
Distribution of descending necrotizing mediastinitis and efficacy of distribution-specific drainage
Introduction
Descending necrotizing mediastinitis (DNM) resulting from oropharyngeal and cervical abscess is a life-threatening condition. The historical mortality rate of DNM has been reported to range from 23–51% (1-4). As surgical management without delay has been understood well as a key to cure the patients, the mortality rate has been decreased (11–17.5%) (5-7). However, because of the low incidence of DNM, details concerning the extension and distribution of the abscess to the mediastinum and appropriate drainage sites remain unclear.
Video-assisted thoracoscopic drainage has been recently applied for DNM, and its efficacy has been reported (8-11). Understanding the extension and distribution of thoracic abscesses may make distribution-specific thoracoscopic drainage possible.
We herein report our retrospective analysis of patients who underwent video-assisted thoracoscopic drainage for DNM. The purpose of this study was to evaluate the efficacy of distribution-specific thoracoscopic drainage. In addition, we suggest a new concept of mapping and classification of the thoracic abscess distribution of DNM and distribution-specific thoracoscopic drainage.
Methods
A retrospective review was conducted for seven patients who underwent thoracic drainage by thoracotomy or video-assisted thoracic surgery (VATS) for DNM at Aichi Medical University Hospital between November 2011 and March 2019. Clinical data were analyzed in the present study. The DNM diagnosis was made on the basis of criteria defined by Estrera et al. (12) in 1983. The detailed extension and distribution of the thoracic abscess was evaluated by computed tomography (CT), and DNM was classified according to Endo’s criteria as either type I (focal) mediastinitis (infection located in the superior mediastinal space, above tracheal bifurcation) or type II (diffuse) mediastinitis; type II mediastinitis was in turn subdivided into two subtypes of IIA (infection still located in the anterior inferior mediastinal space) and IIB (infection has reached the posterior inferior mediastinum) (13).
This study was approved by the Institutional Review Board of Aichi Medical University Hospital. The analyzed values are presented as the mean ± standard deviation.
Results
The clinical data of all seven patients are listed in Table 1. There were 5 men and 2 women with a median age of 61 years old (range, 40 to 91 years old). In 6 patients, underlying diseases that might influence the onset of DNM were present: diabetes mellitus (n=2), hypertension (n=2), alcoholic liver dysfunction (n=1), hemodialysis for renal failure (n=1), hyperlipemia (n=1), atrial fibrillation and brain infarction (n=1), traumatic brain contusion and higher-order dysfunction, (n=1), cardiac infarction (n=1) (with overlapping). The mean white blood cell (WBC) counts and C-reactive protein (CRP) immediately before drainage were 13,200±1,500/µL and 25.7±13.1 mg/dL, respectively. The DNM classification according to Endo’s criteria was type I (n=2), type IIA (n=1), type IIB (n=2) and unclassified type (n=2).
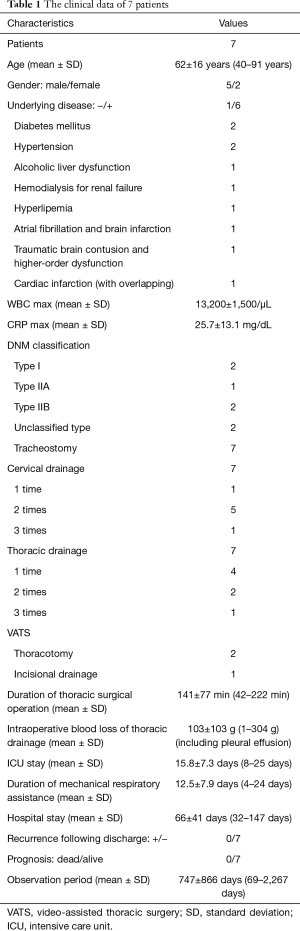
Full table
Cervical and thoracic drainage and tracheostomy were performed in all seven patients. Cervical drainage was performed 14 times for cervical abscesses, and thoracic drainage was performed 11 times for thoracic abscesses. Regarding thoracic drainage, thoracoscopic drainage was performed eight times, and thoracotomy was performed twice. Repeated drainages in three patients were performed because mediastinal abscess still existed after the previous operation or appeared newly in the different portions. In addition, incisional thoracic drainage for anterior thoracic abscesses was performed in one patient. Both cervical and thoracic drainage were needed a maximum of three times in one case. The operation time for thoracic drainage and intraoperative blood loss were 141±77 min (42–222 min) and 103±103 g (1–304 g), respectively.
