
Gender differences in treatment strategies among patients ≥80 years old with non-ST-segment elevation myocardial infarction
Introduction
Myocardial infarction (MI) is the leading cause of death in the United States, and a major cause of mortality around the world (1). The good news is that the mortality of MI patients has considerably decreased worldwide, and this improvement has been considered to be correlated to improved treatment strategies during the last 20 years (2,3). However, these improvements are mainly reflected in young patients and males, while females with MI continue to have a high mortality rate and worse prognosis (4). In addition, previous studies have revealed that gender differences exist in the management of non-ST-segment elevation myocardial infarction (NSTEMI) (5,6).
Present guidelines recommend the use of an early invasive strategy for high-risk patients diagnosed with NSTEMI, regardless of age (7). Furthermore, given that 50% of MI patients have an onset age under 65 years old in the United States, the disease is not defined as “disease for the elderly”. However, elderly patients usually have high adverse events after invasive treatment, and the gender-related differences in mortality were found to be associated with age in both STEMI and NSTEMI patients (8,9). Furthermore, few studies have been reported on gender differences in treatment strategies for older patients with NSTEMI, especially for patients ≥80 years old.
In the present study, a retrospectively study was performed, which included NSTEMI patients ≥80 years old in Fuwai Hospital, in order to investigate the gender difference in treatment strategies and prognosis in China. It is hoped that the present study can provide guidance for clinicians in the decision-making of treatment strategies for NSTEMI patients ≥80 years old.
Methods
The present study included 190 consecutive patients ≥80 years old, who presented with NSTEMI in Fuwai Hospital from September 2014 to August 2017. The clinical diagnosis of NSTEMI was defined as patients who had angina pectoris at rest, ST-segment depression and T wave inversion by electrocardiogram at rest, and positive cardiac markers, including creatine kinase-MB or troponin I/T associated with NSTEMI within 24 hours after initial presentation. These patients were grouped by gender, and each group was stratified by treatment strategy. The invasive strategy included emergency percutaneous coronary intervention (PCI), emergency coronary angiography, emergency balloon dilatation, selective coronary angiography, and selective PCI. The treatment strategy was determined by the clinicians. The last follow-up day was July 31, 2018.
Aspirin and clopidogrel were used for antiplatelet treatment, while statin, beta-receptor-blocking agent, angiotensin-converting enzyme inhibitor (ACEI)/angiotensin receptor blocker (ARB) and diuretics were used, when needed. The patient’s basic information, medical history, discharge medications and prognosis conditions were collected and compared among patients who underwent invasive and conservative strategies. The relationship between mortality and treatment strategies in male and female patients were analyzed. The survival curves of treatment strategies with different genders were separately analyzed.
Statistical analysis
SAS software was used for the data analysis in the present study. Continuous variables were presented as mean ± standard deviation (SD). Normal distribution measurement data were analyzed by the Student’s t-test, while measurement data of skewness distribution were analyzed by rank-sum test. Categorical variables were analyzed by chi-square test. Logistic regression analysis was performed to compare the gender differences in mortality and treatment strategies. The survival curves of these two groups were compared by log-rank test in the Kaplan-Meier survival analysis.
Results
The clinical characteristics of patients are summarized in Table 1. Among the 190 NSTEMI patients ≥80 years old, 107 patients were male and 83 patients were female. In terms of basic information, there was a significant difference in age, creatinine, GRACE grade and Killip class between conservative and invasive strategies in female patients, while only GRACE grade was significantly different between these two treatment strategies in male patients (P<0.05). The medical history, including history of MI, after coronary artery bypass grafting (CABG), III grade, and renal dysfunction, was significantly different between the two treatment strategies in male patients, while the history of MI, diabetes mellitus, renal dysfunction, history of cerebral infarction, and anemia were significantly different between the two strategies in female patients (P<0.05). In addition, in terms of discharge medications, there was a significant difference in the use of diuretics between the two treatment strategies in male patients, while the use of aspirin and diuretics were significantly different between the two treatment strategies in female patients (P<0.05). In the prognostic analysis, death and good prognosis were significantly different between the conservative and invasive strategies in male patients (P<0.05), while there was no significant difference in prognosis in female patients who underwent conservative and invasive strategies (P>0.05).
