, of the upper LTN results in complete paralysis of the serratus anterior and severe winging of the scapula. The safest way to prevent this and gain access to the rib cage deep to the serratus is to divide it longitudinally just posterior to its insertion on the ribcage (Figure 3). By dividing longitudinally, one ensures that the division is perpendicular to the course of the nerve even if it is not readily seen in the operative field. This maneuver allows maximal exposure of the anterolateral ribcage while at the same time protecting the nerve from direct injury. One must still take great care in cephalad retraction of the muscular elements as the LTN may be inadvertently crushed. Gentle retraction is advocated as routine and is especially necessary in the cephalad aspect of the anterolateral wound. In the event of a complete transection of the LTN resulting in serratus paralysis, physical therapy can help strengthen the trapezius and rhomboids in order to compensate and minimize symptoms (6). Severe symptoms may be alleviated surgically in some cases (7).
Lastly, for access to the anteromedial ribcage, one must navigate the pectoralis insertion superiorly. Pectoralis minor inserts deep to pectoralis major at ribs 2–5. It is sometimes necessary to expose the anterior cortex of the rib at this level in order to provide a landing zone for the anterior portion of a fixation plate. Dissection of the attachments of pectoralis minor off the ribs can be challenging in this area through a limited incision and difficult to visualize. These attachments may be rather tenacious, especially in young athletic patients, and bleeding that further obscures the surgical planes is often encountered. Great care, however, must be taken to avoid injuring the structures in the apex of the wound, namely the axillary vessels, LTN and brachial plexus.
Muscle-sparing approach—anterolateral
The serratus anterior muscle is divided into three functional components, each engaging the scapulothoracic interface at a slightly different angle to achieve shoulder stabilization and optimal positioning of the glenohumeral joint to facilitate upper extremity actions such as throwing and retrieving objects with the extremity abducted (6). Surgical splitting of the serratus anterior can be utilized to access the chest wall underneath, but great care must be taken to avoid inadvertent division of the LTN, as described above (Figures 4,5). Avoiding cautery division of the fibers as one proceeds posteriorly is essential. The surgeon should use blunt division of the muscle, reserving cautery only for focal bleeding to maximize safety. However, there is a limit, in this author’s view, to how cephalad one can proceed safely. I find it safest to reserve muscle splitting of the serratus to the inferior third of the muscle, the lowest segment (inserting into ribs 6–9) and never to split the muscle cephalad to the 5th rib. If access is necessary above this level, I rely on division of the serratus approximately two finger-breadths posterior to its insertion, as previously described.
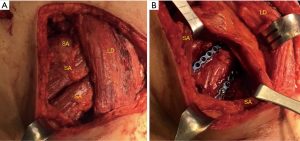
Schulz-Drost has described a minimized approach to chest wall fixation in this area utilizing a relatively small incision and relying entirely on splitting of the overlying musculature to access up to four rib fractures (8). They and others advocate the use of circular wound protectors to circumferentially retract the tissue and allow a window-like wound that can be manipulated in order to gain access to a larger area of the chest wall than is exposed by the skin incision (Figure 5) (8,9). These wound protectors are available from multiple vendors in various sizes and are disposable.
Some authors advocate for the use of an inframammary incision (9,10). While I agree it is a reliable way to access the upper anteromedial chest wall, I have found that the majority of patients I have treated surgically with fractures of the upper medial or lateral chest also have fracture lines that extend below the 5th rib. The horizontal incision of the inframammary approach renders the lower fractures less accessible. Therefore, I tailor the incision in this area to the fracture pattern. I start in the lower axilla and extend the incision medially in an inframammary approach for a focal area of instability, or extend it from axilla caudally to expose a line of fractures in the inferior area.
Posterior (auscultatory triangle) longitudinal incision
Surgical approach
- Incise from just medial to the scapula and extend the incision caudad as needed to cover the majority of the fractures;
- Elevate skin edges to expose the auscultatory triangle;
- Sharply dissect through loose connective tissue in the gap between the borders of the triangle;
- Perform a finger sweep maneuver to bluntly dissect and elevate trapezius, latissimus, and scapula off of the underlying ribcage;
- Sharp dissection and elevation of paraspinous muscle (iliocostalis thoracis) rib insertions may be necessary.
