Benefit of initial dual-therapy on stroke prevention in Chinese hypertensive patients: a real world cohort study
Introduction
Stroke is one of the leading causes of mortality and disability worldwide (1,2). In China, stroke has surpassed coronary heart disease and become the leading cause of death among adults, with 1,500,000 deaths in 2011 (3). Its mortality in China is 4-5 times higher than that in the United States and European countries, 3.5 times higher than that in Japan, and also higher than those in Thailand, India and other developing countries (4). High blood pressure is the most important risk factor for stroke, which accounts for 40-50% of stroke in Chinese population (5). Effective treatment of hypertension can achieve blood pressure control (6). Many large-scale multi-center randomized controlled studies and meta-analysis have demonstrated that lowering blood pressure in hypertensive patients is fundamental for the prevention of stroke and other cardiovascular events (7-11).
Hypertension is a complex chronic disease, with an etiology involving multiple physiologic mechanisms, including the renin-angiotensin-aldosterone system, sympathetic tone, and body fluid volume regulatory system (12). Individual antihypertensive drugs target single mechanism and have limited efficacy in advanced hypertension (13,14). Therefore most current clinical hypertension guidelines recommend combination of at least two anti-hypertensive drugs for the initial treatment of grade ≥2 hypertension or complicated hypertension (5,15,16). During the initial phase of hypertension treatment, combination therapy has been shown to increase the rate of blood pressure control, but also shorten the time to achieve control (17,18). Randomized controlled clinical studies demonstrate a reduced incidence of cardiovascular events including stroke, even for patients with grade 1 hypertension, if target blood pressure was achieved within 3 to 12 months during initial treatment (19,20).
Recent data from controlled trial with limited inclusion of Asian populations and relatively short observation period (21) suggest that initial combination therapy might effectively prevent stroke in hypertensive patients. However, data in Chinese population is limited. Thus we compared the impact of initial mono- versus combination-therapy in preventing stroke in Chinese hypertensive patients, using the population-based “Shanghai Electronic Health Record Management System of Community Residents (SEHRMSCR)”.
Methods
Data source
All the data were obtained from the follow-up database of the population-based “Shanghai Electronic Health Record Management System of Community Residents (SEHRMSCR)”. As previously described (22), SEHRMSCR is an electronic health record-based local health information platform in Shanghai, China, which is established in 2005, it covers 93.05% (n=830,400) of the local permanent residents and 30.5% (n=334,800) of the floating populations in the Minhang District, Shanghai. Results from medical records, physical examination, chronic disease management, two-way consultation, and medication management are collected and transmitted through the network and stored at a central location. Standard Operating Procedure (SOP) has been developed for information gathering, recording and transmission, and local medical staff has undergone training for standardized information collection and management. Compliance with SOP is verified by independent audits on a regular basis. This registration system was sponsored and supervised by Shanghai Health Bureau and the data collection and information store complied with international standards, including data confidentiality and safety. This study was approved by the Ethics Committee of Fudan University.
Inclusion criteria
From the database, follow-up data of hypertensive patients from January 1 2005 to July 31 2011 were selected. Inclusion criteria were: (I) systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥90 mmHg (measured on three different days, with an interval of at least 14 days); (II) at least 18 years of age; (III) no history of stroke; (IV) drug-naive for ≥6 months before enrollment; (V) initiation of single- or dual-antihypertensive therapy. Exclusion criteria included: (I) secondary hypertension; (II) history of malignancy; (III) steroid treatment; (IV) patients with unclear history of stroke at baseline or during follow-up (V) subjects taking ≥3 classes of antihypertensive drugs and/or using antihypertensive drugs that contain traditional Chinese drugs/components.
Operational definitions
Based on the registration data in the SEHRMSCR, the diagnosis of ‘stroke’ included ischemic (ICD-10 code I63-I67) and hemorrhagic stroke (ICD-10 code I61), and transient ischemic attack (TIA) (ICD-10 code G45). New-onset stroke was defined as patients who had no history of stroke at baseline, but were diagnosed with stroke during the follow-up period.
Initial antihypertensive drugs included five drug classes: calcium channel blockers (CCB), beta -blockers, angiotensin II receptor blockers (ARB), angiotensin converting enzyme inhibitor (ACEI), and diuretics. The time of drug initiation is defined as the baseline (i.e., month 0); the follow-up is defined as the ends of months 6, 12, 24, and 42. Four time periods are defined: 0-6, 0-12, 0-24, and 0-42 months.
