
Clinical characteristics and outcomes of mechanically ventilated elderly patients in intensive care units: a Chinese multicentre retrospective study
Introduction
It is well-known that population aging is already taking place in most countries and regions of the world. The proportion of the world’s population aged 60 years or older increased from 8% in 1950 to 12% in 2013. The older population is also aging itself; the proportion of persons aged 80 years or older within the older population increased from 7% in 1950 to 14% in 2013. Twenty-three million persons aged 80 years or over were living in China in 2013 (1).
As the population ages and life expectancy increases, the number of elderly patients admitted to intensive care units (ICUs) is rapidly increasing in many countries (2-5) and has been estimated to rise considerably (3,4). Elderly patients currently account for 42–52% of ICU admissions and for almost 60% of all ICU days (3,6-8). A retrospective analysis in Australia and New Zealand found an annual increase of 5.6% in the number of very elderly (age ≥80 years) patients (3). The main reasons for ICU admission in elderly patients (age ≥65 years) are cardiovascular issues (23–24%) (7,9), respiratory issues (26–52%) (10-16), trauma (29%) (17), or sepsis (22–32%) (3,18-21). Invasive mechanical ventilation (MV) has become one of the most common treatments used in elderly patients admitted to the ICU. About half or more of elderly patients in the ICU need MV (3,7,9-11,14-16,18,21-23). With our aging population, the number of patients with MV will steadily increase, with a projected 80% increase by 2026 when compared to 2000 (24).
Although many clinical studies have described the clinical characteristics and outcomes of elderly patients in the ICU, there is still a lack of information on the prognosis of mechanically ventilated elderly patients in the ICU. This information is important in clinical practice when deciding whether to transfer the patient to an ICU, and whether to initiate or withdraw MV. The aim of this study is to describe clinical characteristics and outcomes of mechanically ventilated elderly patients in the ICU.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/ jtd-20-2748).
Methods
Study setting and design
This retrospective observational cohort study was carried out in fourteen ICUs of thirteen tertiary teaching hospitals in Beijing between January 2012 and June 2013.
Among the fourteen participating ICUs, ten were medical-surgical ICUs, two were surgical ICUs, one was a respiratory ICU, and one was a medical ICU. The number of ICU beds ranged from 8 to 20 during the study period. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This retrospective study was approved by the Research Ethics Boards of all participating institutions (approval number: 2019FXHEC-KY167), with a waiver of informed consent.
Study population
Patients who were admitted to the ICU and received at least 24 hours of invasive MV within the first 48 hours of ICU stay were eligible. Patients were excluded if they were less than 18 years old, had incomplete data sets, were diagnosed with neuromuscular disease, required chronic MV prior to hospital admission, or were transferred from other facilities and had already been intubated or tracheotomised. A patient was considered as one case if they were admitted to the ICU several times during the study period, and only data from the first ICU admission was analysed.
In our study, patients aged 65 years and older at the time of hospital admission, were defined as the elderly, and the cohort was divided into three age groups for analysis: under 65, 65–79, and 80 years and older. Those under 65 years of age were used as a reference population.
Data collection
For every enrolled patient, the following data were recorded: demographic and epidemiological characteristics; reason for ICU admission; comorbidities; severity of illness; primary reason for MV; MV parameters and settings; sedatives, analgesics, and neuromuscular blockers used during MV; total duration of MV; ventilator-free days (25); the occurrence of successful weaning within 28 days; ICU and hospital length of stay (LOS); ICU and hospital costs; complications of MV; the occurrence of withholding or withdrawing life-sustaining treatments; and discharge destination. To obtain survival data after hospital discharge, we contacted survivors, their relatives, or their general practitioner or nursing homes by phone.
Severity of illness was assessed using the Acute Physiology and Chronic Health Evaluation (APACHE) II score (26). The severity of illness as rated by the APACHE II score was given with and without age points to illustrate the impact that age has on the score.
Outcomes of interest
The primary outcome was hospital mortality. Secondary outcomes included the total duration of MV, ICU and hospital LOS, and ICU and 60-day mortality rates.
