Nurse led Patient Education Programme for patients undergoing a lung resection for primary lung cancer
Introduction
All patients who are due to undergo a lung resection within the thoracic surgical unit based at St James’s university hospital, Leeds, UK are invited to attend a Patient Education Programme (PEP) which has been developed by the thoracic surgical nurse specialist. The aims of the PEP are to:
- Improve patient and carer understanding of what is involved in undergoing a lung resection;
- Provide a realistic overview of the hospital experience;
- Ensure that patients and carers are aware of the importance of self-management in recovery;
- Pre-empt and decrease anxiety for patients and carers;
- Communicate that thoracic surgery for lung cancer has a predictable course of recovery and;
- Prepare the patient and carers for post-discharge care needs.
Regional demographics
The thoracic surgical unit is a regional service covering a population of almost 2.5 million receiving referrals from the Yorkshire Cancer Network (YCN). The service offers elective surgery to patients with benign and malignant pulmonary, mediastinal, pleural and oesophageal diseases and an acute service.
The thoracic surgical team consists of five thoracic surgeons and a Macmillan thoracic surgical nurse specialist (TSNS). The team form part of the core membership of the six multidisciplinary teams (MDT) of Leeds, Bradford, Calderdale, Airedale, Harrogate and Mid Yorkshire Trusts. In 2013-2014 there were approximately 1,500 thoracic surgical procedures with around 80 per cent for cancer.
Background to the development of PEP
The concept of the PEP was developed in Leeds following the employment of the TSNS in 2011 and subsequent analysis of patient feedback with regards to the thoracic surgical service. Prior to the appointment of the TSNS there were recognised inequalities in the co-ordination of care for patients who required thoracic surgery. The role of the TSNS was to focus on streamlining the patient pathways, providing support for patients and carers (including meeting information needs) and ensuring that there was proactive management in each patient’s case.
In 2012, the TSNS coordinated an analysis of patient interviews (conducted by Lamerton Swales Social Marketing Consultancy) from patients who had undergone lung resection to identify gaps in the experience of care. Key issues that arose in the patient interview report included that there was:
- Lack of support for patients;
- No clear input in the management of expectations both pre and post-surgery;
- An under-utilisation of written information and;
- A desire from patients to have face to face discussions with health professionals.
The action plan following this detailed analysis was to develop the service to reduce inequalities in patient care, enhance the patient experience, patient reported outcome measures and the efficiency of hospital resources. The PEP was part of the action plan and was implemented in July 2013.
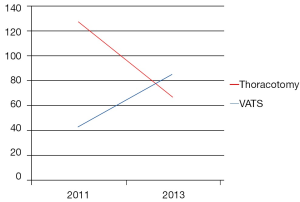
The thoracic surgical service had also seen an increase in resection rates from 15.6 percent in 2009 (1) to 17.3 percent in 2012 (2) with an increasing number of these being performed by video assisted thorascopic surgery (VATS) (Figure 1). This was also important to consider as due to the decreased length of stay for patients undergoing VATS resection there was therefore less time available in hospital to enable the promotion of self-management in recovery which includes physiotherapy and pain management.
The development of the PEP has been underpinned by the principles of utilising patient education to promote a shared care approach which has been successfully established in another thoracic surgical centre. Kerr et al. (3) implemented a Prehabilitation Programme based at the heart of England NHS Foundation Trust in Birmingham and incorporated exercise pre and post operatively along with patient education. There was demonstration of:
- The postoperative pulmonary complication rate falling from 17 percent to 7 percent;
- A reduction in the length of stay;
- Enhanced patient experience in the service and;
- Decreased rates of readmission which translated into cost savings.
Review of the literature
Garretson et al. (4) concluded that with Preoperative Education Programmes patients would no longer arrive at the operating theatre frightened and unaware of what will happen to them. Walker (5) found that the provision of good quality preoperative information facilitates patient’s active involvement in their care and may contribute to an overall increase in satisfaction. When considering the development of a pulmonary resection education module in lung surgery this can improve patient preparedness, relieve anxiety, improves pain perception, enhance patient experience and impact outcomes (6). Blay et al. (7) concluded that preadmission information intervention helps reduce postoperative pain levels and significantly increases knowledge of self-care and complication management.