Although there were no mortal cases or severe complications following drainage, surgical hemostasis was performed for postoperative bleeding in one patient. The mean hospital stay was 66±41 days. Laboratory data on inflammation parameters were almost normal by discharge (WBCs: 4,600±1,680/µL, CRP: 0.46±0.38 mg/dL). The mean observation period was 747±866 days. All patients are alive without recurrence.
Proposal of classification and map of thoracic abscess distribution
Thoracic abscesses of DNM are typically classified according to Endo’s criteria (13). However, in the present study, two patients had an unclassified type. Therefore, we propose a new classification and mapping system for thoracic abscess distribution referred to the International Thymic Malignancy Interest Group (ITMIG) mediastinal compartment (14). We have outlined nine categories of distribution based on the differences in incision sites for drainage, including the anterior thoracic wall, as shown in Figures 1,2, based on the CT and intraoperative findings:
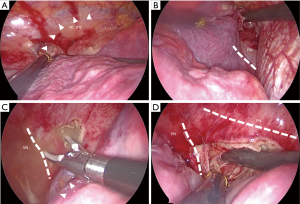
- Upper portion of the anterior compartment (UA): the cervical abscess extends to the anterior mediastinum along the sternum. Abscesses of the UA are usually drained via the cervical approach. However, residual abscesses can be drained by VATS. The internal thoracic vein is a milestone for UA abscesses, and the proximal pleura of the internal thoracic vein should be opened for drainage;
- Lower portion of the anterior compartment (LA): abscesses of the UA often extend to the lower portion of the anterior mediastinum. The distal pleura of the internal thoracic vein along the sternum and/or the phrenic nerve should be opened for drainage (Figure 3A,B);
- Right upper portion of the middle compartment (RU): when cervical abscesses extend to the mediastinum, they do not always pass in front of the thymus. When they extend behind or on the lateral sides of the thymus, the abscesses appear in the right upper portion of the middle mediastinum. For thoracic drainage of RU abscesses, the azygos vein is a milestone, and the proximal pleura of the azygos vein along the right vagus nerve and/or the right brachiocephalic vein should be opened for drainage (Figure 3C,D);
- Right middle portion of the middle compartment (RM): RU abscesses sometimes extend to more distal areas around the right hilum. For drainage of RM abscess, the pleura around the right hilum should be opened;
- Right lower portion of the middle compartment (RL): RM abscesses sometimes extend to more distal areas beyond the right hilum along the esophagus. The pleura around the inferior pulmonary vein or pulmonary ligament along the esophagus should be opened for drainage;
- Left upper portion of the middle compartment (LU): for drainage of LU abscesses, the aortic arch and the subclavian artery are milestones, and the distal pleura of the aortic arch along the subclavian artery should be opened for drainage;
- Left middle portion of the middle compartment (LM): LU abscesses may extend to the more distal mediastinum around the left hilum. They may extend from LA abscesses. For drainage of LM abscesses, the pleura around the left hilum should be opened;
- Light lower portion of the middle compartment (LL): LM abscesses may extend to more distal areas beyond the left hilum. The pleura around the inferior pulmonary vein or pulmonary ligament along the esophagus should be opened for drainage;
- Anterior thoracic wall (AT): we experienced extension of UA abscesses to the anterior thoracic wall. For percutaneous drainage of such abscesses, the skin should be incised just above the abscess.
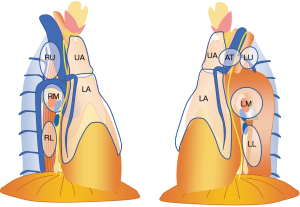
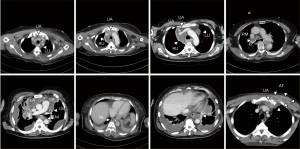
The frequency of the abscess distribution for each category is shown in Table 2. The frequency of abscesses accompanying DNM gradually descends from the neck toward the lower mediastinum. However, abscesses are not necessarily continuous, and skipped lesions are occasionally noted.
