
Comparison of costs of hospitalization of patients with primary lung cancer after lobectomy with access through classic thoracotomy and VATS in the conditions of financing based on diagnosis-related groups
Introduction
One of the major problems that can be encountered in the management of health care units is the need to rationally dispose of limited financial resources for health care. The solution to this problem should be selecting the best for the patient, and at the same time viable, cost-effective solutions in diagnosis and treatment. Paradoxically, it often turns out that a high standard of medical services promotes reduction of costs of health care provided to a patient who once effectively cured does not generate long-term care costs, additional treatment due to complications, financial losses caused by long-term sick leave.
It is not unusual that the same goal in surgery can be achieved with the help of recognized traditional methods as well as modern, less invasive methods. In this case, the choice of the surgical technique should be made based on the patient’s best interest, not only on financial factors. Lobectomy is an example of such a procedure in patients with non-small cell lung cancer. This operation can be performed both via traditional access—thoracotomy or a minimally invasive method—video-assisted thoracoscopic surgery (VATS). Numerous scientific reports prove that the quality of life of patients is higher when minimally invasive methods had been used (1,2). On the other hand, the cost of operation via VATS access is higher than using the classical method (3,4), which inclines hospital managers to impose restrictions on use of VATS—especially since lobectomy tariff valuation offered by the institutional payer (in Poland by the National Health Fund—NFZ) is the same regardless of the operating technique used (5).
A constant development of medicine forces the necessity of consistent verification and updating of medical procedures offered by the national payer and their comparison with real costs of treatment. This also applies to the creation of new pricing for emerging precursory diagnostic and therapeutic methods. This objective can be achieved by cost-effectiveness analysis which is a tool serving to compare costs and gains of new and traditional medical procedures (6). An appropriate valuation of medical services determines access to health care which should always be at the highest possible level.
Objective of the work
Differences in surgical technique and well-being of patients who underwent lobectomy via thoracotomy and VATS were an incentive to conduct the research presented below. These differences concern both duration of the procedure, equipment necessary to carry out the procedure, period of hospitalization after surgery and the quality of life of patients, including the tempo of recovering. All these factors distinguishing one surgical technique from another prompted the authors to verify whether the same cost of the tariff valuation of this medical procedure offered by the NFZ is justified. Due to the lack of publications on this subject so far, we decided to determine whether the cost of a health service, which includes lobectomy varies significantly depending on the surgical access used.
The main aim of the study is to compare cost-effectiveness of hospitalization in patients with lung cancer after lobectomy via traditional and minimally invasive access. To achieve this goal, three specific research objectives have been distinguished:
- Calculation of the average cost of lobectomy via thoracotomy and VATS in Polish setting;
- Estimation of the average cost of hospitalization of a patient undergoing lobectomy via thoracotomy and VATS;
- Comparison of the actual costs of hospitalization of patients after lobectomy via thoracotomy and VATS access with its current pricing offered by national payer (NFZ).
Methods
We performed a retrospective analysis of medical records of patients hospitalized in the Department of Thoracic Surgery, General and Oncological Surgery, USK WAM in Lodz in 2017 due to non-small cell lung cancer, in whom lobectomy via VATS thoracotomy has been performed. The study group consisted of a total of 70 patients in whom the medical documentation was complete and allowed to get all the data necessary for analysis. An obvious limitation of this study are criteria of selection to both groups. Type of access depended mostly on the operator’s preferences and was only slightly influenced by TNM—patients with tumors bigger in diameter than 4 cm undergone thoracotomy, patients with smaller tumors were operated by VATS access if the operator was skilled in VATS or by thoracotomy if the operator was more comfortable in this access. Patients who needed conversion to thoracotomy or extended lobectomy or patients with comorbidities affecting the operation process (as for example empyema forcing decortication simultaneous to lobectomy) were excluded from the analysis. Concerning patients’ characteristics, inclusion condition was resectable non-small cell lung cancer, with no induction chemotherapy or other neoplastic disease history. To keep the study group homogenous, severe complication requiring ICU stay or prolonged ventilation was an exclusion criterion. Longer hospitalization reasons, if mild, for example air-leak, chronic disease aggravation or anemia did not exclude the patient from study. Referring to length of hospitalization it is important to note that there is no local standard referring to discharge conditions. However, the fastest possible discharge is preferred. When only there is no air-leak and there is confirmation of lung expansion, the patient is discharged. The discharge may be influenced only by deterioration of patient’s general state, e.g., severe pain, cardiac or respiratory distress but no non-medical factors were taken into consideration—patients were discharged any day of the week, also during the weekend.