Statistical analysis
Statistical analyses were carried out using SPSS 21.0 (SPSS Inc., Chicago, Illinois, USA). Data were expressed as the mean ± standard deviation (SD) for normally distributed continuous variables, the median [interquartile range (IQR)] for non-normally distributed variables, and the number (percentage) for categorical variables. Continuous variables were compared using the Kruskal-Wallis test or the Mann-Whitney U test. Categorical variables were compared using the chi-square or Fisher’s exact tests. Logistic regression analysis was used to determine risk factors for the ICU, hospital, and 60-day mortality rates. Variables were introduced into the model based on clinical and statistical significance (P value <0.2 on univariate analysis). We then performed three separate multivariate logistic regression analyses using a forward selection procedure to determine risk factors for ICU mortality (first analysis), hospital mortality (second analysis), and 60-day mortality (third analysis). We defined cut-off points for ICU LOS and total duration of MV to create a binary dependent variable: seven days for ICU stay and five days for total duration of MV. These cut-off points were chosen because they were the median values for the variables. A two-sided P value <0.05 was considered statistically significant.
Results
Baseline characteristics
A total of 853 patients were included in this study. Of these, there were 328 patients under the age of 65 years (38.5%), 303 patients aged 65–79 years (35.5%), and 222 patients aged 80 years and older (26.0%). Table 1 presents baseline demographics and clinical characteristics of mechanically ventilated patients in the ICU. There were statistically significant differences in body mass index (BMI) and smoking history among the three age groups. However, significant differences were not found among the three age groups due to gender, past history of surgery, and non-invasive mechanical ventilation (NIMV) before ICU admission.

Full table
With advancing age, patients admitted to the ICU were more likely to be from the medical ward (from 13.1% in the age group under 65 years to 32.4% in the age group of 80 years and older), while the proportion from the surgical ward decreased (54.0% in the age group under 65 years to 30.6% in the age group of 80 years and older).
With increasing age, the prevalence of some pre-existing comorbidities such as hypertension, chronic renal failure, chronic heart failure, chronic obstructive pulmonary disease (COPD), cancer, and stroke significantly increased. The prevalence of having two or more comorbidities also increased with age (P<0.001). In the two older age groups, more than 50% of patients had two or more comorbidities.
ICU hospitalization characteristics
Table 2 presents the hospitalization characteristics of mechanically ventilated patients in the ICU. The APACHE II scoring system was used to assess the severity of illness in patients admitted to the ICU, both with and without age points. There was a significant difference among the three age groups with median APACHE scores of 13 points (IQR, 8–19) in the age group under 65 years, 18 points (IQR, 12–24) in the age group of 65–79 years, and 19 points (IQR, 13–24) in the age group 80 years and older (P<0.001). When compared with patients aged less than 65 years, the two older age groups had higher APACHE scores (both P<0.001). After filtering out the age points, there was still a significant difference in APACHE scores between the age group under 65 years and the age group of 80 years and older [11 points (IQR, 6–17) vs. 14 points (IQR, 8–19), P=0.034]; however, there was not a significant difference between the age group under 65 years and the age group of 65–79 years (P=0.114).

Full table
We found significant differences among the three age groups (P<0.001) in the principal reason for MV: pneumonia (31.1%) was the most prevalent reason for the initiation of MV in the age group of 80 years and older, followed by postoperative status (23.4%), as well as COPD or asthma (10.4%) and congestive heart failure (10.4%). However, the most prevalent reason for MV in the age group under 65 years old and the age group between 65 and 79 years old was postoperative status (48.2% and 37.0%, respectively), followed by pneumonia (11.9% and 17.2%, respectively) and acute respiratory distress syndrome (ARDS; 9.8% and 10.9%, respectively).
Arterial blood gas analysis before MV in the three age groups showed statistical differences in partial pressure of oxygen in arterial blood/fraction of inspired oxygen (PaO2/FiO2) ratio (P=0.026), partial pressure of carbon dioxide (PaCO2, P<0.001), and pulse oxygen saturation (SpO2, P<0.001), but this was not observed in arterial pH (P=0.126).