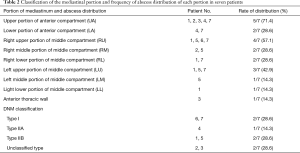
Full table
Discussion
We investigated the patients with DNM who underwent surgical drainage for thoracic abscess and suggest a new mapping and classification system for the thoracic abscess distribution and distribution-specific drainage. As oropharyngeal and/or cervical abscess usually precedes DNM, we collaborate with head and neck surgeons. As the historical mortality rate of DNM has been high (1-4), DNM is well known to be a life-threatening condition. Prompt surgical management is understood to be the key to curing patients, and the mortality rate has been decreased with this approach (5,6,15). However, because of the low incidence of DNM, the details concerning the extension and distribution of abscesses to the mediastinum and appropriate approaches for drainage remain unclear.
Open thoracotomy and extensive mediastinal pleural incision with extensive debridement have been performed as the principal treatment and selected to achieve a cure in patients with DNM. While the efficacy has been suitably demonstrated, bilateral open thoracotomy might be more invasive for DMN patients than VATS drainage. VATS drainage has recently been applied for DNM, and its efficacy has been reported (8-11). To rescue critical patients, this minimally invasive drainage may be an ideal approach. As DNM lesions do not necessarily spread and extend throughout the mediastinum, distribution-specific drainage with VATS techniques may be useful. We were able to cure all of the patients who underwent VATS drainage in the present study. This minimally invasive drainage can be repeated if necessary. Three of the seven cases in the present study underwent repeated VATS drainage to cure their DNM completely because mediastinal abscess still existed after the previous operation or appeared newly in the different portions. While the detailed data were not shown, the operation time for drainage after the first attempt was reduced on subsequent drainage attempts. It is important to know the exact location of the abscess in order to perform appropriate drainage. We therefore suggest a new mapping and classification system for the thoracic abscess distribution using CT findings and distribution-specific drainage.
Regarding the distribution of DNM, Endo et al. classified DNM into types I and II (13). Type II mediastinitis was further subdivided into two subtypes (IIA and IIB). However, we experienced cases that were difficult to classify based on these conventional categories. In our experience, the distribution of the abscess was not continuous, with isolated lesions sometimes scattered about. Drainage of all lesions is necessary to achieve complete treatment. We therefore suggested a map of mediastinal abscesses of DNM that was divided into nine categories. The location of the mediastinal pleural incision or skin incision was different in none categories as stated above.
We have referred ITMIG definition of the mediastinal compartment for mapping of the distribution of the mediastinal abscess. The ITMIG classification includes three compartments, the prevascular (anterior), visceral (middle), and paravertebral (posterior) compartments. It does not adapt superior mediastinal compartment (or mediastinum). The DNM descends from oropharyngeal and cervical abscess and it can extend to any directions (15). The mediastinal incision sites for drainage varies depending on the direction of the extension even in the superior compartment. While the mediastinum is a continuum, we recognize anatomical barriers to complete the mediastinal drainage. Typical barriers include the azygos vein, internal thoracic veins and phrenic nerves. We attempt to preserve these structures whenever possible. Both the azygos vein and internal thoracic vein can be sacrificed, but the stump may be ruptured by subsequent infection. The azygos vein is the boundary landmark of RU and RM, while the internal thoracic veins are the boundary landmark of UA and LA. The phrenic nerves and bilateral brachiocephalic veins are also boundary landmarks. We did not include the “paravertebral compartment (posterior mediastinum)” in our map of thoracic abscess distribution as we have not observed any abscesses of the paravertebral compartment. The paravertebral compartment has been defined as the area of the thoracic spine and the posterior area of the descending aorta (14). It was defined as the paravertebral compartment which was bounded by 1cm posterior to the anterior margin of the thoracic vertebral body (16). We have not observed any abscesses of the paravertebral component because it seems to be difficult for the abscess to descend to the area anatomically.