The collected data were used only in collective summaries, while maintaining full anonymity of patients and referring to this Ethics Approval was not necessary. Approval of Hospital Administration concerning use of medical data was assessed. Patients who were diagnosed with tumors other than non-small cell lung cancer or benign tumors on the basis of histopathological examination and patients who had to convert from VATS to thoracotomy were excluded from the study.
On the basis of clinical data obtained from the medical records of the study group and based on financial data obtained from financial department of the hospital, a database containing key information grouped into 3 blocks was built in the Microsoft Excel spreadsheet: patient demographic data (age and gender), data concerning the procedure (including: type of access, duration of the procedure, type of lobectomy, number and types of disposable equipment used, consumption of hemostatic agents and blood preparations), as well as data on hospitalization, e.g., duration of hospitalization and the number of medicines administered to the patient. On this basis costs of procedures and costs of hospitalization were calculated.
All medical records were matched with financial data obtained from the hospital's financial department, which resulted in the following calculations for each patient: man-day cost per person (taking into account the costs of: food, accommodation, washing hospital underwear, doctor's and nursing staff's fees, depreciation of hospital equipment—both in ward as well as on the operating block, fees for utilities, sewerage, management costs), the cost of medicines given to the patient in the ward (based on data from the department’s settlement with the hospital pharmacy), the cost of the operation dependent on its duration (including: remuneration of operators, scrub nurses, anesthesiologist and nurse anesthetist, equipment used for surgery, equipment used for anesthesia, drugs administered in the operating theatre, sterilization of reusable equipment), and finally total hospital cost (consisting of: number of man-days x cost per person, cost of surgery, cost and list of drugs administered in the ward). Post-discharge cost was not considered in this study.
Based on the obtained data, the following calculations were made: the average duration of the procedure and the time of hospitalization depending on the access used, the average cost of the procedure depending on the surgical access and the average cost of hospitalization in both groups. The obtained results were subjected to statistical analysis using the U Mann Whitney test provided by Statistica 13 software. The statistical significance was considered to be P<0.05.
Results
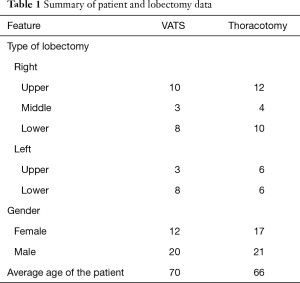
Data from 70 patients were used for the analysis, of which 38 were lobectomy via thoracotomy, while the remaining 32 were operated via VATS. A summary of demographic and anatomic data is presented in Table 1.
Full table
The presented data confirm that the choice of the access used was not dependent on the type of lobectomy, on the sex of the patient, or on his age. The average duration of surgery and hospitalization after surgery and the average cost of surgery and hospital stay, including one of the two surgical approaches, are presented in Table 2.

Full table
The difference in the duration of the operation for two different operational facilities proved to be irrelevant on the basis of the statistical analysis.
On the other hand, there were significant differences in terms of: the average time of post-operative stay in the hospital, which in case of thoracotomy was longer by 2.02 days on average (P=0.0000084) and in the average cost of surgery, which was higher via VATS by 4,399 PLN (€1,023) (P=0.0114). The average total cost of hospitalization of a patient operated via VATS was higher by 3,159 PLN (€735). Despite this significant difference in the costs of the entire hospitalization, depending on the access selected, it did not show statistical significance (P=0.05118).
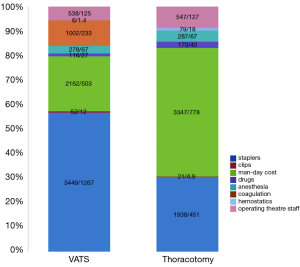
After comparing the proportion of costs that comprised the average cost of hospitalization of a patient undergoing lobectomy, it turned out that concerning VATS access the highest percentage of costs is related to the use of staplers necessary for minimally invasive lung resection. In patients undergoing lobectomy via thoracotomy, the largest part of the costs is related with the length of hospitalization itself. Furthermore, the cost of administered drugs was significantly higher in the group of patients subjected to thoracotomy (average €40 vs. €27 with P=0.0005). The proportion of particular costs in the cost of hospitalization is shown in Figure 1.