The combination of synchronized intermittent mandatory ventilation and pressure support mode (SIMV + PSV) was the most preferred mode of MV in the three age groups (39.0%, 43.6%, and 34.2% in the under 65 years age group, 65–79 years old group, and 80 years and older group, respectively). However, the MV mode was not significantly different among the three age groups (P=0.404).
Regarding the management of patients during MV, significant differences were found in tidal volume (VT; P<0.001) and the use of analgesics (P<0.001) among the three age groups. In the whole cohort, more than 70% (71.9%) of patients were ventilated with a VT <8 mL/kg of predicted bodyweight, and in the third age group, the proportion of patients with a VT <8 mL/kg of predicted bodyweight was the highest (76.1%). The proportion of patients using analgesics in the three age groups decreased with age (72.9% in the age group under 65 years to 47.7% in the age group of 80 years and older). There were no significant differences in the median levels of positive end expiratory pressure (PEEP) and platform pressure among the three age groups, or in the use of sedatives and neuromuscular blockers (all P>0.05).
Clinical courses and outcomes
Table 3 presents the clinical courses and outcomes in each of the three age groups. There were statistically significant differences in the total duration of MV (P<0.001), ventilator-free days (P<0.001), and successful weaning rate within 28 days (P<0.001) among the three age groups. As shown in Table 3, it can be clearly seen that compared with patients in the group aged 65–79 years and the group aged under 65 years, the total MV time of patients in the age group of 80 years and older increased significantly, while the ventilator-free days, and successful weaning rate within 28 days decreased significantly. Only the total duration of MV between the two older age groups had no statistically significant difference [135 (IQR, 59–280) vs. 165 (IQR, 67–404) hours, P=0.101].
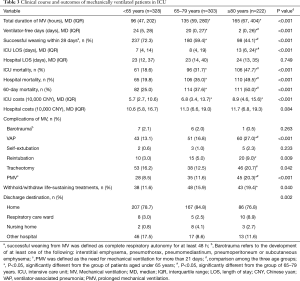
Full table
There was no statistically significant difference in the hospital LOS among the three age groups (P=0.749). However, the difference in the ICU LOS did differ significantly (P<0.001). In the group of patients aged 80 and older, the ICU LOS was 13 days (IQR, 6–24 days), as compared with 8 days (IQR, 4–19 days) for patients aged 65–79 years (P=0.005) and 7 days (IQR, 4–14 days) for patients aged under 65 years (P<0.001).
Mortality rates in the ICU, hospital, and at 60 days significantly increased with age. In the age group of 80 years and older, the hospital mortality rate was 49.5%, which was significantly different from the 19.8% rate for the age group under 65 years (P<0.001) and the 35.0% rate for the age group of 65–79 years (P=0.001). There was also a significant difference in the hospital mortality rate between the age group 65–79 years and the age group under 65 years (P<0.001). The same was true for ICU mortality and 60-day mortality rates.
There was no statistically significant difference in hospital costs among the three age groups (P=0.084). However, ICU costs did differ significantly (P<0.001). The ICU costs were higher in the age group of 65–79 years (with a median of 68,000 CNY) and the age group of 80 years and older (with a median of 89,000 CNY) than those in the age group under 65 years (with a median of 57,000 CNY; P=0.030 and P<0.001, respectively), but there was no significant difference between the two elderly groups (P=0.061).
Table 3 also shows the rate of events that occurred over the course of MV. The proportion of patients who required reintubation tended to be higher in the age group of 80 years and older. Furthermore, the rates of subsequent ventilator-associated pneumonia and the proportion of patients who underwent prolonged MV were significantly higher in the age group of 80 years and older (all P<0.01). In addition, the decision to withhold or withdraw life-sustaining treatments tended to be much more often in the age group of 80 years and older (19.4%). A considerable proportion of the 572 patients who survived the hospital were discharged home. Additionally, the proportion of patients that survived discharge and returned home in all three age groups was similar. However, in the age group of 80 years and older, nearly one-ninth (8.9%) of survivors were transferred to a respiratory care ward.
