Safety and feasibility of uniportal video-assisted thoracoscopic uncommon segmentectomy
Introduction
In recent years, opportunities for lung segmentectomy for early-stage lung cancer with ground glass opacities and small nodules have been increasing (1). Segmentectomy is also an effective surgical procedure for frail cases that cannot tolerate radical surgery for primary lung cancer and cases with metastatic tumors near the hilum. Segmentectomy is usually categorized into common (simple) and uncommon (complex) segmentectomy, and uncommon segmentectomy is technically more complicated because blood vessels and bronchi need to be identified to the periphery and dissected, and there are multiple intersegmental planes to be separated.
Rocco first reported Uniportal video-assisted thoracoscopic surgery (U-VATS) for wedge resection in 2004 (2). Gonzalez-Rivas first reported single-incision VATS lobectomy in 2012 (3,4), and afterwards reported U-VATS segmentectomy (5). The potential benefits of U-VATS reported so far are wound pain reduction, neuralgia reduction, and cosmetic aspects (6-10). However, U-VATS has some difficulties compared with multiportal VATS (M-VATS) because the angle of the forceps is limited, and the stapler is inserted in only one direction. Therefore, there are concerns that uncommon segmentectomy by U-VATS will have some technical problems and increase the risk.
This study aimed to identify the safety and feasibility of U-VATS uncommon segmentectomy compared with U-VATS common segmentectomy and M-VATS uncommon segmentectomy.
We present the following article in accordance with the STROBE reporting checklist (available at http://dx.doi.org/10.21037/jtd-21-292).
Methods
Patient selection
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of Maebashi Red Cross Hospital (NO.: 2020-52), and individual patient consent for this retrospective analysis was waived.
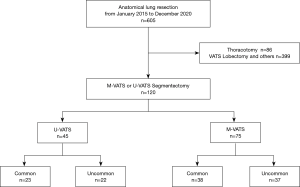
We retrospectively reviewed the medical records of patients who underwent VATS segmentectomy from January 2015 to December 2020. Of them, 45 patients underwent U-VATS and 75 patients underwent M-VATS, and each was classified into common or uncommon segmentectomy (Figure 1). Uncommon segmentectomy was defined as any segmentectomy other than segmentectomies of the lingual, basilar, or superior segment of the lower lobe (S6), and the upper division of the left upper lobe (11).
All patients in our department, except for cases with contrast agent allergy, underwent preoperative three-dimensional computed tomography (3D-CT) angiography and bronchography to image bronchovascular structures and tumor location and determine the resection line.
In our department, the standard curative surgery for primary lung cancer is lobectomy with systemic lymph node dissection. In patients who underwent intentional segmentectomy for primary lung cancer, clinical stage 0-IA1 (Tis-1aN0M0) was confirmed by careful preoperative staging with CT and/or FDG-PET. For patients who could not tolerate radical surgery due to complications and poor pulmonary function, segmentectomy was also performed as reduction surgery. In patients with metastatic lung tumors, segmentectomy was performed only when it was difficult to secure enough margin in wedge resection due to the location and size of tumor.
Postoperative complications were evaluated with the Common Terminology Criteria for Adverse Events version 5.0. The major complications were defined as requiring additional treatment.
M-VATS was performed by three senior surgeons, and U-VATS was performed by two of them. U-VATS was started in February 2019 and the surgical procedure was decided by the surgeon.
The study was approved by the institutional ethics board of Maebashi Red Cross Hospital (NO.:2020-52), and individual patient consent for this retrospective analysis was waived.
Procedure for U-VATS
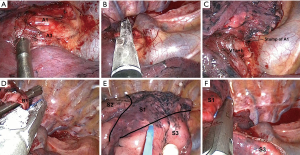
Surgery was carried out under general anesthesia in all cases, with the patient in the lateral decubitus position under differential lung ventilation. The operator always stood on the ventral side and the assistant on the dorsal side of the patient. A 3.5–4.0-cm skin incision was made in the fourth intercostal anterior axillary line for right upper lobectomy or the fifth intercostal anterior axillary line for other types of surgery and an XS Alexis wound retractor (Applied Medical, Rancho Santa Margarita, CA, USA) was fitted. Either a 5-mm or 10-mm 30º degree thoracoscope was immobilized on the dorsal side of the wound margin, with the ventral side providing space for the operator to manipulate the scope. Vessel and bronchial transection were in principle carried out with an automated suturing device, but suture ligation with 3-0 silk was performed if required by the vessel diameter. The inflation-deflation technique was normally used for segment identification. From May 2020, indocyanine green (ICG) was administered intravenously and an infrared thoracoscope was also used for observations. In almost all cases, intersegmental division was accomplished using only an automated suturing device, but for some patients a cautery was used where necessary. The chest drain was placed from the ventral side of the wound. As an example, detailed procedures for right apical segmentectomy (S1) are shown in Figure 2.