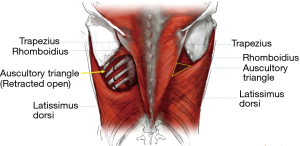
Posterolateral (auscultatory triangle) longitudinal incision—discussion
Fractures of the posterior and posterolateral rib cage represent the second most common location and, in some ways, the most easily accessible. The patient may be positioned either in the prone or in the lateral decubitus position, depending on other factors such as presence of contralateral rib fractures, external fixators of the pelvis or extremities, spinal injuries, etc. If the patient has ipsilateral fractures anteriorly, with or without flail, that may require fixation, the recommendation is to position the patient in the lateral decubitus in order to access both anterior and posterior fractures without repositioning. As in fractures of the anterolateral ribcage, the ideal incision overlies the majority of the fractures needing reduction.
Once the precise location of the fractures is identified and the incision is made, the superficial aspect of the thoracic musculature is exposed by elevating adequate skin flaps. The auscultatory triangle has heretofore been the darling of medical internists teaching medical students the optimal location to auscultate the lungs. Surgeons operating on the posterolateral or posterior chest wall have rediscovered it for a different purpose. It is defined by the inferolateral border of the trapezius, the superior border of the latissimus, and the inferomedial borders of the scapula and rhomboid major. There exists here a small gap in the muscular carapace of the thorax that can be easily exploited by the surgeon seeking access to the thoracic wall. After dissecting through the loose connective tissue at the center of the triangle, finger dissection is used to open the space between the musculature and the rib cage proper. Taking care not to injure oneself on the fragments of broken rib, the fractures are located by palpation and the approach strategy is considered. This approach is ideal for ribs 4–9 fractured between the angle of the rib and the posterior axillary line. Simple retraction of the muscular boundaries of the auscultatory triangle will suffice for many of the fractures in this area with modern minimally-invasive tools such as percutaneous and right-angle instruments. However, fractures that are more cephalad or caudad may require either partial division or splitting of the overlying muscles (Figure 6). It must be reiterated that location of the skin incision dictates to where the operative field can be shifted. Muscles can be divided or split and retracted to expose the ribcage, but the skin of the upper back can often resemble the scalp in its inelasticity and lack of compliance, particularly in the young and persons with larger BMI. I have found that larger incisions are often necessary in order to retract and elevate the myocutaneous flaps that permit placing osteosynthesis plates.
Current rib fixation technology manufacturers emphasize the need for adequate hardware fixation on either side of the fracture—that is, there must be sufficient healthy, unfractured bone to take a minimum number of fixation screws to minimize the chances of hardware failure. While each manufacturer has a slightly different classification of what is an appropriate length, the surgeon must ultimately determine what fracture locations are out of bounds for fixation.
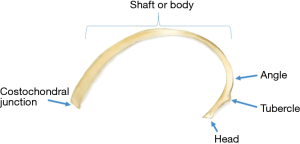
Although body shapes and sizes vary widely, one anatomical landmark that is quite reliable is the angle of the rib. This is the location of the rib where its curvature ends posterolaterally and it angles anteriorly to articulate with the thoracic vertebrae (Figure 7). It is also the lateral border of the attachments of the paraspinous muscles and marks where the ribs lose their flattened profiles and become relatively narrow and round. The distance between the angle of the rib and its vertebral attachment is barely the minimum length required to safely fixate utilizing hardware from most major instrument manufacturers. Thus, the angle of the rib marks the medial-most boundary for the location of “fixable” ribs. Fractures medial to the angle are typically deemed inoperable although some surgeons have had success affixing plates to the transverse process and lateral mass of the vertebra (private correspondence).
It is my opinion that, given the presence of nerves, nerve roots and the spinal cord itself, fixation of hardware medial to the rib proper be avoided altogether in order to safeguard these structures from direct or indirect injury. While the benefits of rib fixation remain somewhat controversial and indications are still being developed, at minimum surgeons must abide by the first principle of the Hippocratic Oath, “primum non nocere,” and avoid such a surgical misadventure at all costs.
Subscapular approach
Surgical approach
- Incise along the medial aspect of the scapula in a curvilinear fashion to the scapular tip;
- Elevate skin edges to expose the auscultatory triangle;
- Sharply dissect through loose connective tissue in the gap between the borders of the triangle;
- Perform a finger sweep maneuver to bluntly dissect and elevate trapezius, latissimus, and scapula off of the underlying ribcage;
- Partial division of the trapezius superiorly and/or latissimus inferiorly may be necessary.