Univariate and multivariate logistic regression analyses
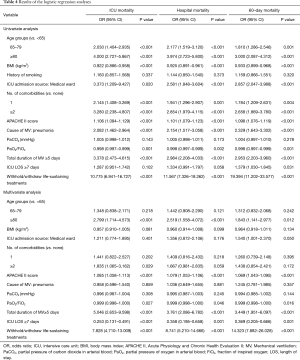
Table 4 presents the statistical results of univariate and multivariate analyses for ICU mortality, hospital mortality, and 60-day mortality. Multivariate logistic regression analysis had found that age, APACHE II score, PaO2/FiO2 ratio, total duration of MV, ICU LOS, and the decision to withhold/withdraw life-sustaining treatments were independent influence factors for ICU mortality, hospital mortality, and 60-day mortality. In addition, the number of comorbidities was also an independent risk factor for ICU mortality. Multivariate logistic regression analysis also showed that when compared with the reference group (under 65 years) and adjusted for other variables, the odds ratios of ICU death, hospitalization death and death within 60 days in patients aged 80 years and older were 2.799 (95% CI: 1.714–4.573), 2.519 (95% CI: 1.558–4.072) and 1.843 (95% CI: 1.141–2.977), respectively.
Full table
Discussion
In this multicentre retrospective study, our main findings were that the elderly account for a major proportion of adult patients receiving MV in ICU. Mechanically ventilated elderly patients have a lower ICU, hospital and 60-day survival, but the hospital LOS and hospital costs are similar to younger patients. Advanced age should be considered as an important independent risk factor for mortality rates of patients receiving MV in the ICU.
In recent decades, a few studies have shown that the proportion of elderly patients receiving MV treatment in ICUs reaches 25.4–50.5% (27-30). In our study, we found that this proportion of elderly patients was up to 61.5%, and the proportion of very elderly patients was up to 26.0%, which was significantly higher than in the previous studies. There are several reasons why this might be the case, including the following: first, it is well-known that population aging is taking place much more rapidly now in developing countries than it had in developed countries in the past. In particular, China is one of the fastest aging countries in the world (1). This demographic trend is bound to increase the demand for health care resources. Secondly, there is still a lack of well-defined thresholds for elderly patients, and the definition of the term “elderly” has varied from 65 to 75 years old (7,10,22,23,27,29-36). Therefore, the research results may differ.
As reported by others, acute respiratory failure was the most frequent indication for MV (27,28,30,37), accounting for 87.5% of the principal reason for MV for our total study group. There were statistically significant differences in the principal reason for MV among the three age groups (P<0.001). Compared with the other two age groups, very elderly (age ≥80 years) patients were more likely to receive MV for medical indications (pneumonia, aspiration, and congestive heart failure) and less likely to receive MV for postoperative reasons and trauma. Esteban et al. (27) also found that older patients (age >70 years) were ventilated because of cardiac diseases (heart failure and cardiac arrest) and fewer were ventilated because of coma, ARDS and trauma. The reasons for this may be explained as follows: first, we found that with age, patients admitted to the ICU were more likely to come from the medical ward, while the proportion coming from surgical wards declined. Secondly, in our study, we found that the prevalence of having two or more comorbidities increased with age in patients with MV in the ICU (P<0.001). Having several organ dysfunctions and failures, such as cardiovascular and respiratory dysfunction and failure increased the relative risk of receiving MV. Multivariate analysis revealed that factors such as increasing age, New York Heart Association (NYHA) functional classification III or IV, neurologic and respiratory reasons for admission, emergency surgery; pneumonia, and lower Glasgow Coma Score were associated with the use of MV (38).