Procedure for M-VATS
Three or four ports were used, and XXS Alexis wound retractors were fitted to a 2.0-cm skin incision on the fourth intercostal anterior axillary line and a 1.5-cm skin incision on the sixth intercostal anterior axillary line. A 10-mm flexible camera was inserted via the 1.5-cm skin incision on the sixth intercostal anterior axillary line. When four ports were used, an additional 15-mm skin incision was made in the seventh intercostal space below the scapula for use as the assistant’s port. Segmentectomy was performed in the same way as in U-VATS. The chest drain was placed via the port on the sixth intercostal anterior axillary line.
Statistical analysis
Fisher’s exact test was applied for comparing categorical variables. The t-test was applied for comparing continuous variables. A P<0.05 was considered statistically significant. All statistical analyses were performed with EZR (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics and segmentectomy performed by U-VATS and M-VATS
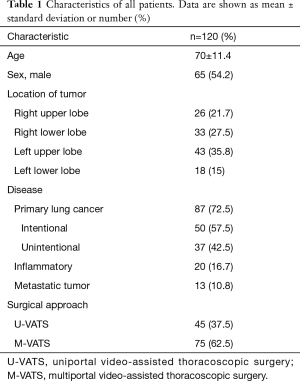
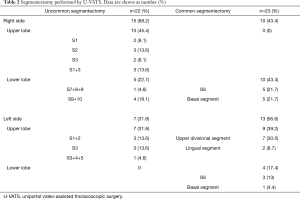
The characteristics of all patients are shown in Table 1. There were 87 (72.5%) cases of primary lung cancer, 50 (57.5%) of which underwent intentional segmentectomy. The details of segmentectomies performed by U-VATS and M-VATS are shown in Tables 2 and 3. In the U-VATS group, there were no uncommon segmentectomies of the left lower lobe.
Full table
Full table
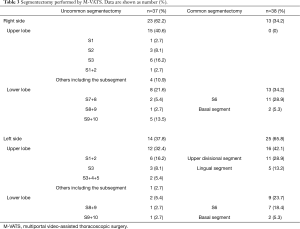
Full table
Comparison between common and uncommon segmentectomies in U-VATS
Comparison of patient characteristics and perioperative outcomes between the common and uncommon segmentectomy groups in U-VATS are shown in Table 4. There were no significant differences between the groups in patient characteristics including age, sex, and disease. No significant intraoperative bleeding (bleeding from the pulmonary artery or vein that could be managed under VATS) and no conversions to thoracotomy were observed in the uncommon segmentectomy group, and the mean intraoperative blood loss was significantly less in the uncommon segmentectomy group than in the common segmentectomy group (70±115 mL in common vs. 15±26 mL in uncommon, P=0.034). There were no significant differences in the duration of postoperative drainage and the duration of postoperative hospitalization.
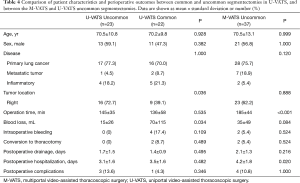
Full table
Postoperative complications occurred in 1 patient (4.3%) in the common segmentectomy group: who had atrial fibrillation. On the other hand, in the uncommon segmentectomy group, 3 patients (13.6%) had postoperative complications: prolonged air leak in 1, delayed pneumothorax in 1 and hypoxemia in 1. There was no significant difference in the rate of postoperative complications between the groups (P=0.346).
Comparison between M-VATS and U-VATS uncommon segmentectomies
Comparisons of patient characteristics and perioperative outcomes between the M-VATS and U-VATS uncommon segmentectomies are shown in Table 4. There were no significant differences between the groups in patient characteristics including age, sex, disease and tumor location. Operation time was significantly shorter in the U-VATS group than in the M-VATS group (145±35 vs. 185±44 min, P<0.001). There were no significant differences in blood loss, intraoperative bleeding and duration of postoperative drainage. The duration of postoperative hospitalization was significantly shorter in the U-VATS group than in the M-VATS group (3.1±1.6 vs. 4.2±1.8 days, P=0.02).