The benefits of giving good quality preoperative information to patients can:
- Influence experience of post-operative pain by decreasing preoperative anxiety (8);
- Increase knowledge of self-care and complication management (9);
- Increase satisfaction of care (5);
- Decrease preoperative state of anxiety (10) and;
- Promote exercise to prevent post-operative complications.
The principles of the PEP are underpinned in United Kingdom national guidance. The NHS Enhanced Recovery Partnership Programme (NHSIII 2008) (11) focuses on improving patient outcomes and speeding up a patient’s recovery after surgery with benefits to both patients and staff. The programme focuses on making sure that patients are active participants in their own recovery process by making informed decisions and by managing expectations.
The evidence and guidance produced supports the implementation of the PEP.
The pathway to PEP
The programme is co-ordinated by the TSNS and is held once a week lasting 2 hours. Patients suitable to attend PEP are identified in the thoracic surgical clinic by the TSNS after they have been seen by the consultant thoracic surgeon. A full explanation of the purpose of the PEP is provided along with written information detailing the date, time and location.
The PEP is held in the rehabilitation unit in the Leeds cancer centre. On the day of the PEP patients and carers are greeted and welcomed by the TSNS. The room is set up with an overhead projector and laptop to present each topic.
Evidence was gathered to support the topics on the agenda to provide a comprehensive and well-structured programme to meet the aims of the PEP.
PEP topics
The introduction describes the aims of the PEP, the topics and potential benefits of attending the programme.
Admission discharge information
A photograph gallery via PowerPoint depicts the journey from entering the hospital, ward and the interactions with the hospital team including discharge. The patient in the photographs is a member of the Lung Cancer and Mesothelioma Patient Support Group. Discharge advice is given with regards to wound management, pain control, physiotherapy, driving and flying. Follow up is discussed and the importance of contacting the TSNS if advice is required.
The aim of this is to ensure that anxiety related to the admission is minimised and also gives the opportunity for the patients to ask any questions about discharge planning. Often questions are asked about what type of care is required after surgery and if any additional help will be required at home.
Physiotherapy
The thoracic physiotherapist delivers the session on physiotherapy which includes advice on exercises prior to admission, the days following surgery and what to do when at home. A diary is provided to help guide the exercise regime and patients are encouraged to complete this. During this session the patients and carers are invited to take part in the exercises with the physiotherapist demonstrating the correct application of each exercise. In addition the importance of keeping as active in the weeks prior to surgery as well as after is highlighted.
Data is being collected on the effectiveness of the physiotherapist interventions and will be available in due course. There is evidence to suggest that increasing physical activity prior to surgery has proven to contribute to improving patient outcomes (3,12).
Pain management
A detailed presentation is given with a particular focus on the reasons why pain control is required, how this is delivered and the potential side effects of medication. Patients are informed that good and effective pain management can help to prevent post-operative complications, a quicker recovery and to enable the ability to complete tasks such as mobilising soon after surgery and deep breathing exercises.
Patients are informed of the role of the ward nurses in pain management and to ensure that prompt advice is required if pain is not adequately controlled. It is promoted that if pain is present and the nursing team are not informed that this can lead to unnecessary discomfort which can potentially reduce appetite and energy levels, low mood and a delayed discharge.
Sjöling et al. (10) reported that patient satisfaction with pain management is significantly correlated to the preoperative information received and when information is provided it influences the experience of pain after surgery reducing preoperative anxiety. In addition, Niemi-Murola et al. (13) recommended preoperative interviews as an important tool to receive and give information concerning postoperative pain management.
Nutrition
Nutritional advice is provided. To promote fitness prior to surgery the principle of a balanced diet or maintained existing diet is provided. If patients do have weight loss then advice is given to enhance their current diet and consideration is made to utilising food supplements. Practical advice is given on what can be done whilst an inpatient to ensure nutritional intake is maintained immediately after surgery and during the recovery period.
Enhanced Recovery Programmes include dietary supplementation to ensure that patients are nutritionally optimised prior to surgery as poor nutritional intake before or during the wound healing process can lead to impaired healing resulting in wound breakdown (14).