Subscapular approach—discussion
Among the most challenging fractures to treat are those of the upper posterior and posterolateral ribcage. The scapula is a major obstacle when it comes to fixing ribs 2–5 posterolaterally, one that has only recently been partly overcome thanks to instrument innovation. Due to the thick musculature of the upper posterior chest, particularly in young males who represent the majority of trauma victims, percutaneous approaches are rarely feasible. The preferred approach is a modified posterolateral thoracotomy incision, one that curves along the inferior and medial borders of the scapula and allows elevation of the scapula to access the ribcage beneath. Depending on the location of the fractures, partial division of the trapezius and/or latissimus muscles may be required. As with the posterolateral approach, the recommendation is to enter the auscultatory triangle and elevate the muscles from the ribcage first, then locate by blind palpation the position of the fractured ribs prior to engaging in extensive muscle division. The surgeon can then determine how much, if any, of the trapezius/rhomboid complex needs to be divided to access the fractured ribs. We have found it often necessary to divide part of trapezius rather than perform the fixation using a muscle-splitting technique because sufficient retraction of the scapula may not be possible without releasing some of its muscular attachments.
Positioning of the patient for this approach is another challenge. The natural range of motion of the upper extremity will determine the range of motion of the scapula as well. Full abduction of the upper extremity such as when the patient is in the prone position will limit the extent to which the scapula can be elevated off the chest wall. Therefore, the lateral decubitus position is recommended in this case to gain full access to the subscapular region by distracting the scapula away from the chest wall. Some advocate prepping the entire ipsilateral extremity into the surgical field in order to mobilize it intraoperatively and thus exploit the scapular range of motion in order to expand the access to the region, particularly when fixing combined posterior and anterior rib fractures (8,9).
General considerations
Orthodoxy comes from a combination of the Greek terms: “ortho” meaning straight and “doxy” meaning opinion. Thus, orthodoxy means straight or sound opinion or way of thinking. The opposite is generally termed “un-orthodoxy,” or downright “heresy,” which means to go against established doctrine. We are on the cusp of what may become, assuming that further studies demonstrate its benefit, the emergence of surgical rib fixation as mainstream treatment of severe chest wall injuries. Until this practice is widely accepted, this general approach will remain un-orthodox and perhaps even a little bit heretical to some. It is likewise with the actual technical approach to the injured chest wall segments. The standard thoracotomy incision is, to many surgeons, the only acceptable method to incise the chest even though the surgical goals for which we learned to perform this procedure were vastly different. In training, the standard horizontal anterolateral, posterolateral or full thoracotomy incision overlying the 4th/5th intercostal space was the well-worn path to all of the major structures of the thoracic cavity and, therefore, presumed to be adequate for the chest wall as well. It only took a couple of challenging high or low rib fractures for most of us to realize that these approaches were not adequate for fixation of all but a few of the fracture patterns with which our patients present. This is because, while the anterolateral ribs 4–8 are the most commonly broken and are amply exposed with this approach, they are rarely the only ribs broken in a patient who is a candidate for rib fixation.
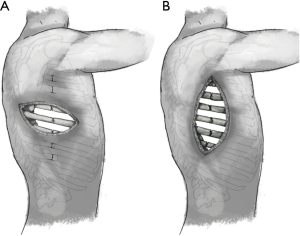
Gasparri and colleagues have advocated the use of the standard posterolateral thoracotomy for the repair of most fractures in their cohort; however, they admit that in order to achieve this, it is necessary to divide the latissimus, trapezius, and rhomboid muscles, which likely adds a considerable degree of perioperative morbidity (11). And so, unorthodox though it may be, selecting the incision that best exposes all of the actual fractures themselves is the key. In the case of more than four ribs broken in a line, anything other than an overlying parallel incision would render all but the most central fractures virtually inaccessible (Figure 8).
Careful preoperative mapping and rechecking surface anatomical landmarks is essential. Of special note is the use of the 3-dimensional reconstruction feature now available in all modern radiographic software packages in order to fully understand the fracture patterns and how best to approach each one. Examining CT imaging one slice at a time only conveys a part of the story and makes mapping according to surface landmarks infinitely more challenging. For that reason, as a standing protocol, the radiology department in our hospital routinely makes 3-dimensional reconstructions of the chest wall both with and without the presence of the scapula (Figure 9). By examining the model without the scapula, the surgeon can more thoroughly assess the number and precise location of displaced fractures. Adding the scapula allows one to locate them on the patient’s chest wall based on the surface anatomy. The scapula is the key landmark to utilize in gauging the location of fractures in the majority of cases where the severity of the displacement affords actual palpation of the fracture lines. One caveat is that the scapula shifts significantly relative to the chest wall such that its position may vary by several centimeters. It is imperative, therefore, that the surgeon identify the precise position of the upper extremities during the CT scan and utilize that information to guide positioning on the OR table. By recreating the position of the upper extremity in the operating room, the surgeon may then use the scapular tip to identify the relative position of the fractures.