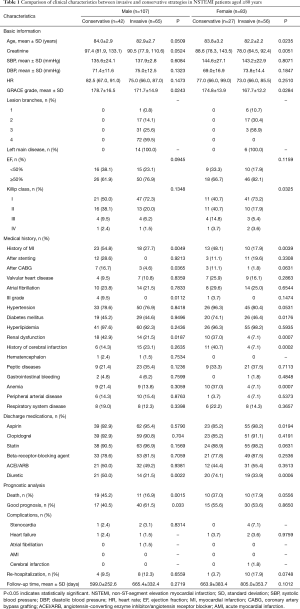
Full table
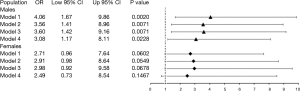
In logistic regression analysis of death and treatment strategies in NSTEMI patients ≥80 years old, the risk ratio was 4.06 [95% confidence interval (CI): 1.67–9.86] in males and 2.71 (95% CI: 0.96–7.64) in females. After adjusting for age, the risk ratio was 3.56 (95% CI: 1.41–8.96) in males and 2.91 (95% CI: 0.98–8.64) in females. After adjusting for age, hypertension, diabetes and hyperlipemia, the risk ratio was 3.60 (95% CI: 1.42–9.16) in males and 2.98 (95% CI: 0.92–9.58) in females. After adjusting for age, hypertension, diabetes, hyperlipemia, renal insufficiency and anemia, the risk ratio were 3.08 (95% CI: 1.17–8.11) in males and 2.49 (95% CI: 0.73–8.54) in females (Figure 1).
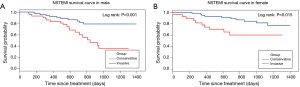
In the Kaplan-Meier survival analysis of survival probability and treatment strategies in NSTEMI patients ≥80 years old, the survival probability of invasive strategy was significantly higher than that of conservative strategy in males (P=0.001) and females (P=0.015) (Figure 2). The survival curve of invasive strategy in males and females were similar during the follow-up, while the lowest survival rate of conservative strategy decreased to approximately 0.35 in males, and approximately 0.6 in females. This indicates that the difference in treatment strategies in males was more pronounced than in females, in terms of long-term survival rate.
Discussion
Gender differences in treatment strategies for older patients, especially in patients over 80 years old remain unclear in China. In the present study, a retrospectively study was performed to investigate the gender difference in treatment strategies in NSTEMI patients ≥80 years old in China. The results revealed that good prognosis and death were significantly different between invasive and conservative strategies in males. Mortality was significantly correlated with treatment strategies in males in the multivariate logistic regression analysis. In addition, the survival probability of invasive strategy was significantly higher than that of conservative strategy in males and females during the follow-up, but the difference was more obvious in males, in terms of long-term survival probability.
It is noteworthy that gender differences exist in the underlying pathogenesis, clinical course, therapeutic approach and prognosis of NSTEMI (10,11). Women with NSTEMI usually have worse baseline characteristics, when compared to men (12,13). A published study revealed that the rate of adverse events, including death and bleeding, were different by gender in NSTEMI patients with a median age of under 68 years old (14). Although women with NSTEMI had worse baseline characteristics, their outcomes were comparable with those in men (15,16). In line with previous studies (17,18), it was found that women with NSTEMI were more likely to have comorbidities than men.
Previous studies have demonstrated that NSTEMI patients who were noninvasively managed had a greater risk for long-term mortality, and the decrease in mortality was associated with the use of an invasive strategy (19-21). In addition, the study conducted by Tegn et al. revealed that invasive strategy was superior for NSTEMI patients of 80 years old or older, when compared to conservative strategy (22). The present study demonstrated that NSTEMI male patients ≥80 years old, who were invasively treated, had a significantly lower death rate and better prognosis, when compared to patients conservatively treated, while these were no statistical difference for females. It was also found that the mortality of NSTEMI patients over 80 years old was significantly correlated to treatment strategies in male after adjusting for some characteristics, but not in females. This suggests that the invasive strategy is indeed superior to conservative strategy, in terms of death and prognosis in NSTEMI patients ≥80 years old, but gender difference was present.
