|
Images of the Issue
Cardiac obstruction secondary to metastatic invasion - A rare
complication of Human Herpes Virus 8-positive plasmablastic
lymphoma in acquired immunodeficiency syndrome
Daniele Pádua1, Ana Clara Rodrigues1, Sérgio Barros1, Ana Lúcia Arruda1, Marianne Castro2, José Lázaro Andrade1
1Echocardiography Laboratory-InRad-University of São Paulo Medical School, São Paulo, Brazil; 2Division of Pathology-University of São Paulo Medical School, São Paulo, Brazil
Corresponding to: Daniele Pádua, MD. INRAD (Radiology Institute)-University of São Paulo Medical School, Av. Dr. Eneas de Carvalho Aguiar, 255, 05403-001, São Paulo-SP, Brazil. Tel: +55 (11) 2661 7067; Fax: +55 (11) 2661 7067. Email: danipadua@hotmail.com.
|
|
Abstract
Human herpes virus 8 (HHV8)-positive plasmablastic lymphoma (PBL) is a particularly rare and aggressive subtype of non-Hodgkin lymphoma, strongly associated with human immunodeficiency virus infection, with poor response to therapy and short survival. Characteristically, it shows proliferation of large plasmablastic cells with often eccentrically placed nuclei, with immunohistochemical assay positive for HHV8 latent nuclear antigen 1 and IgM. Primary mediastinal occurrence of a HHV8-positive PBL is rare and metastatic disease even more uncommon; tumor invasion to the heart leading to intracardiac obstruction with a rapidly fatal disease course has not been previously described.
Key words
Plasmablastic lymphoma; cardiac tumors; cardiac metastasis; non-Hodgkin lymphoma; cardiac obstruction J Thorac Dis 2012;4(4):425-427. DOI: 10.3978/j.issn.2072-1439.2012.01.02
|
|
Introduction
Human herpes virus 8 (HHV8)-positive plasmablastic lymphoma (PBL) is a rare subtype of non-Hodgkin lymphoma (NHL), strongly associated with human immunodeficiency virus (HIV), mainly involving lymph nodes with local invasion and rapid dissemination. They are highly aggressive, with poor response to therapy and short survival, with most patients dying within the first year of diagnosis ( 1). Primary mediastinal occurrence of PBL is unusual and invasion to the right and left heart chambers have not been reported so far.
|
|
Case report
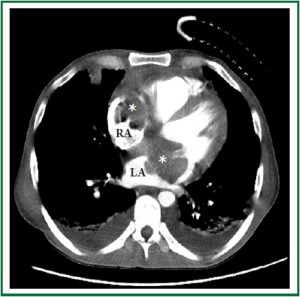
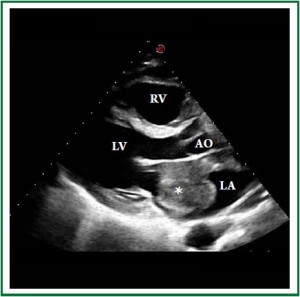
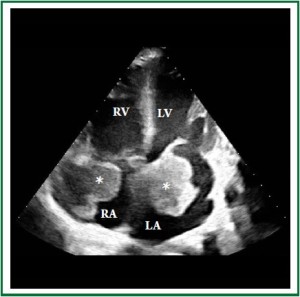
A 46-year-old Caucasian male was admitted to the emergency room with progressive dyspnea, lower limb edema and intermittent fever for 1 month. Past medical history included HIV infection for 20 years, with irregular highly active antiretroviral therapy (HAART) treatment. He had a history of smoking, alcoholism and cocaine addiction. On physical examination, the patient presented with a rapid respiratory rate, blood pressure of 118×68 mmHg and heart rate of 104 bpm. Laboratory data revealed hemoglobin concentration of 6.7 g/dl, white blood cell count of 3.600 /mm 3 and platelet count of 22.000 /mm 3, with a CD4 count of 49 cels /μl. Computed tomography demonstrated a large, infiltrative, solid mass involving the ascending aorta, pulmonary artery, right ventricle and both atria ( Figure 1 and Figure 2) with a lymph node conglomerate in the anterior mediastinum. Transthoracic echocardiography revealed biatrial dilation, mild left ventricular hypokinesia and severe right ventricular impairment. A large echodense mass with irregular borders filled almost completely the left atrium ( Figure 3), while another mass was observed inside the right atrium ( Figure 4), both attached to the interatrial septum. Increased transvalvular mitral and tricuspid gradients were observed by Doppler study. HAART was started along with intratechal methotrexate, followed by intravenous dexamethasone. Mediastinal biopsy revealed a HHV8-positive PBL. Tumoral cells showed positivity for immunohistochemical markers HHV8, MUM-1, CD138 (focal), CD20 (focal) and Ki67 (high index), whereas CD3 and Epstein-Barr virus (EBV) resulted negative. Bone marrow biopsy showed rare neoplastic cells, compatible with interstitial infiltration by HHV8-positive PBL. Chemotherapy with cyclophosphamide was started. A control echocardiogram after 3 days showed no tumor regression, but significant deterioration of systolic
ventricular function. The patient developed hemodynamic
instability and worsening of respiratory pattern, requiring
ventilatory and hemodynamic support. Despite therapy, the
patient died the following day.