Four patients (10.8%) in the M-VATS group had postoperative complications, including prolonged air leak in 1, delayed pneumothorax in 2 and hypoxemia in 1. There was no significant difference in the rate of postoperative complications between the groups (P=1.000).
Discussion
This study showed that the perioperative results of U-VATS uncommon segmentectomy are equivalent to those of U-VATS common segmentectomy or M-VATS uncommon segmentectomy and can be performed safely.
Although the standard radical surgery for primary lung cancer is still lobectomy (12), ground glass opacity (GGO) on thin-section CT has been shown to have a very good prognosis, and sublobar resection has become widespread (13). For metastatic lung tumors and inflammatory disease, sublobar resection is also performed. Segmentectomy can be performed even for lesions that are not present on the periphery of the lung and cannot be palpated, while ensuring sufficient margin, combined with preoperative 3D-CT simulation. However, uncommon segmentectomy is technically challenging in terms of treating fragile vessels and peripheral bronchi and creating several intersegmental planes. Handa et al. evaluated operative and postoperative outcomes of complex and simple segmentectomies and showed that only median operative time (180 vs. 143.5 min, P<0.0001) was significantly longer in the complex group (11). Xie et al. also reported that in both U-VATS (P<0.001) and M-VATS (P=0.011), operation time was significantly longer in the complex segmentectomy group than in the simple segmentectomy group (14). Moreover, in a randomized controlled trial to confirm the noninferiority of segmentectomy to lobectomy (JCOG0802/WJOG4607L), complex segmentectomy was a predictor of air leak and empyema (grade ≥2) (odds ratio, 2.07; 95% CI, 1.11–3.88; P=0.023) (15). This may be due to the procedure of creating a fissure, which included cautery, stapler and cautery, or stapler. We mainly use a stapler to create an intersegmental plane, and we previously reported no significant differences in perioperative results including blood loss, operation time, drainage, hospitalization and morbidity between common and uncommon segmentectomy group (16).
Several papers comparing the results of segmentectomy by M-VATS and U-VATS have been reported, all of which were comparable (14,17,18). A technical difficulty with U-VATS is that the angle of the forceps and stapler insertion is limited. In U-VATS, the camera is basically fixed to the dorsal side of the wound edge to secure the operator’s space on the ventral side, and a curved long suction tube is used to avoid interference of the forceps. By arranging them in the optimal position inside and outside the thoracic cavity, smooth operation is possible. Ligation with 3-0 silk is also useful for vessel dissection when a stapler is not adequate in segmentectomy. Before creating the intersegmental plane, the distal bronchial and vessel stumps are fully dissected from the surrounding tissue to the periphery, creating the space for stapler insertion. When inserting the stapler, it is important to move the lungs significantly to match the stapler insertion angle.
Cheng et al. reported about the learning curve for U-VATS segmentectomy, showing that an experienced surgeon can achieve a relatively stable level after 33 cases (19). In the present study, operation time was significantly shorter in the U-VATS uncommon segmentectomy group than in the M-VATS uncommon segmentectomy group. Possible reasons include the following. Firstly, U-VATS was started in 2019, and there may have been an effect due to differences in experience and skill when operators who had previously mastered segmentectomy by performing it numerous times in M-VATS shifted to U-VATS. Secondly, in U-VATS the camera is inserted from the same angle as the operator, meaning that its field of view is consistent with the operator’s viewpoint, and this gives the operator a sense similar to conducting open-chest surgery. Finally, the use of forceps and energy devices designed and developed for U-VATS enabled the operator to carry out dissection effectively and rapidly.
This study has several weaknesses because of its retrospective design. The total number of cases is relatively small, so a prospective and multicenter study is required. In addition, the study period was too short to evaluate long-term outcomes. In particular, it is necessary to examine the long-term oncologic results of cases of primary lung cancer.