Discussion
The tariff valuation of medical procedures serves for the effective spending of funds for healthcare. The pricing of healthcare provision reimbursed by the NFZ is made in Poland by the Agency for Health Technology Assessment and Tariffs (7). However, such valuation is also necessary to set the prices of medical services performed by private doctors or clinics, it is the basis for invoicing patient or payer (e.g., an insurer) for treatment in line with actual costs, to set standards for treatment of patients with a particular disease, to group these diseases and medical procedures, and finally, it can be the basis for making decisions at the level of the board of the unit providing services in relation to the cost-effectiveness of this procedure, the economic use of material and human resources, and can be used to optimize the work of the ward or operating theatre in the case of surgical procedures (8).
Material cost is the key cost of a healthcare procedure. The cost of a healthcare service includes however not only the costs of medical procedures, but also other costs, especially those related to the time of hospitalization and used drugs. The proper identification and assessment of all types of costs that must be beard during medical procedure is essential for determining the actual price of health care service (9).
Some medical procedures can be carried out by various methods or techniques while achieving the same final result. Often, such differences concern procedures, where the same organ is removed via different ways or using different tools. Some of these differences have been included in the ICD-9 classification, for example, there is a distinction between laparoscopic and open cholecystectomy. Such a distinction has its consequences for the valuation of a given procedure, however, it was not included in the case of lobectomy via traditional and VATS access.
Our research gave an opportunity to assess the cost-effectiveness of lobectomy in patients with non-small cell lung cancer operated via two different accesses: traditional—thoracotomy and minimally invasive—VATS.
On the basis of our analysis, it was shown that patients who are operated via minimally invasive method are hospitalized after surgery significantly shorter with an average of 2 days. Shorter in-hospital stay was also observed in other studies (10), e.g., Farjah et al. observed in their study group lower percentage of longer than 14 days stay in patients after VATS procedures (11). The costs of the procedure carried out via VATS access are significantly higher than the cost of the same procedure performed via traditional access. As statistics show, even though the study group was small, this difference does not affect the overall cost of hospitalization. There are however studies performed on wider study groups in which cost of hospitalization in total is higher after thoracotomy than VATS. This is related to non-surgical costs of hospitalization, in particular high costs associated with a longer stay in the hospital (12) which was also confirmed in our study. Taking into account the results of this work and scientific reports on the benefits of minimally invasive procedures (1,13), it seems justified to state that patients in which early-stage disease allows for minimally invasive surgery should be operated in this way for several reasons. First, minimally invasive techniques result in significantly better post-operative quality of life, faster recover and faster access to possible further oncological treatment, and in the case of patients in working age—faster return to work. Secondly, significantly shorter hospitalization after minimally invasive surgery enables increase of the availability of hospital beds, especially for oncological patients. In Polish conditions regarding to unlimited funding of oncologic procedures by the domestic payer (NFZ) it allows them to undergo surgery earlier and to shorten the waiting time for complementary oncological treatment if required.
At the same time, the comparable cost of hospitalization of patients undergoing lobectomy via both accesses is an argument against the limitation of high-cost operations via VATS access, requiring appropriate equipment because the high cost of surgery in this case is balanced by shorter hospitalization and lower costs of treatment after surgery.
Under current conditions of financing medical procedures in Poland by the NFZ, a lobectomy procedure is valued at 22,930 PLN (€5,333). It means that regardless of the amount of instruments used for the operation, regardless of any complications involving additional costs and regardless of length of hospitalization NFZ pays this same amount both for VATS and classic lobectomy. Despite the lack of a statistically significant difference in the costs of hospitalization of patients undergoing lobectomy via VATS and thoracotomy, it seems that postulating a different pricing of costs of this procedure would be justified. Due to high material costs of VATS lobectomy, a possible higher valuation in the catalogue of procedures financed by the payer as compared to the lobectomy via thoracotomy, would encourage hospital managers to introduce minimally invasive procedures on a larger scale. This type of solution is already used in other procedures such as, for example, open and laparoscopic cholecystectomy.
