Thoracic surgery and COVID-19: changes and managements during the pandemic
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has disrupted routine hospital services globally. Until Jul 10th, 12 million cases have been confirmed world widely with total deaths numbering over 50 thousand (1). This pandemic has had a massive impact on waits for elective operations, with tens of thousands of scheduled surgeries being cancelled or postponed (2). The post-pandemic evaluation and future planning should involve surgical services as an essential part to maintain appropriate surgical care for the population during an outbreak (3).
While there were numerous recommendations regarding surgery (4-9) and some predictive researches on the impact on surgery (2,10), no researches have yet explored the surgical volumes, distribution of surgical cases, or capacity of the hospital to deliver essential surgical services in the perspective of thoracic surgery.
In China, all the COVID-19 patients were treated in designated hospitals, therefore the thoracic surgery departments in non-COVID-19 hospitals may not well develop their tailored strategies in response to the pandemic due to insufficient experience. However, all the hospitals should be cautious and be prepared for a potential second wave of the disease.
In addition, the situation on cancellation of elective surgeries is unknown and it is not clear how to address a large backlog of thoracic surgeries when surgical priorities have changed dramatically to copy with the current challenges. During the pandemic peak period in China, medical supplies especially masks and personal protective equipment (PPE) were in short supply, it could help us to perform rationally and effectively on medical resources allocation if there were a prediction model.
The aim of this article is to deliberate the above issues by conducting a retrospective study in a real-world setting based on the available data from our hospital, which is one of the four designated COVID-19 hospitals in Guangzhou. Lessons can be learned from our changes and managements in each phase of response to COVID-19. We present the following article in accordance with the MDAR reporting checklist (available at http://dx.doi.org/10.21037/jtd-20-2883).
Methods
Medical records in The Department of Thoracic Surgery were used to collect for the analysis and comparison during the Wuhan lockdown (2020, Jan 23rd to Apr 8th). Hospital information system was searched to gather the surgery information. All the related information was exported in Microsoft Excel 2019 (Microsoft, Redmond, WA, USA) for inspecting and MySQL served as the relational database for continuously updated.
Two reviewers (ZR and RC) extracted the relevant data independently, and these data were then cross-checked. Additionally, inclusion criteria include: (I) patients who underwent surgery at the Department of Thoracic Surgery during the Wuhan lockdown; (II) patients who agreed to participate in the research and signed an informed consent form. The exclusion criteria included the following points: (I) missing detailed information; (II) patients underwent a surgery not available previously in our hospital.
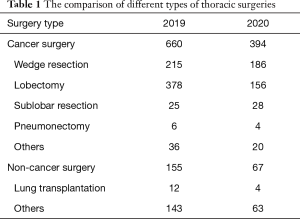
We extracted the number of surgical cases, ASA grades, number of emergency/elective surgical cases and other surgical related information during the Wuhan lockdown in Department of Thoracic Surgery to compare with the paired numbers of 2019 and analyzed the distribution differences. Moreover, thoracic surgeries were classified as lung cancer surgery and non-cancer surgery according to characteristic of operation types to discuss the detailed changes. Lung cancer surgeries were classified as wedge resection, sublobar resection, lobectomy, pneumonectomy and others according to pulmonary anatomy. Non-cancer surgeries were classified as lung transplantation and others.
We here discussed our guidelines in response to this outbreak. The related control measures implemented by our hospital from the start of the outbreak were collected from the department of hospital medical affairs.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the First Affiliated Hospital of Guangzhou Medical University (No. 2020-94) and informed consent was taken from all the patients.
Statistical analysis
A predicted model was built by using regression fitting and modeling according to data in last 5 years to research that the COVID-19 has impacted on thoracic surgery volume. Besides, we used the model to predict how long it will take in The Department of Thoracic Surgery to solve the backlog surgeries. A data analysis was performed by Python (Python version 3.7.0) on Jupyter notebook (11). Further details can be found in supplementary methods (Appendix 1). Figures were made using the drawing software Origin 2018 (OriginLab, MA, USA) and GraphPad Prism 8.0 (CA, USA).