In addition, the survival curve between invasive and conservative strategies were significantly different in both males and females ≥80 years old with NSTEMI during the follow-up period. However, the survival probability was not significantly different between these two treatment strategies in males and females during the 1-year following up. This is similar to the study conducted by Alabas et al., in which survival was not evident between males and females with NSTEMI in the 6-month and 1-year following up periods (23). The survival probability of invasive strategy decreased to approximately 0.8 and 0.75 during the following up in males and females, respectively, while the survival probability of conservative strategy decreased to approximately 0.4 and 0.6 during the following up in males and females, respectively. This indicates that the benefit of invasive strategy in males ≥80 years old with NSTEMI was certain in the long-term following up. This founding was verified by a previous study conducted by Alfredsson et al., in which men with NSTEMI could benefit from invasive strategy in the long-term follow-up (24). Although the difference in survival rate between invasive and conservative strategies was significant in males and females, the difference was more obvious in males in terms of long-term follow-ups. This indicates that clinicians may consider gender and clinical features when considering treatment strategies for patients ≥80 years old with NSTEMI, especially in males.
To our knowledge, the present study is the first time to investigate the gender difference in treatment strategies in NSTEMI patients ≥80 years old in China. The present study increases the confidence in a clinician’s choice of treatment strategy for NSTEMI patients ≥80 years old. Given the small number of NSTEMI patients over 80 years old in China, and that the present study was performed in only one center, the sample size may be not be sufficient. Hence, further studies should be performed in multi-centers with a larger sample size.
Conclusions
Gender differences exist in invasive and conservative strategies in NSTEMI patients ≥80 years old. Death is significantly associated with treatment strategies in males, but not in females. The survival curve was significantly different between these two treatment strategies in males and females, especially in males.
Acknowledgments
We thank all the subjects who participated in our study. We thank Key Laboratory of Cardiovascular Disease and National Center for Cardiovascular Diseases.
Footnote
Conflicts of Interest: The authors declare that they have no conflicts of interest.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. A written informed consent was obtained from each patient in the present study. The ethics approval for the present study was obtained from the Fuwai Hospital Health Human Research Ethics Committee.
References
- Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation 2014;129:e28-292. [PubMed]
- Radovanovic D, Seifert B, Roffi M, et al. Gender differences in the decrease of in-hospital mortality in patients with acute myocardial infarction during the last 20 years in Switzerland. Open Heart 2017;4:e000689. [Crossref] [PubMed]
- Radovanovic D, Erne P. Gender difference in the application of reperfusion therapy in patients with acute myocardial infarction. Cardiology 2009;114:164-6. [Crossref] [PubMed]
- Dégano IR, Subirana I, Fusco D, et al. Percutaneous coronary intervention reduces mortality in myocardial infarction patients with comorbidities: Implications for elderly patients with diabetes or kidney disease. Int J Cardiol 2017;249:83-9. [Crossref] [PubMed]
- Worrall-Carter L, McEvedy S, Wilson A, et al. Impact of comorbidities and gender on the use of coronary interventions in patients with high-risk non-ST-segment elevation acute coronary syndrome. Catheter Cardiovasc Interv 2016;87:E128-36. [Crossref] [PubMed]
- Donataccio MP, Puymirat E, Parapid B, et al. In-hospital outcomes and long-term mortality according to sex and management strategy in acute myocardial infarction. Insights from the French ST-elevation and non-ST-elevation Myocardial Infarction (FAST-MI) 2005 Registry. Int J Cardiol 2015;201:265-70. [Crossref] [PubMed]