The decrease in blood pressure is defined as the difference between the recorded blood pressure at baseline versus each time point (i.e., the ends of months 6, 12, 24, and 42). Target blood pressure control rate in patients without diabetes or kidney disease, is defined as SBP <140 mmHg and DBP <90 mmHg. In patients with diabetes or kidney disease, it is defined as SBP <130 mmHg and DBP <80 mmHg (5). The target blood pressure control rate is the percentage of the cumulated patients who achieved the target blood pressure among the total sample size (4).
“Switching of antihypertensive therapy”, it refers to the condition of patients in the initial mono-therapy group, who were switched to combination drugs/traditional Chinese drugs/more than two classes of drugs during the follow-up period were recorded. Also patient in the initial combination group, who were switched to mono-therapy/traditional Chinese drugs/more than two classes of drugs were recorded. Switch rates were calculated at the ends of months 6, 12, 24, and 42 as cross-sectional time points.
The switch rate was defined as the ratio between the number of patients whose initial treatment was switched and that of cumulated patients who received antihypertensive therapy in that month.
Other variables
In addition to baseline blood pressure (SBP and DBP), follow-up blood pressure, hypertensive medications, and adjustment of medications during the follow-up, the following information was collected from the database: Socio-demographic characteristics (age, sex, height, and weight), cardiovascular risk factors (smoking, total cholesterol, early-onset family history of cardiovascular disease, and diabetes), target organ damage (left ventricular hypertrophy, proteinuria or abnormal serum creatinine, atherosclerotic plaque, retinal artery stenosis), cerebrovascular (stroke, TIA), and cardiovascular disease history (myocardial infarction, angina, congestive heart failure, and kidney diseases).
Statistical analysis
Based on their initial therapy, subjects were divided into the dual-therapy group and mono-therapy group. Baseline characteristics, initial medications, decrease in blood pressure, target blood pressure control rate, drug switching patterns, and incidence density (cases per 100 person-years) of stroke during the follow-up period were described. The inter-group differences of continuous variables were compared using t-test, and those of categorical variables with chi-square test/Fisher’s exact test. The Kaplan-Meier method (Log-rank test) was used for the comparison of stroke risks in both groups. In the Cox proportional hazards model, the baseline factors including socio-demographic characteristics, baseline blood pressure, history of cardiovascular disease, cardiovascular disease risk factors, and target organ damage were included. The unadjusted and adjusted hazard ratio (HR) and 95% confidence interval (95% CI) of the stroke between these two groups were calculated. All the statistical analyses were carried out using the SAS 9.3 software and Stata 11.0.
Results
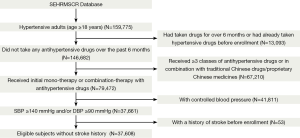
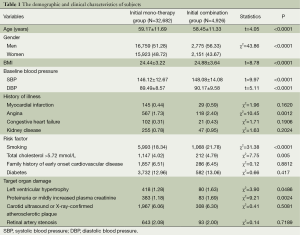
A total of 37,608 subjects met the inclusion criteria and were enrolled in this cohort (Figure 1). The initial mono- and dual-therapy group included 32,682 (86.9%) and 4,926 (13.1%) subjects, respectively. Table 1 shows the baseline data of the two groups. Overall, compared with those in the mono-therapy group, patients in the combination group were significantly younger, had a higher percentage of male subjects, a higher body mass index (BMI), and higher baseline blood pressure (DBP and SBP). In addition, the incidence of angina, smoking, total cholesterol, left ventricular hypertrophy, proteinuria, increased plasma creatinine of combination group were also significantly higher than mono group (P≤0.0486).
Full table
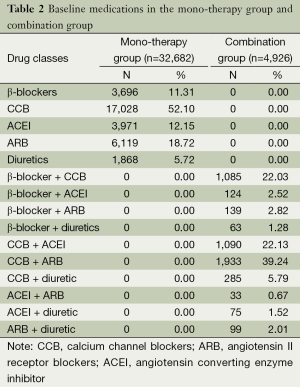
As shown in Table 2, for initial treatment, the most commonly used drug in the mono-therapy group was CCBs (52.10%), followed by ARBs (18.72%). In the dual-therapy group, the most common combination was “CCB + ARB” (39.24%), followed by “CCB + ACEI” (22.13%).
Full table
As shown in Table 3, during 42 months of follow-up, 40.3% of patients in the mono-therapy group had switched to combination therapy, most commonly addition of traditional Chinese drugs or proprietary Chinese medicines. In the dual-therapy group, 43.6% of patients had switched to other combination therapy, particularly the CCBs (7.8%).