Results
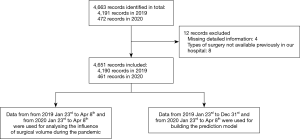
Patients from 2019 Jan 23rd to Dec 31st and from 2020 Jan 23rd to Apr 8th underwent surgery in The Department of Thoracic Surgery were reviewed consecutively. The study evaluated 4,651 (year 2019: 4,190; year 2020: 461) records for study inclusion. Among them, the data from 2019 Jan 23rd to Apr 8th to 2020 Jan 23rd to Apr 8th were used to explore the impact of the thoracic surgical operation during the pandemic, and all data were used to build the prediction models. To ensure the integrity and consistency of the data for each indicator, we excluded the unqualified sample records (Figure 1).
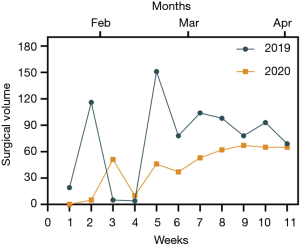
Surgical volume decreased during the COVID-19
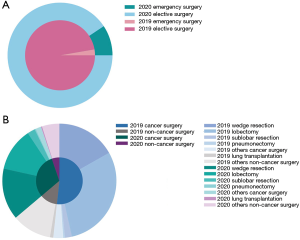
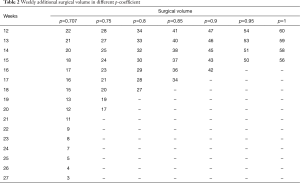
By comparing two sets (2019 vs. 2020) of surgical cases during the Wuhan lockdown, we found that the thoracic surgical volume in 2020 decreased overall (43.4%) (Figure 2). To compared with the last year, a significant reduction of elective surgeries was showed (47.3%), however, a 48.8% increase was shown in emergency surgery (Figure 3A, Figures S1,S2). We also compared the different types of thoracic surgeries, in all types of surgeries, the highest reduction is lung transplantation (66.7%) (Table 1, Figure 3B). There is no obvious difference among the classification based on age, gender and anesthesia level. The changes in surgical volumes according to the ASA grades were presented in Figure S3.
Full table
The outbreak response measures
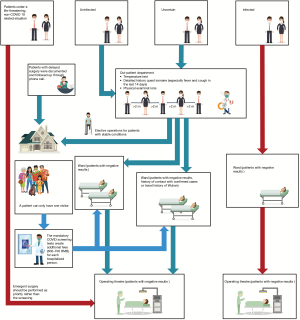
The workflow in the surgical department has changed and we believed that it will evolve as the pandemic continues. In our hospital, patients needing surgery are divided into three main categories in terms of COVID-19: infected, uncertain and uninfected. All patients were firstly arranged to a special fever clinic in our out-patient department where 2-meter distancing is required in the queue. After a temperature test, a detailed history questionnaire (especially fever and cough in the last 14 days) and physical examinations were performed by doctors with PPE.
Surgical indications were rigorously evaluated. Elective operations for patients with stable conditions were postponed but documented and followed up through phone call. A pulmonary computed tomography (CT) scan, nucleic acid sequencing of throat swab and a complete blood count (CBC) were mandatory before hospitalization for preliminary diagnosis of COVID-19 infection.
These testing requirements were the same for any companion requesting to enter the ward as well. A patient can only have one visitor and both the patient and visitor are not allowed to leave the ward without permission during hospitalization to avoid cross infection. The mandatory COVID screening tests create additional fees (600–700 RMB) for each hospitalized person. Considering the epidemic curve is flat in China now, with no upsurge in new infections and the community spread is minimal or controlled, a tomography (CT) scan and a CBC in the above screening tests have become optional since May 20th in our hospital, but the nucleic acid sequencing of throat swab is still a must.
Patients with positive results of COVID-19 screening tests were nursed in wards in a separate building. Patients with negative results, history of contact with confirmed cases or travel history of Wuhan were considered to be suspected cases and transferred to another specific ward. When patients were sent to hospital under a life-threating, non-COVID-19 related situation such as a car accident, emergent surgery should be performed as priority rather than the screening. Uninfected patients were transferred to the ward through a special lane to avoid cross infection. Individual accommodation was recommended for all patients and rigorous quarantine was applied for confirmed cases. Surgical management during the COVID-19 showed in Figure 4.