- Jneid H, Anderson JL, Wright RS, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2012;60:645-81. [Crossref] [PubMed]
- Champney KP, Frederick PD, Bueno H, et al. The joint contribution of sex, age and type of myocardial infarction on hospital mortality following acute myocardial infarction. Heart 2009;95:895-9. [Crossref] [PubMed]
- Shah N, Kelly AM, Cox N, et al. Myocardial infarction in the "young": risk factors, presentation, management and prognosis. Heart Lung Circ 2016;25:955-60. [Crossref] [PubMed]
- Johnston N, Jönelid B, Christersson C, et al. Effect of gender on patients with ST-elevation and non-ST-elevation myocardial infarction without obstructive coronary artery disease. Am J Cardiol 2015;115:1661-6. [Crossref] [PubMed]
- Tavris D, Shoaibi A, Chen AY, et al. Gender differences in the treatment of non-ST-segment elevation myocardial infarction. Clin Cardiol 2010;33:99-103. [Crossref] [PubMed]
- Khera S, Kolte D, Gupta T, et al. Temporal trends and sex differences in revascularization and outcomes of ST-segment elevation myocardial infarction in younger adults in the United States. J Am Coll Cardiol 2015;66:1961-72. [Crossref] [PubMed]
- Udell JA, Koh M, Qiu F, et al. Outcomes of women and men with acute coronary syndrome treated with and without percutaneous coronary revascularization. J Am Heart Assoc 2017. [Crossref] [PubMed]
- Edmund Anstey D, Li S, Thomas L, et al. Race and sex differences in management and outcomes of patients after ST-elevation and non-ST-elevation myocardial infarct: results from the NCDR. Clin Cardiol 2016;39:585-95. [Crossref] [PubMed]
- Janion-Sadowska A, Sielski J, Gierlotka M, et al. Gender-related differences in clinical course, therapeutic approach and prognosis in patients with non-ST segment elevation myocardial infarction. Kardiol Pol 2011;69:784-92. [PubMed]
- Gupta T, Kolte D, Khera S, et al. Contemporary sex-based differences by age in presenting characteristics, use of an early invasive strategy, and inhospital mortality in patients with non-ST-segment-elevation myocardial infarction in the United States. Circ Cardiovasc Interv 2018;11:e005735. [Crossref] [PubMed]
- Lam CS, McEntegart M, Claggett B, et al. Sex differences in clinical characteristics and outcomes after myocardial infarction: insights from the Valsartan in Acute Myocardial Infarction Trial (VALIANT). Eur J Heart Fail 2015;17:301-12. [Crossref] [PubMed]
- Worrall-Carter L, McEvedy S, Wilson A, et al. Gender differences in presentation, coronary intervention, and outcomes of 28,985 acute coronary syndrome patients in Victoria, Australia. Womens Health Issues 2016;26:14-20. [Crossref] [PubMed]
- Blatt A, Kalmanovich E, Karny-Rahkovich O, et al. Comparison of noninvasively and invasively managed patients, with or without revascularization in non-ST elevation myocardial infarction (from the Acute Coronary Syndrome Israeli Survey). Am J Cardiol 2016;118:1-5. [Crossref] [PubMed]
- Hall M, Dondo TB, Yan AT, et al. Association of clinical factors and therapeutic strategies with improvements in survival following non-ST-elevation myocardial infarction, 2003-2013. JAMA 2016;316:1073-82. [Crossref] [PubMed]
- Gnanenthiran SR, Kritharides L, D’Souza M, et al. Revascularisation compared with initial medical therapy for non-ST-elevation acute coronary syndromes in the elderly: a meta-analysis. Heart 2017;103:1962-9. [PubMed]
- Tegn N, Abdelnoor M, Aaberge L, et al. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (after eighty study): an open-label randomised controlled trial. Lancet 2016;387:1057-65. [Crossref] [PubMed]
- Alabas OA, Gale CP, Hall M, et al. Sex Differences in treatments, relative survival, and excess mortality following acute myocardial infarction: national cohort study using the SWEDEHEART Registry. J Am Heart Assoc 2017. [Crossref] [PubMed]
- Alfredsson J, Clayton T, Damman P, et al. Impact of an invasive strategy on 5 years outcome in men and women with non-ST-segment elevation acute coronary syndromes. Am Heart J 2014;168:522-9. [Crossref] [PubMed]