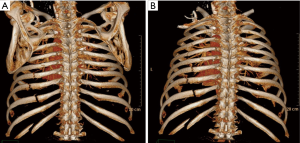
Once the accurate position of the scapula is recognized, longitudinal and horizontal mapping can take place. The surgeon can use the thoracic spinous processes and the scapular tip, all the while referencing the CT scan images, in order to identify the position of posterior and posterolateral fractures. The scapular tip and the nipple, the inferior pectoral groove, and lateral border of the sternum are frequently used surface landmarks.
Some surgeons have advocated for performing preoperative thoracoscopy in order to aid in identifying the location of rib fractures. I do not find it necessary to perform routinely but we recognize it as another tool that may be useful to some surgeons, particularly where thoracoscopy is otherwise already indicated.
On occasion, severely displaced fractures can be palpable. This is typical where severe displacement of the fractures has occurred and when body habitus allows. However, care must be taken as normal anatomical features may be mistaken for displaced fractures. For example, the insertion of the serratus anterior on the anterolateral ribs, the angle of the rib posteriorly where paraspinal muscles attach, and the costochondral junction particularly when calcified and hypertrophic, can all resemble displaced fractures to the touch. Gentle pressure can at times confirm that the area in question is a displaced fracture; but, once again, overall chest wall instability can be misleading and a surgeon should never rely on palpation of the chest wall alone to plan the surgical incision. Ultimately, the carpenter’s motto of “measure thrice, cut once” is the best practice.
Comments
A 2009 survey of surgeons who treated patients with rib fractures suggested that the majority of trauma surgeons believed that SSRF was a necessary component of care for some patients with severe crush injuries of the chest wall (12). Interestingly, the same surgeons felt themselves unable to perform this procedure with their current level of training on the technique. This paper seeks to add to the body of literature an additional technical reference for accessing the chest wall that may aid those seeking some guidance early in their experiential curve.
While most rib fractures that lead to significant disability and warrant surgical fixation are accessible utilizing one of these three approaches, there remain fractures of the high posterior and high anterior thorax that are significantly more challenging to access. Although approaches to these types of fractures have not been covered here, the basic principles of approach can be applied: incise over the fractures present, split muscles where possible, and utilize natural gaps in the muscular thorax while avoiding damage to essential nerves due to division or retraction. Applying these principles should allow the surgeon to gain access to the bones of the thorax in order to stabilize a disabling injury of the ribcage.
Although fixation of only one fracture line of a flail chest has been described as a successful method of treatment, it is better to attempt that both fractures of a flail segment be fixed whenever feasible. Marasco et al. found that, in their cohort, surgical fixation of only one fracture line was necessary in order to affect stabilization (13). They noted that patients who underwent single fracture fixation, effectively converting a flail segment into a simple fracture, had similar outcomes to those who had both fractures fixed. The authors have more recently noted that, particularly with posterior fractures left unreduced, some fractures continue to displace over time despite overall improved stability (10). Therefore, wherever possible, all fractures that potentially contribute to chest wall instability should be fixed. Ultimately, however, it may be feasible to leave one fracture line un-reduced when it becomes especially challenging due to either anatomic location, intraoperative patient instability, challenges positioning the patient, or undesirable cosmetic outcome of the necessary incision. Furthermore, this question highlights the current lack of understanding of chest wall mechanics and absence of quantifiable measures of dynamic chest wall instability in actual living patients.
One fracture pattern not covered here is that of the anterior ribcage encompassing the cartilaginous portion. Cartilage comprises the majority of the anterior rib cage from the lateral border of the sternum to the mid clavicular line and the entire inferomedial border. Cartilage behaves very differently from bone in many respects and many authors advocate not applying hardware directly to this area. Rather, any fixation involving this portion of the rib should receive hardware that spans the entire length of the cartilage and is anchored securely from bony rib to bony sternum (10). Cartilage is also unable to heal, being a largely avascular tissue, and fractures of this area are prone to result in nonunion (14). Other authors have reported successful fixation of costal cartilage fractures, but this technique has not been validated with sufficient published cohort studies (15). The costal margin is further problematic as it is the anterior attachment site of the diaphragm, and costal margin rupture with traumatic diaphragmatic hernia is a particularly challenging injury that requires technical approaches beyond what can be covered in this paper.
Other technical aspects of surgical fixation not covered here, such as bridging gaps in the ribcage, ideal positioning of the screws in anterior plate fixation, utilizing the principle of osteosynthesis, stress shielding, and using bioprosthetic agents to promote healing may need to be examined closely by the surgeon attempting surgical fixation, particularly when starting out on this surgical endeavor in their practice. Ultimately, the best resource is a surgeon who has had ample experience with this type of operation, whether that surgeon practices within one’s institution, at a neighboring facility, or who can be consulted remotely for advice.