Unlike other studies (28,38), our study shows that SIMV + PSV was the main invasive ventilatory mode in the whole group as well as in all three age groups, followed by assist-control ventilation and PSV. In fact, this may reflect heterogeneity in the selection of ventilatory modes in different ICUs and countries (37,38). However, there was no statistically significant difference in ventilatory modes among the three age groups (P=0.404). In our cohort, the median VT setting was 7.26 mL/kg of predicted bodyweight (IQR, 6.37–8.11), a value lower than that described in some studies (28,37,38). More than 70% (71.9%) of patients were ventilated with a VT <8 mL/kg of predicted bodyweight, and this proportion increased with age. This value is greater than the 48.4% reported by Metnitz et al. in a multinational cohort (38). This may be related to the median PaO2/FIO2 ratios being <200 in the three age groups. Metnitz et al. found that patients with the lowest PaO2/FIO2 ratios were ventilated more often with tidal volumes <8 mL/kg of body weight, than patients with higher PaO2/FiO2 ratios (38).
Age has always been considered to be a factor in increased ICU resource utilization. Our findings may support this. In this study, we found statistically significant differences in duration of MV, length of ICU stay, and ICU costs among the three age groups. However, this does not mean that the length of hospital stays and hospital costs of elderly patients have increased significantly. The association between age and hospital costs in patients receiving MV was studied by Chelluri et al. (39). They found that daily and total hospital costs were lower in older patients. They suggest that the lower resource use for older patients may be related to a preference for less aggressive care by elderly patients and their families or by healthcare providers. We also support this view because we found that the decision to withhold or withdraw life-sustaining treatments tended to be much more often with aging. Moreover, Turnbull et al. (40) have also shown a higher rate of limiting life support among older patients.
Our results suggest that ICU mortality, hospital mortality, and 60-day mortality of ventilated elderly patients in the ICU are significantly elevated. Age was strongly associated with mortality rates of mechanically ventilated elderly patients in the ICU, and remained a strong predictor of mortality even after adjusting for other variables. Our study adopted the most widely used criteria to define an elderly population, and analyzed the relationship between age and ICU mortality, hospital mortality and 60-day mortality in the three age intervals. We present the results of a quantitative assessment of increased risk of death associated with specific age intervals (≥80 years).
To our knowledge, this is the first study in China to evaluate the characteristics and outcomes in elderly patients (≥65 years) receiving MV in the ICU. However, we also are aware of several limitations of our study. First, this study is a retrospective study, and the data were obtained in 2012–2013, which may impose temporal limitations on the applicability of this data set. Second, we only evaluated ICU mortality, hospital mortality, and 60-day mortality, without discussing long-term mortality, activities of daily living (ADL), and quality of life (QOL) after discharge, because we did not collect relevant data. Future studies should focus on long-term mortality, physical rehabilitation, and QOL of elderly patients discharged from the hospital. Third, we did not collect data on clinical and laboratory variables during the period of MV, such as changes in blood pressure, heart rate, respiratory rate, pH, PaO2, PaCO2, SpO2, and ventilator parameters. Thus, we cannot further assess the effectiveness of MV.
Conclusions
In conclusion, the results obtained in the present study indicate that the elderly patients constitute a major proportion of adult patients receiving MV in the ICU.
The elderly mechanically ventilated patients (≥65 years) have a higher ICU and hospital mortality, but the hospital LOS and hospital costs are similar to younger patients. Advanced age should be considered as a significant independent risk factor for hospital mortality of mechanically ventilated ICU patients. Evaluating the clinical characteristics and outcomes of elderly mechanically ventilated patients has become important in terms of the effective use of limited medical resources and making decisions for clinicians, patients and their families.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-20-2748
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-20-2748
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ jtd-20-2748). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This retrospective study was approved by the Research Ethics Boards of all participating institutions (approval number: 2019FXHEC-KY167), with a waiver of informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- United Nations, Department of Economic and Social Affairs, Population Division (2013). World Population Ageing 2013. ST/ESA/SER.A/348 2013. Available online: http://www.un.org/en/development/desa/population/publications/ageing/WorldPopulationAgeing2013.shtml. Accessed 02 Mar 2019.