The dietician team has been involved with the information contained in the presentation and reflects advice provided in national guidance (National Lung Cancer Forum for Nurses 2014) (15).
Adjuvant treatment
Adjuvant therapy is considered as an option for all patients following lung resection. This topic is included to ensure that patients are aware of the possibility that further treatment may be required. This is often not mentioned as a possibility in clinic consultations so a description of the Multi-Disciplinary Team decision making process is outlined together with the reasons why chemotherapy or radiotherapy may be recommended.
Discussing the potential need for adjuvant treatment may increase treatment uptake if required together with reducing anxiety when mentioned as a possibility following surgery.
Smoking cessation
Smoking cessation is a key area of promoting a healthy lifestyle. The majority of patients who require lung resection have been smokers or continue to smoke. Patients who do smoke are actively encouraged to stop. An appointment with the Smoking Cessation Service is made directly from the thoracic surgical clinic for those keen to stop immediately. Patients who require time to think about stopping are provided with the smoking cessation clinic information which includes Drop in Clinics. Written information is available for patients to take home to aid in smoking cessation.
Patients who are still smoking when the PEP is delivered are given further encouragement and advice and this is provided in the presentation. The benefits of stopping smoking are detailed including the reduction of anaesthetic risk, recovery whilst in high dependency, to aid physiotherapy whilst an inpatient, the reduction in risk of developing lung cancer in the future and the financial savings.
The relationship between cigarette smoking and an increase risk in postoperative pulmonary complications is recognised (16-18). Smoking cessation within one month before lung cancer surgery decreases the risk of major pulmonary complications and a reduction in the incidence of wound infection compared to those that continued to smoke (8,14,19). Stopping smoking after diagnosis has been correlated with increased overall survival and can decrease the rate of recurrence compared with continuing smokers (20-22).
If a patient requires adjuvant treatment there is evidence to suggest decreased effectiveness of anti-cancer treatments in smokers. Rades et al. (23) concluded that smoking during radiotherapy had a significant detrimental effect on local regional control of the cancer. Chen et al. (24) commented that smoking during radiotherapy for head and neck cancer is associated with unfavourable outcomes. Videtic et al. (25) found that patients who continued to smoke through combination chemotherapy and radiotherapy for small cell lung had poorer survival rates than those who did not.
Information and support services
Written patient information is available with regards to lung cancer, surgery, nutrition, smoking cessation and local cancer support groups. A DVD is also available with narratives from patients who have undergone cancer treatments (produced by the Roy Castle Lung Cancer Foundation 2015) (26). Patients are given information about the local Patient Support Group and are actively encouraged to attend to provide ongoing mutual support. All patients are able to access to the TSNS and the cancer unit lung cancer nurse specialist via telephone advice lines.
Patient involvement
The Leeds Lung Cancer and Mesothelioma Patient Support Group meet once a month with one of its roles providing expert advice on the development of the lung cancer service.
The group was pivotal in providing valuable insight into how the thoracic surgical service could develop in responding to patient’s needs and requirements. When the idea of the PEP was initiated the group members (in particular those who had undergone lung resection) were asked for their opinion about the topics that needed to be included. All patients felt that if this type of programme had been in place prior to treatment this would have been extremely important in their care to prepare for surgery and in the time following surgery. The group were involved in the pilot run of the programme and provided feedback on changes that were required. Regular feedback is provided to the group with consideration now being made to having a member present on the day of the PEP to answer any questions and to provide a first-hand experience of thoracic surgery.
Audit
Audit of the PEP has been undertaken. It is also part of a wider thoracic surgical service evaluation to identify patient experience and quality of life after lung resection. Initial results will be provided at the ESTS Conference in June 2015 from which further interventions will be developed.
For the first six months of PEP patients were asked for immediate feedback on the day they attended the programme to establish the relevance of topics, effectiveness at reducing anxiety and the presentation style.