Existing data-based prediction model for delayed surgeries
In order to predict how many manual weeks the hospital can clear the backlog surgeries, a prediction model was designed:
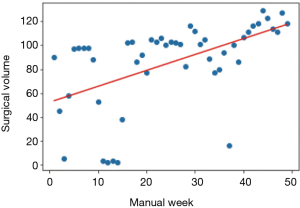
In this equation, 129 is the max value that the hospital can operate thoracic surgery in a week, p is a coefficient, p=1 means the all the thoracic surgeons are in position. We assume that in every week the p is same. w is the slope and the b is the intercept of the regression fitting function. x is the manual week (started at 12 because from Jan 23th to Apr 8th it passed 11 manual weeks). And by our calculates when the p is smaller than 0.7856 it will appear the situation that result is negative number which means in this week the hospital, instead of operating the overstock thoracic surgery in the time period which start at Jan 23th and end at Apr 8th, add new thoracic surgery to the overstock. So, the threshold value of p is 0.7856. Fit curve was showed in Figure 5.
It is a remarkable fact that as for the third and fourth manual week in 2019 and the first manual week in 2020 are the time during the Chinese Spring Festival. Few surgeries are operated in these manual weeks. We regard data in these 3 manual weeks as abnormal data. In order to keep the fitting function’s accuracy, we use Linear interpolation formula to simulate the thoracic surgical volume in these weeks.
Two different values of p-coefficient were used in this model: first, we assumed the p-coefficient =0.95, 0.90, 0.85, 0.80 and 0.75 which represented the all of the situation in The Department of Thoracic Surgery which exceed the threshold, time required in each situations was showed in Table 2 and Figure S4.
Full table
Discussion
The overall declined surgical volume in the Department of Thoracic Surgery during the Wuhan lockdown could be explained by multiple factors. Our hospital is one of the four designated COVID-19 hospitals in Guangzhou. From Jan 23rd to Apr 8th, there were 459 confirmed cases of COVID-19 found in Guangzhou, twenty of them were treated in our hospital. The number of blood donations has already dropped dramatically during the pandemic. The COVID-19 patients required a large amount of hospital resources such as blood plasma and many general supplies (12). Meanwhile, some of our healthcare workers were dispatched to the epicenter and the frontline healthcare workers in our hospital were rapidly altering their professional responsibilities to help hospital needs, which disarranged our normalcy. Studies have showed that in locations with widespread infections and limited resources, the risk of elective surgical procedures for patients and community may outweigh the benefit (13). As such, our hospital announced that all elective surgeries, and non-essential medical and surgical procedures be delayed at the start of the COVID-19 pandemic, which matched the guidance from The American College of Surgery posted a guideline about how to prioritize cases by describing the Elective Surgery Acuity Scale (ESAS) which has value of reference (14).
Regardless, even in the midst of a pandemic certain procedure types must be performed, including appropriate cancer treatment, emergent thoracic surgery and urgent lung transplantation, as these are considered life‐saving procedures. Thus, our panelists established the rules presented in our results to ensure the safety of healthcare workers and patients involved. From Jan 23rd to Apr 8th in 2020, there were 461 surgeries performed in the Department of Thoracic Surgery with zero cases of nosocomial COVID-19 infection. Despite COVID-19 being a threat, by developing a scientific and effective management of hospital, it is possible to ensure optimal surgical safety during this crisis.
Among all surgical types we reviewed in the Department of Thoracic Surgery, lung transplantation had the biggest reduction (66.7%) on cases. Limiting access to transplantation is associated with a significant loss of prognosis for most patients on the transplant list. The influence of organ transplantation is related to the impact on the donors and increasing risks of infection.
Risks of perioperative during COVID-19 pandemic
Firstly, the lack of effective test methods during the early stage of pandemic led to the uncertainty of surgery decision. The Royal College of Surgeons recommends pre-operative chest imaging with a chest X-ray or CT, especially if the patient has respiratory symptoms and is unable to be tested for COVID-19 prior to the operating room (15). However, a large proportion of COVID-19 patients are asymptomatic. Study from University of Oxford found that the 5% and 80% of people testing positive for SARS-CoV-2 may be asymptomatic (16), which means surgeons are exposed to danger even if all subjects were negative due to the testing limitations. With the improvement of technology, Yang et al. (17) found that nasopharyngeal and oropharyngeal testing has its limitations. During the pandemic, all patients could be considered to be potentially infected with the virus given the possibility of a false negative test.