- Wunsch H, Linde-Zwirble WT, Harrison DA, et al. Use of intensive care services during terminal hospitalizations in England and the United States. Am J Respir Crit Care Med 2009;180:875-80. [Crossref] [PubMed]
- Bagshaw SM, Webb SA, Delaney A, et al. Very old patients admitted to intensive care in Australia and New Zealand: a multi-centre cohort analysis. Crit Care 2009;13:R45. [Crossref] [PubMed]
- Laake JH, Dybwik K, Flaatten HK, et al. Impact of the post-World War II generation on intensive care needs in Norway. Acta Anaesthesiol Scand 2010;54:479-84. [Crossref] [PubMed]
- Nguyen YL, Angus DC, Boumendil A, et al. The challenge of admitting the very elderly to intensive care. Ann Intensive Care 2011;1:29. [Crossref] [PubMed]
- Marik PE. Management of the critically ill geriatric patient. Crit Care Med 2006;34:S176-82. [Crossref] [PubMed]
- Fuchs L, Chronaki CE, Park S, et al. ICU admission characteristics and mortality rates among elderly and very elderly patients. Intensive Care Med 2012;38:1654-61. [Crossref] [PubMed]
- Docherty A, Lone N, Anderson N, et al. Epidemiology and outcomes of older patients admitted to Scottish intensive care units: a national database linkage study. Lancet 2015;385:S33. [Crossref] [PubMed]
- Ball IM, Bagshaw SM, Burns KE, et al. Outcomes of elderly critically ill medical and surgical patients: a multicentre cohort study. Can J Anaesth 2017;64:260-9. [Crossref] [PubMed]
- Sacanella E, Pérez-Castejón JM, Nicolás JM, et al. Mortality in healthy elderly patients after ICU admission. Intensive Care Med 2009;35:550-5. [Crossref] [PubMed]
- Tabah A, Philippart F, Timsit JF, et al. Quality of life in patients aged 80 or over after ICU discharge. Crit Care 2010;14:R2. [Crossref] [PubMed]
- Heyland D, Cook D, Bagshaw SM, et al. The Very Elderly Admitted to ICU: A Quality Finish? Crit Care Med 2015;43:1352-60. [Crossref] [PubMed]
- Tripathy S, Mishra JC, Dash SC. Critically ill elderly patients in a developing world--mortality and functional outcome at 1 year: a prospective single-center study. J Crit Care 2014;29:474.e7-13. [Crossref] [PubMed]
- Ball IM, Bagshaw SM, Burns KE, et al. A clinical prediction tool for hospital mortality in critically ill elderly patients. J Crit Care 2016;35:206-12. [Crossref] [PubMed]
- Le Borgne P, Maestraggi Q, Couraud S, et al. Critically ill elderly patients (>/=90 years): Clinical characteristics, outcome and financial implications. PLoS One 2018;13:e0198360 [Crossref] [PubMed]
- Lerolle N, Trinquart L, Bornstain C, et al. Increased intensity of treatment and decreased mortality in elderly patients in an intensive care unit over a decade. Crit Care Med 2010;38:59-64. [Crossref] [PubMed]
- Becker S, Müller J, de Heer G, et al. Clinical characteristics and outcome of very elderly patients >/=90 years in intensive care: a retrospective observational study. Ann Intensive Care 2015;5:53. [Crossref] [PubMed]
- Heyland DK, Garland A, Bagshaw SM, et al. Recovery after critical illness in patients aged 80 years or older: a multi-center prospective observational cohort study. Intensive Care Med 2015;41:1911-20. [Crossref] [PubMed]
- Heyland DK, Stelfox HT, Garland A, et al. Predicting Performance Status 1 Year After Critical Illness in Patients 80 Years or Older: Development of a Multivariable Clinical Prediction Model. Crit Care Med 2016;44:1718-26. [Crossref] [PubMed]
- Orsini J, Butala A, Salomon S, et al. Prognostic factors associated with adverse outcome among critically ill elderly patients admitted to the intensive care unit. Geriatr Gerontol Int 2015;15:889-94. [Crossref] [PubMed]
- Mukhopadhyay A, Tai BC, See KC, et al. Risk factors for hospital and long-term mortality of critically ill elderly patients admitted to an intensive care unit. Biomed Res Int 2014;2014:960575 [Crossref] [PubMed]