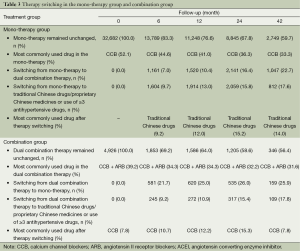
Full table
The reduction of SBP was significantly larger in the initial combination group than in the initial mono-therapy group, while the reduction of DBP showed no such difference at different time points except in the 42th follow-up month (Table 4).
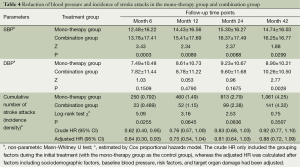
Full table
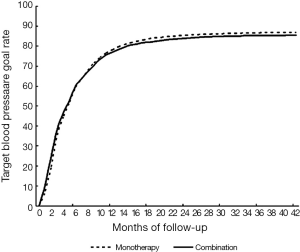
The achieved target blood pressure control rates of mono vs. combination at 6, 12, 24, and 42 months of follow-up, were 59.47% vs. 60.05%, 78.23% vs. 77.06%, 85.51% vs. 84.02%, and 86.90% vs. 85.44%, respectively. The target blood pressure control rate was significantly higher in the combination group than in the mono-therapy group before the 6th follow-up month; it was reversely higher in the mono-therapy group after the 13th follow-up month. Eventually, the target blood pressure control rates in both groups reached about 80% around the 15th follow-up month (Figure 2). However, the speed to achieve the target blood pressure was low in both groups.
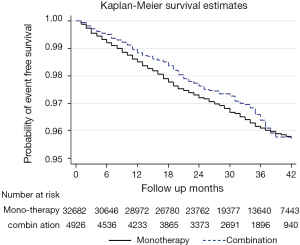
During the follow-up of 6, 12, 24, and 42 months, stroke events occurred in the mono- and dual-therapy group were 250 vs. 23, 460 vs. 52, 813 vs. 99, and 1,061 vs. 141, respectively. Their corresponding incidence densities of stroke were 0.792 vs. 0.489, 1.49 vs. 1.15, 2.79 vs. 2.38, and 4.25 vs. 4.32 (cases per 100 person-year), respectively (Figure 3). After controlling the possible confounding factors using the Cox proportional hazards model, the 6-month incidence density of stroke in the dual-therapy group was significantly lower than mono-therapy group (adjusted HR 0.64; 95% CI: 0.30-0.93) (Table 4) . However, there were no significant differences of the incidence density were observed at 12, 24, and 48 months.
Discussion
This study explored the preventive effect of combination anti-hypertensive therapy on stroke based a very large sample of hypertensive patients in “real world” practice. Despite this is an observational study, which is different from a strictly-designed clinical trial, we still have several interesting findings. Overall, our data demonstrates that, for patients with uncontrolled hypertension in real “world” clinical practice, initial dual therapy is more effective for the prevention of stroke during the first 6 months of treatment, but not thereafter. The data provides important insights and has important implications for the early dual treatment of Chinese hypertensive subjects.
In this study, only 13% of subjects in our cohort were started on dual therapy, which was significantly lower than the reported figure of 26% among hypertensive outpatients in the clinical practice of United States (23). Also, the rates of medication switching were high in both the mono- and dual-therapy groups. The target blood pressure control rate and the time to reach the target blood pressure differed from those reported in randomized controlled trials (RCTs) (17,18,24,25). The speed to achieve the target blood pressure was low in both groups; this phenomenon might be due to the inadequate capacity of hypertension treatment of Chinese internal physicians, low adherence of drug treatment of Chinese hypertensive patients and intolerable side effects of anti-hypertensive drugs. Further more, the differences between our findings and those from RCTs likely reflect differences in the health care setting and the complexity of blood pressure control in clinical practice, that is, our study is based on data from real-world health records, the treatment assignment and compliance are therefore not controlled and standardized as would be the case in a prospective trial, but the data accurately reflect “real-world” treatment conditions.