Naturally, we are aware of many limitations of our research, especially that it concerns the conditions of financing in Poland and the assessment of costs of treatment within the limited framework of our center. Costs of hospitalization in Polish hospitals are lower than in other European countries, there is also a significant difference between costs of specialist equipment necessary for VATS procedures in different countries. This makes comparison of above-mentioned costs between Poland and other countries very difficult or even impossible. Therefore, possible assessment of the indications for separation of lobectomy tariffs via various accesses by a national payer should be based on in-depth studies on this subject analyzing the cost of treatment of larger groups of patients from different thoracic centers in Poland. While cost of hospitalization in Polish hospitals is cheaper, it could be also interesting to verify differences in short- and long-term quality of life of patients operated by VATS and thoracotomy in Poland comparing to other European countries.
Conclusions
- The cost of lobectomy via minimally invasive access is significantly higher than in the traditional thoracotomy, but is also associated with statistically significant shorter hospitalization time and similar duration of surgery.
- Despite high material costs of lobectomy via VATS, the total cost of hospitalization does not show a statistically significant difference in relation to traditional thoracotomy.
- Significantly shorter hospitalization time after VATS lobectomy allows to increase the availability of hospital beds for patients awaiting surgery due to lung cancer.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The collected data were used only in collective summaries, while maintaining full anonymity of patients and referring to this Ethics Approval was not necessary. Approval of Hospital Administration concerning use of medical data was assessed. Written informed consent from the patient was waived due to retrospective nature of this study.
References
- Bendixen M, Jørgensen OD, Kronborg C, et al. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol 2016;17:836-44. [Crossref] [PubMed]
- Zhao J, Zhao Y, Qiu T, et al. Quality of life and survival after II stage nonsmall cell carcinoma surgery: Video-assisted thoracic surgery versus thoracotomy lobectomy. Indian J Cancer 2015;52 Suppl 2:e130-3. [Crossref] [PubMed]
- Brunelli A. Cost analysis of VATS approaches. Video-assist Thorac Surg 2016;1:26. [Crossref]
- Fang HY, Hsiao FY, Huang HC, et al. Cost and effectiveness of video-assisted thoracoscopic surgery for clinical stage I non-small cell lung cancer: a population-based analysis. J Thorac Dis 2014;6:1690-6. [PubMed]
- Piwkowski C, Gabryel P, Gałęcki B, et al. High costs as a slow down factor of thoracoscopic lobectomy development in Poland - an institutional experience. Wideochir Inne Tech Maloinwazyjne 2013;8:334-41. [Crossref] [PubMed]
- Hill SR. Cost-effectiveness analysis for clinicians. BMC Med 2012;10:10. [Crossref] [PubMed]
- Development of Diagnosis Related Groups. Zasady rachunku kosztów. Access on: 4/03/2018. Available online: bpz.gov.pl/old/file/zasady%20JGP.pdf
- Jaworzyńska M. Wycena procedur medycznych w praktyce zakładów opieki zdrowotnej. Determinanty funkcjonowania podmiotów leczniczych w Polsce – nowe wyzwania., Wyd. UniwersytetuEkonomicznegowe Wrocławiu, Wrocław 2013:177-84.
- Rogowski W. Rachunek efektywności inwestycji. Wyzwania teorii i potrzeby praktyki, wyd. Nieoczywiste, Kraków, 2016:130.
- Casali G, Walker WS. Video-assisted thoracic surgery lobectomy: can we afford it?. Eur J Cardiothorac Surg 2009;35:423-8. [Crossref] [PubMed]
- Farjah F, Backhus LM, Varghese TK, et al. Ninety-day costs of video-assisted thoracic surgery versus open lobectomy for lung cancer. Ann Thorac Surg 2014;98:191-6. [Crossref] [PubMed]
- Lacin T, Swanson S. Current costs of video-assisted thoracic surgery (VATS) lobectomy. J Thorac Dis 2013;5 Suppl 3:S190-3. [PubMed]
- Shah RD, D'Amico TA. Modern impact of video assisted thoracic surgery. J Thorac Dis 2014;6:S631-6. [PubMed]