Secondly, despite the promise of accuracy of test, risks associated with intraoperation should be noted. During the operation, adequate PPE in the operating room are necessary for the health of individual healthcare providers and an adequate workforce during the pandemic. During the pandemic, minimal operators should be arranged when surgery can work correctly, which can reduce the potential scope of infection to a minimum. All the COVID-19 related surgery should be operated in negative-pressure environment. All the surgeries which can generate aerosols demanded special attention, such as thoracoscopic surgery. Furthermore, there is no evidence for assessing the impact of different types of aerosol-generating surgery on operators. Therefore, we concluded that ventilation system in operating room should be promised in a high intensity situation.
Challenges in solving backlog of surgical cases
How to decide on the optimal timing of a thoracic surgery, work within limitations and keep an eye on potential subsequent waves of COVID-19 will continue to be important.
Multiple factors are affecting the surgical plan. Firstly, hospital facilities such as shortage of operating rooms, stricter standards and more complex admission process have led a longer time to complete a surgery. Secondly, the impact of pandemic for thoracic surgery is comprehensive. Since the outbreak, blood donations in our hospital have reduced largely. Thirdly, it is hard to estimate now whether some of measures in response to COVID-19 would become “new normal” and be implemented even after this pandemic. Further investigations are needed to validate the efficacy of each measure. Surgical decision should be updated frequently, especially in a new situation (18,19).
A pulmonary CT scan, nucleic acid sequencing of throat swab and a CBC were mandatory before hospitalization for preliminary diagnosis of COVID-19 infection.
Prediction model’s practical application to heavily affected population
We present proportional coefficient p to represent the ability to maintain surgical volume during the COVID-19. Policymakers and hospital managers can calculate the suitable coefficient according to the severity of the pandemic and the number of surgeons locally. The proportional coefficient p changes varied as the local COVID-19 pandemic situation, government measures, surgeon’s completion of surgery and other factors.
The same proportional coefficient p in each week was used in the design types of our research, the reason for doing so was the pandemic situation in Guangzhou and operative competence in our hospital was controllable and stable. Unless reemergence outbreak, we considered that our plan could maintain smoothly.
In the heavily affected area, millions of infected cases have been reported. The incidence rate of COVID-19 infection and the death toll is rising daily. Although we just present this notion, the coefficient can update on-the-fly to allow flexible adjustment in every week, to evaluate and master the surgical reality at the hospital. Especially true for areas with more emerging infections.
More detailed information is that in the COVID-19 designated hospitals, the ward may be occupied or isolated and procedure volume may significantly decrease. Most elective surgery can be deferred beyond the pandemic period, but emergency surgery is still necessary. These hospitals can admit patients in a planned manner according to our prediction model.
In parallel, this model can also exert its effect in the public health field, data from multiple hospitals can be collected in real-time, and the CDC can assign the hospitalization according to the reality at each hospital, which can help to solve the backlog in the whole disease-endemic area rapidly.
Advantages and shortages
This is the first study discussed on the operative volume, distribution of cases, or capacity of a thoracic surgery departments in China to deliver surgical services in a real-world setting during this pandemic. As the escalating new COVID-19 cases found in the world, China has entered a next phase of the COVID-19 outbreak, we hope to share our experiences and discussed the challenges we faced. Our study is also the first to build a prediction model to calculate the time required for the backlog surgeries, which can also provide a basis for next step in the multicenter research.
However, there are several shortcomings in this study. Firstly, the sample size was collected only from one hospital, which is too small to generalize the conclusion in other situations during the pandemic. Secondly, Guangzhou is a city not severely affected by COVID-19 as Wuhan in China during the period which we extracted our data from. Thirdly, compared with cities on other countries, such as America, a relatively small number of COVID-19 patients admitted in our hospital (n=20) may account for a low risk of COVID-19 cross infection in our hospital, which can not be ignored when we quantify and qualify the capacity to resume surgery activity of a hospital. Fourthly, the available data only allow us to build a linear model instead of non-linear model, which may increase the uncertainty of model.
Many factors can be found to influence the model curve, such as blood supply, which can affect the stability of our model. Meanwhile, public health emergencies can also cause the change and recalculation of predicted curve. It is pointed that regular updates based on current situation is necessary, this is why we used the MySQL served as the relational database for continuously updated. Further studies are awaited, a multicentered study on surgery and hospital managements of the whole city or country is required.
Therefore, we encourage all the health care workers around the world to share their experience and perspectives on surgery in a real-world setting during the current pandemic to collectively mitigate the impact of COVID-19.