- Farfel JM, Franca SA, Sitta Mdo C, et al. Age, invasive ventilatory support and outcomes in elderly patients admitted to intensive care units. Age Ageing 2009;38:515-20. [Crossref] [PubMed]
- Khouri T, Kabeshova A, Annweiler C, et al. Amount of care per survivor in young and older patients hospitalized in intensive care unit: a retrospective study. J Gerontol A Biol Sci Med Sci 2014;69:1291-8. [Crossref] [PubMed]
- Needham DM, Bronskill SE, Calinawan JR, et al. Projected incidence of mechanical ventilation in Ontario to 2026: Preparing for the aging baby boomers. Crit Care Med 2005;33:574-9. [Crossref] [PubMed]
- Schoenfeld DA, Bernard GR. ARDS Network. Statistical evaluation of ventilator-free days as an efficacy measure in clinical trials of treatments for acute respiratory distress syndrome. Crit Care Med 2002;30:1772-7. [Crossref] [PubMed]
- Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med 1985;13:818-29. [Crossref] [PubMed]
- Esteban A, Anzueto A, Frutos-Vivar F, et al. Outcome of older patients receiving mechanical ventilation. Intensive Care Med 2004;30:639-46. [Crossref] [PubMed]
- Esteban A, Anzueto A, Frutos F, et al. Characteristics and outcomes in adult patients receiving mechanical ventilation: a 28-day international study. JAMA 2002;287:345-55. [Crossref] [PubMed]
- Lieberman D, Nachshon L, Miloslavsky O, et al. Elderly patients undergoing mechanical ventilation in and out of intensive care units: a comparative, prospective study of 579 ventilations. Crit Care 2010;14:R48. [Crossref] [PubMed]
- Añon JM, Gómez-Tello V, González-Higueras E, et al. Prognosis of elderly patients subjected to mechanical ventilation in the ICU. Med Intensiva 2013;37:149-55. [PubMed]
- Torres OH, Francia E, Longobardi V, et al. Short- and long-term outcomes of older patients in intermediate care units. Intensive Care Med 2006;32:1052-9. [Crossref] [PubMed]
- Su KC, Tsai CC, Chou KT, et al. Spontaneous breathing trial needs to be prolonged in critically ill and older patients requiring mechanical ventilation. J Crit Care 2012;27:324.e1-7. [Crossref] [PubMed]
- Boumendil A, Somme D, Garrouste-Orgeas M, et al. Should elderly patients be admitted to the intensive care unit? Intensive Care Med 2007;33:1252. [Crossref] [PubMed]
- Hennessy D, Juzwishin K, Yergens D, et al. Outcomes of elderly survivors of intensive care: a review of the literature. Chest 2005;127:1764-74. [Crossref] [PubMed]
- Zhu Y, Yin H, Zhang R, et al. Gastric versus postpyloric enteral nutrition in elderly patients (age >/=75 years) on mechanical ventilation: a single-center randomized trial. Crit Care 2018;22:170. [Crossref] [PubMed]
- Pan CX, Platis D, Maw MM, et al. How Long Does (S)He Have? Retrospective Analysis of Outcomes After Palliative Extubation in Elderly, Chronically Critically Ill Patients. Crit Care Med 2016;44:1138-44. [Crossref] [PubMed]
- Esteban A, Anzueto A, Alía I, et al. How is mechanical ventilation employed in the intensive care unit? An international utilization review. Am J Respir Crit Care Med 2000;161:1450-8. [Crossref] [PubMed]
- Metnitz PG, Metnitz B, Moreno RP, et al. Epidemiology of mechanical ventilation: analysis of the SAPS 3 database. Intensive Care Med 2009;35:816-25. [Crossref] [PubMed]
- Chelluri L, Mendelsohn AB, Belle SH, et al. Hospital costs in patients receiving prolonged mechanical ventilation: does age have an impact? Crit Care Med 2003;31:1746-51. [Crossref] [PubMed]
- Turnbull AE, Lau BM, Ruhl AP, et al. Age and decisions to limit life support for patients with acute lung injury: a prospective cohort study. Crit Care 2014;18:R107. [Crossref] [PubMed]