In conclusion, common and uncommon segmentectomies can be achieved in U-VATS with similar results. In the present study, similar perioperative results such as blood loss and the postoperative complication rate could be observed between U-VATS and M-VATS. Moreover, U-VATS shortened the operation time and postoperative hospitalization in uncommon segmentectomy compared with M-VATS. U-VATS is a safe and useful approach to perform uncommon segmentectomy.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at http://dx.doi.org/10.21037/jtd-21-292
Data Sharing Statement: Available at http://dx.doi.org/10.21037/jtd-21-292
Peer Review File: Available at http://dx.doi.org/10.21037/jtd-21-292
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jtd-21-292). HI serves as an unpaid editorial board member of Journal of Thoracic Disease from Aug 2020 to Jul 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the institutional ethics board of Maebashi Red Cross Hospital (NO.:2020-52), and individual patient consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Okada M, Koike T, Higashiyama M, et al. Radical sublobar resection for small-sized non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg 2006;132:769-75. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fiera E, et al. Single-incision video-assisted thoracoscopic lobectomy: initial results. J Thorac Cardiovasc Surg 2012;143:745-7. [Crossref] [PubMed]
- Gonzalez-Rivas D, Paradela M, Fernandez R, et al. Uniportal video-assisted thoracoscopic lobectomy: two years of experience. Ann Thorac Surg 2013;95:426-32. [Crossref] [PubMed]
- Hernandez-Arenas LA, Purmessur RD, Gonzalez-Rivas D. Uniportal video-assisted thoracoscopic segmentectomy. J Thorac Dis 2018;10:S1205-14. [Crossref] [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes. Eur J Cardiothorac Surg 2016;49:i37-41. [PubMed]
- Zhao R, Shi Z, Cheng S. Uniport video assisted thoracoscopic surgery (U-VATS) exhibits increased feasibility, non-inferior tolerance, and equal efficiency compared with multiport VATS and open thoracotomy in the elderly non-small cell lung cancer patients at early stage. Medicine (Baltimore) 2019;98:e16137 [Crossref] [PubMed]
- Dai F, Meng S, Mei L, et al. Single-port video-assisted thoracic surgery in the treatment of non-small cell lung cancer: a propensity-matched comparative analysis. J Thorac Dis 2016;8:2872-8. [Crossref] [PubMed]
- Akter F, Routledge T, Toufektzian L, et al. In minor and major thoracic procedures is uniport superior to multiport video-assisted thoracoscopic surgery? Interact CardioVasc Thorac Surg 2015;20:550-5. [Crossref] [PubMed]
- Yang X, Li M, Yang X, et al. Uniport versus multiport video-assisted thoracoscopic surgery in the perioperative treatment of patients with T1-3N0M0 non-small cell lung cancer: asystematic review and meta-analysis. J Thorac Dis 2018;10:2186-95. [Crossref] [PubMed]
- Handa Y, Tsutani Y, Mimae T, et al. Surgical outcomes of complex versus simple segmentectomy for stage I non-small cell lung cancer. Ann Thorac Surg 2019;107:1032-9. [Crossref] [PubMed]
- Ginsberg RJ, Rubinstein LV. Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung cancer study group. Ann Thorac Surg. 1995;60:615-22. [Crossref] [PubMed]
- Suzuki K, Koike T, Asakawa T, et al. A prospective radiological study of thin-section computed tomography to predict pathological noninvasiveness in peripheral clinical IA lung cancer (Japan Clinical Oncology Group 0201). J Thorac Oncol 2011;6:751-6. [Crossref] [PubMed]
- Xie D, Wu J, Gonzalez-Rivas D, et al. Uniportal versus multiportal video-assisted thoracoscopic surgery does not compromise the outcome of segmentectomy. Eur J Cardiothorac Surg 2021;59:650-7. [Crossref] [PubMed]
- Suzuki K, Saji H, Aokage K, et al. Comparison of pulmonary segmentectomy and lobectomy: safety results of a randomized trial. J Thorac Cardiovasc Surg 2019;158:895-907. [Crossref] [PubMed]
- Igai H, Kamiyoshihara M, Yoshikawa R, et al. The safety and feasibility of thoracoscopic uncommon pulmonary segmentectomy. J Thorac Dis 2019;11:2788-94. [Crossref] [PubMed]
- Han KN, Kim HK, Choi YH. Comparison of single port versus multiport thoracoscopic segmentectomy. J Thorac Dis 2016;8:S279-S286. [PubMed]
- Chen YY, Huang WL, Chang CC, et al. Uniportal versus multiportal thoracoscopic complex segmentectomy: propensity matching analysis. Ann Thorac Cardiovasc Surg 2020;11: Epub ahead of print. [Crossref] [PubMed]
- Cheng K, Zheng B, Zhang S, et al. Feasibility and learning curve of uniportal video-assisted thoracoscopic segmentectomy. J Thorac Dis 2016;8:S229-S234. [PubMed]