Conclusions
An understanding of thoracic operative case volume and distribution is essential in facilitating targeted interventions to strengthen surgical capacity in the time of COVID-19. A proper guideline is imperative to ensure access to safe, timely surgical care. Despite COVID-19 being a threat, by developing a scientific and effective management of hospital, it is possible to ensure optimal surgical safety during this crisis.
Acknowledgments
We sincerely thank all the medical staff who are fighting against this public health crisis.
Funding: This work was supported by the China National Science Foundation (Grant No.81871893), Key Project of Guangzhou Scientific Research Project (Grant No. 201804020030).
Footnote
Reporting Checklist: The authors have completed the MDAR reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-2883
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-2883
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-20-2883). JH serves as the Executive Editor-in-Chief of Journal of Thoracic Disease. WL serves as an unpaid editorial board member of Journal of Thoracic Disease from Apr 2018 to Apr 2021. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the First Affiliated Hospital of Guangzhou Medical University (No. 2020-94) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Coronavirus disease (COVID-19) pandemic. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019
- Puliatti S, Eissa A, Eissa R, et al. COVID-19 and urology: a comprehensive review of the literature. BJU Int 2020;125:E7-14. [Crossref] [PubMed]
- Søreide K, Hallet J, Matthews JB, et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg 2020;107:1250-61. [Crossref] [PubMed]
- Next steps on NHS response to COVID-19: Letters from Sir Simon Stevens and Amanda Pritchard. Available online: https://www.england.nhs.uk/coronavirus/publication/next-steps-on-nhs-response-to-covid-19-letter-from-simon-stevens-and-amanda-pritchard/
- COVID-19 and surgical procedures: a guide for patients. 2020. Available online: https://www.facs.org/covid-19/clinical-guidance/patient-guide
- Haddad FS. COVID-19 and orthopaedic and trauma surgery. Bone Joint J 2020;102-B:545-6. [Crossref] [PubMed]
- Hogan A. COVID-19 and emergency surgery. Br J Surg 2020;107:e180 [Crossref] [PubMed]
- Wexner SD, Cortés-Guiral D, Gilshtein H, et al. COVID-19: impact on colorectal surgery. Colorectal Dis 2020;22:635-40. [Crossref] [PubMed]
- COVIDSurg Collaborative. Global guidance for surgical care during the COVID-19 pandemic. Br J Surg 2020;107:1097-103. [Crossref] [PubMed]
- Hwee J, Chiew J, Sechachalam S. The impact of coronavirus disease 2019 (COVID-19) on the practice of hand surgery in Singapore. J Hand Surg Am 2020;45:536-41. [Crossref] [PubMed]
- Perkel JM. Why Jupyter is data scientists' computational notebook of choice. Nature 2018;563:145-6. [Crossref] [PubMed]
- Shander A, Goobie SM, Warner MA, et al. Essential role of patient blood management in a pandemic: a call for action. Anesth Analg 2020;131:74-85. [Crossref] [PubMed]
- Aminian A, Safari S, Razeghian-Jahromi A, et al. COVID-19 outbreak and surgical practice: unexpected fatality in perioperative period. Ann Surg 2020;272:e27-9. [Crossref] [PubMed]
- COVID-19: guidance for triage of non-emergent surgical procedures. 2020. Available online: https://www.facs.org/covid-19/clinical-guidance/triage
- COVID-19: good practice for surgeons and surgical teams. Available online: https://www.rcseng.ac.uk/standards-and-research/standards-and-guidance/good-practice-guides/coronavirus/
- COVID-19: what proportion are asymptomatic? 2020. Available online: https://www.cebm.net/covid-19/covid-19-what-proportion-are-asymptomatic/
- Yang W, Sirajuddin A, Zhang X, et al. The role of imaging in 2019 novel coronavirus pneumonia (COVID-19). Eur Radiol 2020;30:4874-82. [Crossref] [PubMed]
- Kumar D, Manuel O, Natori Y, et al. COVID-19: a global transplant perspective on successfully navigating a pandemic. Am J Transplant 2020;20:1773-9. [Crossref] [PubMed]
- Michaels MG, La Hoz RM, Danziger-Isakov L, et al. Coronavirus disease 2019: implications of emerging infections for transplantation. Am J Transplant 2020;20:1768-72. [Crossref] [PubMed]