A main finding is the early benefit of dual therapy, with reduced incidence of stroke during the first 6 months, but no significant difference during subsequent 6-24 months. This finding supports prior data that early control of hypertension can remarkably reduce the risk of cardiovascular events (19,20,26). This could be ascribed to the rapid effect of initial blood pressure control, less side-effect, better blood pressure control, and low rate of medication in dual therapy group. However, the risk of stroke did not parallel the blood pressure level: the target blood pressure control rate and stroke incidence differed significantly only during the first 6 months, while the significant differences in incidence of stroke disappeared at 12, 24, and 42 months, even after the confounding factors were adjusted. There might be many factors influence the stroke prevention effects due to the observational nature of real-world study. In this context, the choice of medications is critical. It is known to all, CCBs have been widely used in clinical practice due to their good antihypertensive effect, few contraindications, and potential for combination with other anti-hypertensives. In our cohort, the initial therapy and maintenance therapy in both groups were mainly CCB-based (alone or in combination), and CCB+ARB was the dominant therapy after medication switching in the combination group. As demonstrated by the majority of studies (9,27-31), both CCBs and ARBs, alone or in combination, can effectively prevent new-onset stroke. Thus this medication use pattern might confound preventive effect of new-onset stroke. This pattern seemed consistent with the Chinese guidelines for the management of hypertension (4), in which recommend that CCB-based antihypertensive therapy as the first-line treatment for high blood pressure in China. Furthermore, the lack of concordance between risk of stroke and blood pressure control might be related to confounding effects due to drug switching specifically to the decreased proportion of the combination of CCB + ARB, which may have resulted to a decreased synergistic effect on stroke prevention. Therefore, even in patients whose blood pressure has been controlled by CCB + ARB, reduction of ARB (e.g., due to economic concerns) and switching to CCB alone is not recommended because such a switching strategy may potentially weaken the protective effect of ARBs against stroke (32). Boutitie et al. reavealed that ARBs could not only lower blood pressure via angiotensin receptor AT1 but also provide stroke prevention by improving cerebral collateral circulation (via AT2) and enhancing hypoxic tolerance of nerve cells (33).
Our study had some limitations: first, as an observational study by nature, the subjects were not randomized, and therefore the baseline characteristics of these two groups were not comparable, and the results might be biased even after statistical adjustment for confounders. Second, blood pressure measurement, antihypertensive therapies, and diagnostic criteria of stroke were not standardized. Third, some influencing factors of the efficacy such as medication adherence and clinical inertia were not collected, and their potential confounding effects could not be analyzed.
In conclusion, our study demonstrates that initial combination therapy plays an important role in early prevention and management of the new-onset stroke in hypertensive patients. The combination of CCB and ARB may exert synergistic effect on stroke prevention, and therefore should be maintained even after the blood pressure goal is reached. Based on this data from a large cohort of Chinese hypertensive patients, combination antihypertensive therapy seems to be a beneficial initial strategy for early stroke prevention.
Acknowledgements
Funding: The study was supported by grants from Novartis GCR.
Disclosure: Mr. Yu-Song He is an employee of Novartis. The funding source had no role in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript. No other disclosures were reported.
References
- Feigin VL, Lawes CM, Bennett DA, et al. Worldwide stroke incidence and early case fatality reported in 56 population-based studies: a systematic review. Lancet Neurol 2009;8:355-69. [PubMed]
- Xu WH. Translational stroke: a rapidly expanding area! Ann Transl Med 2014;2:73. [PubMed]
- Li X, Song G, Jin Y, et al. Higher level of heme oxygenase-1 in patients with stroke than TIA. J Thorac Dis 2014;6:772-7. [PubMed]
- Saba L, Anzidei M, Piga M, et al. Multi-modal CT scanning in the evaluation of cerebrovascular disease patients. Cardiovasc Diagn Ther 2014;4:245-62. [PubMed]
- Zhang X, Tong F, Li CX, et al. A fast multiparameter MRI approach for acute stroke assessment on a 3T clinical scanner: preliminary results in a non-human primate model with transient ischemic occlusion. Quant Imaging Med Surg 2014;4:112-22. [PubMed]
- Weber MA, Bakris GL, Dahlöf B, et al. Baseline characteristics in the Avoiding Cardiovascular events through Combination therapy in Patients Living with Systolic Hypertension (ACCOMPLISH) trial: a hypertensive population at high cardiovascular risk. Blood Press 2007;16:13-9. [PubMed]
- Liu L, Zhang Y, Liu G, et al. The Felodipine Event Reduction (FEVER) Study: a randomized long-term placebo-controlled trial in Chinese hypertensive patients. J Hypertens 2005;23:2157-72. [PubMed]
- Julius S, Kjeldsen SE, Weber M, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet 2004;363:2022-31. [PubMed]
- Sever PS, Dahlöf B, Poulter NR, et al. Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial--Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial. Lancet 2003;361:1149-58. [PubMed]
- Law MR, Morris JK, Wald NJ. Use of blood pressure lowering drugs in the prevention of cardiovascular disease: meta-analysis of 147 randomised trials in the context of expectations from prospective epidemiological studies. BMJ 2009;338:b1665.