Lastly, while surgical fixation has garnered the attention of surgeons around the world as a potentially crucial modality for treating severe injuries of the ribcage, these techniques should be only a small part of the surgeon’s armamentarium for the treatment of patients with destabilized ribcage injuries. As with other types of injury and disease, the most successful approach is one that utilizes multidisciplinary care in order to produce the desired outcomes (16). Multimodal pain control, including regional anesthetics as well as systemic analgesics, rehabilitation and physical therapy, respiratory therapy and pulmonary hygiene, and long-term outpatient follow up are necessary to have the desired impact on this disease entity in our patients. Surgical fixation is only one of the many tools that a system of care can offer patients suffering from this often deadly, frequently debilitating type of injury.
Acknowledgements
Special thanks to Drs. Richard Whitworth and William Schwarz for their mentorship and support.
Footnote
Conflicts of Interest: P Greiffenstein has served as a paid consultant for product development for DuPuy Synthes, KLS Martin and Zimmer Biomet and has also served as lead instructor for surgical skills lab for Zimmer Biomet. The other authors have no conflicts of interest to declare.
References
- de Moya M, Nirula R, Biffl W. Rib fixation: Who, What, When? Trauma Surg Acute Care Open 2017;2:e000059. [Crossref] [PubMed]
- Butensky AM, Gruss LP, Gleit ZL. Flank pseudohernia following posterior rib fracture: a case report. J Med Case Rep 2016;10:273. [Crossref] [PubMed]
- Marr AB, Stuke LE, Greiffenstein P. Kinematics. In: Moore EE, Feliciano DV, Mattox KL, editors. Trauma, 8th edition. McGraw Hill Education, 2017:3-20.
- Borrelly J, Aazami MH. New insights into the pathophysiology of flail segment: the implications of anterior serratus muscle in parietal failure. Eur J Cardiothorac Surg 2005;28:742-9. [Crossref] [PubMed]
- Gray H. Anatomy, Descriptive and Surgical. Lea Brothers & Co, 1858:767-8.
- Martin RM, Fish DE. Scapular winging: anatomical review, diagnosis, and treatments. Curr Rev Musculoskelet Med 2008;1:1-11. [Crossref] [PubMed]
- Skedros JG, Mears CS, Langston TD, et al. Medial scapular winging associated with rib fractures and plating corrected with pectoralis major transfer. Int J Surg Case Rep 2014;5:750-3. [Crossref] [PubMed]
- Schulz-Drost S, Grupp S, Pachowsky M, et al. Stabilization of flail chest injuries: minimized approach techniques to treat the core of instability. Eur J Trauma Emerg Surg 2017;43:169-78. [Crossref] [PubMed]
- Nauth A. Surgical approaches for rib fracture fixation. In: McKee MD, Schemitsch EH. editors. Injuries to the Chest Wall. Springer International Publishing, 2015:81-8.
- Marasco S, Saxena P. Surgical rib fixation - technical aspects. Injury 2015;46:929-32. [Crossref] [PubMed]
- Gasparri MG, Tisol WB, Haasler GB. Rib stabilization: lessons learned. Eur J Trauma Emerg Surg 2010;36:435-40. [Crossref] [PubMed]
- Mayberry JC, Ham LB, Schipper PH, et al. Surveyed opinion of American trauma, orthopedic, and thoracic surgeons on rib and sternal fracture repair. J Trauma 2009;66:875-9. [Crossref] [PubMed]
- Marasco S, Liew S, Edwards E, et al. Analysis of bone healing in flail chest injury: do we need to fix both fractures per rib? J Trauma Acute Care Surg 2014;77:452-8. [Crossref] [PubMed]
- Sollender GE, White TW, Pieracci FM. Fracture of the Costal Cartilage: Presentation, Diagnosis, and Management. Ann Thorac Surg 2018. [Epub ahead of print].
- Pharaon SK, Schoch S, Marchand L, et al. Orthopaedic traumatology: fundamental principles and current controversies for the acute care surgeon. Trauma Surg Acute Care Open 2018;3:e000117. [Crossref] [PubMed]
- Todd SR, McNally MM, Holcomb JB, et al. A multidisciplinary clinical pathway decreases rib fracture-associated infectious morbidity and mortality in high-risk trauma patients. Am J Surg 2006;192:806-11. [Crossref] [PubMed]