|
|
Discussion
HIV infection is a well-known condition for neoplasm
development, with cancer diagnosis increasing more than 40%
in infected patients, contributing to approximately 30% of HIV-related deaths ( 2). HIV-associated lymphomas are highly
aggressive, characteristically occur at younger age and have a male
predominance. They are often associated with EBV and HHV8,
suggesting a role for these viruses in disease pathogenesis.
HHV8-positive plasmablastic lymphoma, however, is a rare
neoplastic lymphoprolipherative entity. The HHV8-infected
cells have a pre-plasma cell phenotype and a plasmacytic/
plasmablastic morphology, characterized by a proliferation of
larger plasmablastic cells with dense amphophilic cytoplasm and
vesicular, often eccentrically placed nuclei containing one or two
prominent nucleoli ( 1). The tumoral cells immunohistochemical
assay is positive for HHV8 latent nuclear antigen 1 and IgM,
with lambda light chain restriction. The markers CD20, MUM-1
and CD138 can be positive or negative, and EBV encoded RNA
is classically negative ( 3). Most reported cases of PBL associated
o HHV8 in HIV-positive patients were associated to multicenter
Castleman disease (MCD) ( 1, 4). HHV8-positive lymphoma
cells show the same phenotypic features as the plasmablasts
described in MCD, including cytoplasmic IgM expression and
lack of EBV infection, suggesting that the plasmablastic variant of
MCD could precede the development of frank HHV8-positive
lymphoma ( 4). These tumors were typically found in nodal
or splenic localization ( 5). The primary tumor described here
involved mediastinal lymph nodes, and most likely disseminated
locally, invading both atria. To the best of our knowledge, this is
the first reported case of a primary mediastinal HHV8- positive
PBL invading the heart. Treatment of HHV8-positive PBL is
not well established, with poorly defined therapeutic options;
treatment with systemic chemotherapy such as for standard
lymphoma has not improved prognosis. In this case, there was
poor response to chemotherapy, with progressive impairment
of ventricular function by tumor infiltration, resulting in cardiorespiratory failure, hemodynamic instability and death. HHV8-
positive PBL has an aggressive behavior and poor prognosis,
especially in HIV-infected individuals. Metastatic disease is rare,
may considerably affect outcome. Appropriate management of
the disease is uncertain. Abbreviations: HHV8=Human herpes virus 8; PBL=
plasmablastic lymphoma; NHL=non-Hodgkin lymphoma;
HIV=immunodeficiency virus; HAART=highly active
antiretroviral therapy; EBV=Epstein-Barr virus; AO=aorta;
LA=left atrium; LV=left ventricle; RA=right atrium; RV=right
ventricle; MCD=multicenter castlelman disease.
|
|
References
- Dupin N, Diss TL, Kellam P, Tulliez M, Du MQ, Sicard D, et al. HHV-8 is
associated with a plasmablastic variant of Castleman disease that is linked
to HHV-8-positive plasmablastic lymphoma. Blood 2000;95:1406-12.[LinkOut]
- Burgi A, Brodine S, Wegner S, Milazzo M, Wallace MR, Spooner K, et al.
Incidence and risk factors for the occurrence of non-AIDS-defining cancers
among human immunodeficiency virus-infected individuals. Cancer
2005;104:1505-11.[LinkOut]
- Campo E, Swerdlow SH, Harris NL, Pileri S, Stein H, Jaffe ES. The 2008
WHO classification of lymphoid neoplasms and beyond: evolving concepts
and practical applications. Blood 2011;117:5019-32.[LinkOut]
- Carbone A, Cesarman E, Spina M, Gloghini A, Schulz TF. HIV-associated
lymphomas and gamma-herpesviruses. Blood 2009;113:1213-24.[LinkOut]
- Oksenhendler E, Boulanger E, Galicier L, Du MQ, Dupin N, Diss TC,
et al. High incidence of Kaposi sarcoma-associated herpesvirus-related
non-Hodgkin lymphoma in patients with HIV infection and multicentric
Castleman disease. Blood 2002;99:2331-6.[LinkOut]
Cite this article as: Pádua D, Rodrigues AC, Barros S, Arruda AL, Castro M,
Andrade JL. Cardiac obstruction secondary to metastatic invasion - A rare
complication of Human Herpes Virus 8-positive plasmablastic lymphoma
in acquired immunodeficiency syndrome. J Thorac Dis 2012;4(4):425-427.
doi: 10.3978/j.issn.2072-1439.2012.01.02
|