- Rashid P, Leonardi-Bee J, Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke 2003;34:2741-8. [PubMed]
- Takahashi H, Yoshika M, Komiyama Y, et al. The central mechanism underlying hypertension: a review of the roles of sodium ions, epithelial sodium channels, the renin-angiotensin-aldosterone system, oxidative stress and endogenous digitalis in the brain. Hypertens Res 2011;34:1147-60. [PubMed]
- Hansson L, Zanchetti A, Carruthers SG, et al. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet 1998;351:1755-62. [PubMed]
- Walley T, Duggan AK, Haycox AR, et al. Treatment for newly diagnosed hypertension: patterns of prescribing and antihypertensive effectiveness in the UK. J R Soc Med 2003;96:525-31. [PubMed]
- Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007;28:1462-536. [PubMed]
- Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560-72. [PubMed]
- Flack JM, Calhoun DA, Satlin L, et al. Efficacy and safety of initial combination therapy with amlodipine/valsartan compared with amlodipine monotherapy in black patients with stage 2 hypertension: the EX-STAND study. J Hum Hypertens 2009;23:479-89. [PubMed]
- Weir MR, Levy D, Crikelair N, et al. Time to achieve blood-pressure goal: influence of dose of valsartan monotherapy and valsartan and hydrochlorothiazide combination therapy. Am J Hypertens 2007;20:807-15. [PubMed]
- Weber MA, Julius S, Kjeldsen SE, et al. Blood pressure dependent and independent effects of antihypertensive treatment on clinical events in the VALUE Trial. Lancet 2004;363:2049-51. [PubMed]
- Philipp T, Glazer RD, Wernsing M, et al. Initial combination therapy with amlodipine/valsartan compared with monotherapy in the treatment of hypertension. J Am Soc Hypertens 2011;5:417-24. [PubMed]
- Liu M, Wu B, Wang WZ, et al. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol 2007;6:456-64. [PubMed]
- Health Bureau of Minxing District of Shanghai Municipal. Establishing the new regional health information platform: the design of electronic health record (EHR) based resident health information platform in Minxing District. China Information: electronic medicine 2010;3:63-5.
- Egan BM, Bandyopadhyay D, Shaftman SR, et al. Initial monotherapy and combination therapy and hypertension control the first year. Hypertension 2012;59:1124-31. [PubMed]
- Sowers JR, Lastra G, Rocha R, et al. Initial combination therapy compared with monotherapy in diabetic hypertensive patients. J Clin Hypertens (Greenwich) 2008;10:668-76. [PubMed]
- Everett BM, Glynn RJ, Danielson E, et al. Combination therapy versus monotherapy as initial treatment for stage 2 hypertension: a prespecified subgroup analysis of a community-based, randomized, open-label trial. Clin Ther 2008;30:661-72. [PubMed]
- Gradman AH, Parisé H, Lefebvre P, et al. Initial combination therapy reduces the risk of cardiovascular events in hypertensive patients: a matched cohort study. Hypertension 2013;61:309-18. [PubMed]
- Staessen JA, Wang JG, Thijs L. Cardiovascular protection and blood pressure reduction: a meta-analysis. Lancet 2001;358:1305-15. [PubMed]
- Modi P, Chitwood WR Jr. Retrograde femoral arterial perfusion and stroke risk during minimally invasive mitral valve surgery: is there cause for concern? Ann Cardiothorac Surg 2013;2:E1. [PubMed]
- Sun BG, Meng J, Xiang T, et al. Acupuncture of the Five Shu Acupoints in spleen meridian to lower blood uric acid level. Ann Palliat Med 2014;3:22-7. [PubMed]
- Staessen JA, Gasowski J, Wang JG, et al. Risks of untreated and treated isolated systolic hypertension in the elderly: meta-analysis of outcome trials. Lancet 2000;355:865-72. [PubMed]
- Bosch J, Yusuf S, Pogue J, et al. Use of ramipril in preventing stroke: double blind randomised trial. BMJ 2002;324:699-702. [PubMed]
- Schrader J, Lüders S. Preventing stroke. BMJ 2002;324:687-8. [PubMed]
- Boutitie F, Oprisiu R, Achard JM, et al. Does a change in angiotensin II formation caused by antihypertensive drugs affect the risk of stroke? A meta-analysis of trials according to treatment with potentially different effects on angiotensin II. J Hypertens 2007;25:1543-53. [PubMed]