While the results of this study are encouraging, any conclusions should be tempered by the major limitation of the small number of patients. However, we can propose the categorization of distribution of DNM and distribution-specific drainage. Distribution-specific drainage is possible under the detail recognition of distribution of DNM. I hope that this proposal can be accepted widely and a new study of DNM patients will be planned.
Conclusions
We were able to cure all seven cases with DNM. Successful management may depend on rapid treatment being performed in collaboration with head and neck surgeons and appropriate thoracic drainage. For appropriate thoracic drainage, recognizing the exact distribution of the thoracic abscess is necessary, and our new mapping and classification approach with nine categories of thoracic abscess distribution may be helpful. In addition, repeated drainage may be needed to achieve a complete cure of DNM.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd.2020.03.82). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was approved by the Institutional Review Board of Aichi Medical University Hospital (No. 2019-208).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pearse HE. Mediastinitis following cervical suppuration. Ann Surg 1938;108:588-611. [Crossref] [PubMed]
- Wheatley MJ, Stirling MC, Kirsh MM, et al. Descending necrotizing mediastinitis: transcervical drainage is not enough. Ann Thorac Surg 1990;49:780-4. [Crossref] [PubMed]
- Corsten MJ, Shamji FM, Odell PF, et al. Optimal treatment of descending necrotizing mediastinitis. Thorax 1997;52:702-8. [Crossref] [PubMed]
- Kiernan PD, Hernandez A, Byrne WD, et al. Descending cervical mediastinitis. Ann Thorac Surg 1998;65:1483-8. [Crossref] [PubMed]
- Ridder GJ, Maier W, Kinzer S, et al. Descending necrotizing mediastinitis: contemporary trends in etiology, diagnosis, management, and outcome. Ann Surg 2010;251:528-34. [Crossref] [PubMed]
- Prado-Calleros HM, Jiménez-Fuentes E, Jiménez-Escobar I. Descending necrotizing mediastinitis: Systematic review on its treatment in the last 6 years, 75 years after its description. Head Neck 2016;38 Suppl 1:E2275-83. [Crossref] [PubMed]
- Palma DM, Giuliano S, Cracchiolo AN, et al. Clinical features and outcome of patients with descending necrotizing mediastinitis: prospective analysis of 34 cases. Infection 2016;44:77-84. [Crossref] [PubMed]
- Min HK, Choi YS, Shim YM, et al. Descending necrotizing mediastinitis: a minimally invasive approach using video-assisted thoracoscopic surgery. Ann Thorac Surg 2004;77:306-10. [Crossref] [PubMed]
- Son HS, Cho JH, Park SM, et al. Management of descending necrotizing mediastinitis using minimally invasive video-assisted thoracoscopic surgery. Surg Laparosc Endosc Percutan Tech 2006;16:379-82. [Crossref] [PubMed]
- Cho JS, Kim YD. Treatment of mediastinitis using video-assisted thoracoscopic surgery. Eur J Cardiothorac Surg 2008;34:520-4. [Crossref] [PubMed]
- Son HS, Cho JH, Park SM, et al. Management of descending necrotizing mediastinitis using minimally invasive video-assisted thoracoscopic surgery. Surg Laparosc Endosc Percutan Tech 2006;16:379-82. [Crossref] [PubMed]
- Estrera AS, Landay MJ, Grisham JM, et al. Descending necrotizing mediastinitis. Surg Gynecol Obstet 1983;157:545-52. [PubMed]
- Endo S, Murayama F, Hasegawa T, et al. Guideline of surgical management based on diffusion of descending necrotizing mediastinitis. Jpn J Thorac Cardiovasc Surg 1999;47:14-9. [Crossref] [PubMed]
- Carter BW, Tomiyama N, Bhora FY, et al. A modern definition of mediastinal compartments. J Thorac Oncol 2014;9:S97-101. [Crossref] [PubMed]
- Sumi Y. Descending necrotizing mediastinitis: 5 years of published data in Japan. Acute Med Surg 2014;2:1-12. [Crossref] [PubMed]
- Fujimoto K, Hara M, Tomiyama N, et al. Proposal for a new mediastinal compartment classification of transverse plane images according to the Japanese Association for Research on the Thymus (JART) General Rules for the Study of Mediastinal Tumors. Oncol Rep 2014;31:565-72. [Crossref] [PubMed]