The feedback questionnaire showed that patients felt the sessions were delivered in a way that they could understand, had helped to reduce anxiety about forthcoming surgery and found the programme as a whole very useful. Comments included:
- “Very reassuring, easy to understand, excellent programme”;
- “Well presented and beneficial for patient having lung surgery”;
- “Very informative and prepared everyone well for what is about to take place”;
- “Particularly liked the emphasis on exercise and nutrition before surgery”.
In 2013 a patient satisfaction survey was conducted of 186 patients who had attended the PEP. Comparisons were made between those who had attended and those who had not. Analysis of data demonstrated that 100 per cent of patients who had attended PEP felt well prepared for surgery compared to 88 per cent of those who had not.
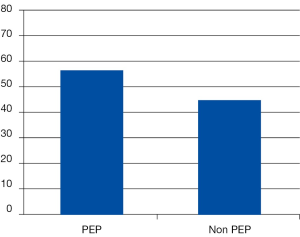
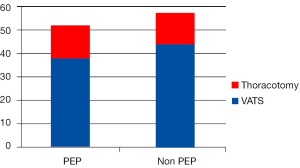
An audit conducted in 2014 demonstrated a reduction in length of stay in those attending PEP compared to those who did not attend. A total of 67 per cent of patients who attended PEP were discharged by day four following their operation compared to 55 per cent who had not attended PEP (Figure 2). There was little difference between patients receiving VATS and thoracotomy (Figure 3) providing evidence that there is a reduced length of stay for patients attending PEP.
The results support the evidence that a well thought out structured pre-operative PEP has a positive impact on patient reported outcomes as well as length of stay.
The future
The team are in the process of developing a short film to replace the photographic journey which will show what happens when patients are admitted to the hospital and the subsequent pathway.
Quality of life data collected from the thoracic surgical clinics will help to identify intervention measures that can be implemented at any point of the treatment pathway. Such measures may be related to breathless management or pain control.
At the time of writing there are plans to repeat patient experience interviews. The patient narratives will help to focus the continued development of the PEP on issues that the patients themselves have highlighted.
The thoracic physiotherapists are currently conducting an audit to evaluate their impact on patient recovery and experience.
Conclusions
The evidence to support the aims of the PEP to improve patient experience, promoting a shared care approach, shortening length of stay, reducing post-operative complications and enhancing the physical and psychological wellbeing of patients who require a lung resection is gradually developing.
It is expected that where patients have modified their behaviour in smoking cessation and physical activity this will have a longer term benefit on their own and family’s health and also on health resources.
The PEP was developed and implemented with minimal additional resource and with the concentration of Health Professionals time there has potential cost savings to the hospital. The team has become very cohesive with the enthusiasm of the team benefiting the running of PEP.
The principles of the PEP could be implemented into any surgical pathway and potentially into other areas of health care.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- National Lung Cancer Audit: 2010 Patient Cohort. 7th annual report of the National Lung Cancer Audit. NHS Trusts. 2010. Available online: www.hscic.gov.uk/searchcatalogue?productid=46&q=title%3a%22Lung+cancer%22&infotype=0%2fAudit&sort=Relevance&size=10&page=1#top, accessed on February 5, 2015.
- National Lung Cancer Audit, Open Data—2013. Health & Social Care information Centre. Available online: www.hscic.gov.uk/searchcatalogue?productid=14253&q=title%3a%22Lung+cancer%22&infotype=0%2fAudit&sort=Relevance&size=10&page=1#top, accessed on February 5, 2015.
- Kerr A, Wotton R, Bishay E, et al. Rehabilitation for Operated Lung Cancer Programme: 18 months outcomes. 27th EACTS Annual Meeting. Vienna, Austria, 2013.
- Garretson S. Benefits of Pre-Operative Information Programmes. Nursing Standard 2004;18:33-7. [PubMed]
- Walker JA. What is the effect of preoperative information on patient satisfaction? Br J Nurs 2007;16:27-32. [PubMed]
- Crabtree TD, Puri V, Bell JM, et al. Outcomes and perception of lung surgery with implementation of a patient video education module: a prospective cohort study. J Am Coll Surg 2012;214:816-21.e2.
- Blay N, Donoghue J. The effect of pre-admission education on domiciliary recovery following laparoscopic cholecystectomy. Aust J Adv Nurs 2005;22:14-9. [PubMed]
- Groth SS, Whitson BA, Kuskowski MA, et al. Impact of preoperative smoking status on postoperative complication rates and pulmonary function test results 1-year following pulmonary resection for non-small cell lung cancer. Lung Cancer 2009;64:352-7. [PubMed]
- Ong J, Miller PS, Appleby R, et al. Effect of a preoperative instructional digital video disc on patient knowledge and preparedness for engaging in postoperative care activities. Nurs Clin North Am 2009;44:103-15. [PubMed]
- Sjöling M, Nordahl G, Olofsson N, et al. The impact of preoperative information on state anxiety, postoperative pain and satisfaction with pain management. Patient Educ Couns 2003;51:169-76. [PubMed]
- National Health Service Institution of Innovation and Improvement (2008). Enhanced Recovery Programme. Available online: http://www.institute.nhs.uk/quality_and_service_improvement_tools/quality_and_service_improvement_tools/enhanced_recovery_programme.html, accessed on February 5, 2015.
- Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med 2013;188:e13-64. [PubMed]
- Niemi-Murola L, Pöyhiä R, Onkinen K, et al. Patient satisfaction with postoperative pain management--effect of preoperative factors. Pain Manag Nurs 2007;8:122-9. [PubMed]
- Williams L, Leaper D. Nutrition and Wound Healing. Clinical Nutrition Update 2000;5:3-5.
- National Lung Cancer Forum for Nurses (2014). A Practical Guide for Lung Cancer Nutritional Care. Available online: http://lungcancernutrition.com/A%20Practical%20Guide%20to%20Lung%20Cancer%20Nutritional%20Care.pdf, accessed on February 6, 2015.
- Vaporciyan AA, Merriman KW, Ece F, et al. Incidence of major pulmonary morbidity after pneumonectomy: association with timing of smoking cessation. Ann Thorac Surg 2002;73:420-5; discussion 425-6. [PubMed]
- Barrera R, Shi W, Amar D, et al. Smoking and timing of cessation: impact on pulmonary complications after thoracotomy. Chest 2005;127:1977-83. [PubMed]
- Mason DP, Subramanian S, Nowicki ER, et al. Impact of smoking cessation before resection of lung cancer: a Society of Thoracic Surgeons General Thoracic Surgery Database study. Ann Thorac Surg 2009;88:362-70; discussion 370-1. [PubMed]
- Sorensen LT, Karlsmark T, Gottrup F. Abstinence from smoking reduces incisional wound infection: a randomized controlled trial. Ann Surg 2003;238:1-5. [PubMed]
- Richardson GE, Tucker MA, Venzon DJ, et al. Smoking cessation after successful treatment of small-cell lung cancer is associated with fewer smoking-related second primary cancers. Ann Intern Med 1993;119:383-90. [PubMed]
- Parsons A, Daley A, Begh R, et al. Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: systematic review of observational studies with meta-analysis. BMJ 2010;340:b5569. [PubMed]
- Sitas F, Weber MF, Egger S, et al. Smoking cessation after cancer. J Clin Oncol 2014;32:3593-5. [PubMed]
- Rades D, Setter C, Schild SE, et al. Effect of smoking during radiotherapy, respiratory insufficiency, and hemoglobin levels on outcome in patients irradiated for non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 2008;71:1134-42. [PubMed]
- Chen AM, Chen LM, Vaughan A, et al. Tobacco smoking during radiation therapy for head-and-neck cancer is associated with unfavorable outcome. Int J Radiat Oncol Biol Phys 2011;79:414-9. [PubMed]
- Videtic GM, Stitt LW, Dar AR, et al. Continued cigarette smoking by patients receiving concurrent chemoradiotherapy for limited-stage small-cell lung cancer is associated with decreased survival. J Clin Oncol 2003;21:1544-9. [PubMed]
- Roy Castle Lung Cancer Foundation (2015). Living With Lung Cancer DVD. Available online: www.roycastle.org/how-we-can-help/Our-Publications/Lung-Cancer-DVD-and-Online-Videos, accessed on February 9, 2015.