
Diagnosis for readmission of senile patients hospitalized with acute decompensated heart failure in different departments: a retrospective cross-sectional study
Introduction
Heart failure is associated with significant hospital admission rates, mortality, and costly health care expenditures, especially in the elderly. In American, congestive heart failure (CHF) will affect more than 8million people and cost $68.9 billion by 2030 (1-3). In China, the age-standardized prevalence is 1.10%, accounting for 12.1 million patients with heart failure, and the inpatient mean cost per-capita is $4,406.80 (4).
Despite advances in the treatment and management of heart failure and heart failure-related risk factors (5,6), nearly 25% of all patients hospitalized with heart failure are readmitted within 30 days after being discharged (7). Short-term hospital readmissions not only lead to a significant strain on the health care budget (8,9), but are also associated with increased risk of 180-day all-cause death (10,11). Therefore, efforts to reduce HF readmissions may be a reasonable target both for reducing overall expenses and improving the outcome of the patients.
In response to the aging Chinese society, dedicated geriatric departments have been widely established in hospitals at all levels. Elderly patients with acute or decompensated heart failure are often admitted in different wards (either the geriatric department or other departments). In general, the geriatric department tends to admit older patients who require longer stays than other departments in our hospital. Recent systematic reviews or studies (12,13) have focused on the demographics, comorbidities, behavior factors, and mortalities after heart failure. However, few reports have focused on departmental differences in heart failure admissions, and no studies to date have examined the readmission rates, medical expenditure, length of hospital stay, and the diagnosis for readmission in the different departments. Which kind of patients can benefit from geriatric department was not well known. Based on these information, triage senile patients will be more accurate. This current study investigated the characteristics and diagnosis for readmission after hospitalization of acute decompensated heart failure in senile patients admitted to different departments. We hypothesize that admissions to the geriatric department are associated with higher costs, longer hospital stays, and increased morbidity compared to admissions to other departments. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-433/rc).
Methods
Study design
A retrospective cross-sectional study was conducted on senile patients admitted to our hospital with a primary diagnosis of CHF exacerbation.
Setting
The study was conducted at The People’s Hospital of Sichuan Province, from January 2017 to December 2017.
Participants
Adults aged 80 years or more, with a prior diagnosis of CHF, were included in the study. Admissions related to chemotherapy were excluded, as these were largely planned admissions. Patients readmitted on the same day were considered a continuation of index admission and were also excluded.
Study size
All cases admitted to the hospital during the study period constituted the sample size. A total of 1,316 patients satisfied the inclusion criteria and were included in the analysis.
Definition of readmissions and CHF
The International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) was used to identify the primary discharge diagnoses of acute decompensated heart failure. The heart failure diagnosis was based on current or past clinical symptoms, signs or radiographic or echocardiography evidence of pulmonary congestion. Other diagnoses were grouped according to the ICD-10-CM codes.
Readmission was defined as any admission within 30 days of a prior admission, except those that were previously planned to be readmitted. Analysis was performed on the admission level, while considering that consecutively readmission may be excluded. The top 3 diagnosis for admission were evaluated to determine cause-specific readmissions.
Variables and data collection
Data related to demographic information (including age and sex), comorbidities (such as diabetes, renal disease, hypertension, coronary artery disease, stroke, vascular disease, and atrial fibrillation).
Echocardiography was performed using standard ultrasound equipment, left ventricular ejection fraction (LVEF) were measured using modified Simpson’s method. Blood sample was collected on admission. Brain natriuretic peptide (BNP) level was measured by standard radioimmunoassay. Costs and discharge disposition were collated. A review of the electronic medical record 30 days after discharge was performed to determine if any-cause readmissions had occurred.
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics Committee of The People’s Hospital of Sichuan Province (No. 2019034). Individual consent for this retrospective analysis was waived.
Statistical analysis
Descriptive statistics were utilized to compare patients, admissions, and hospital characteristics of readmissions in different wards. Student’s t-tests were performed for normally distributed continuous variables, and chi-square tests were used for categorical variables. Logistic regression was used to assess the relationship between potential predictors [age, gender, BNP, ejection fraction (EF), atrial fibrillation] for readmissions.
All statistical tests were completed with SPSS 22.0 for Windows, and two-tailed 95% confidence levels and a P value <0.05 was required to reject the null hypothesis.
Results
Of the 3,922 hospitalizations during the study period, 1,316 heart failure patients were re-hospitalized, including 893 who were admitted to geriatric department. The readmission rate was 33.55%.
Compared with other departments, readmissions to the geriatric department were associated with of a larger number of males (72.96% vs. 58.29%, P<0.0001), older patients (89.10 vs. 82.12 years, P<0.001), lower BNP levels (625.13±823.71 vs. 929.31±873.38 pg/mL, P<0.0001), and longer period of hospitalization (24.38 vs. 15.65 days, P<0.01). However, there was no significant difference between the geriatric department readmissions and readmissions to other departments in terms of the atrial fibrillation percentage (19% vs. 21.4%, P=0.356), heart rate (70.56±15.23 vs. 72.23±14.67 beats per minute, P=0.194), nor total costs ($4,483 vs. $4,415, P=0.129). The characteristics of the patients are presented in Table 1.
Table 1
| Characteristics | Geriatric department (n=858) | Other departments (n=458) | P value |
|---|---|---|---|
| Age in years, mean ± SD | 89.10±4.582 | 82.12±8.096 | <0.001 |
| Male, n (%) | 626 (72.96) | 267 (58.29) | <0.0001 |
| Female, n (%) | 232 (27.04) | 191 (41.74) | – |
| BNP (pg/mL), mean ± SD | 625.13±823.71 | 929.31±873.38 | <0.0001 |
| EF (%), mean ± SD | 56.3±23.7 | 53.8±18.9 | 0.231 |
| Heart rate (bpm), mean ± SD | 70.56±15.23 | 72.23±14.67 | 0.194 |
| Atrial fibrillation, n (%) | 163 (19.00) | 98 (21.40) | 0.356 |
| LOS in days, mean ± SD | 24.38±5.228 | 15.65±5.907 | <0.01 |
| Discharge disposition, n (%) | |||
| Routine | 849 (98.95) | 397 (13.32) | 0.016 |
| Other institution | 9 (1.05) | 61 (86.68) | – |
| Cost of hospitalization ($), mean ± SD | 4,483±192 | 4,415±320 | 0.129 |
SD, standard deviation; BNP, brain natriuretic peptide; EF, ejection fraction; LOS, length of stay.
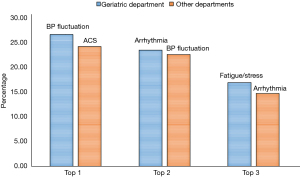
The top 3 diagnosis for rehospitalizations lasting 7 days or less in the geriatric department were blood pressure fluctuations (26.5%), arrhythmia (23.4%), and fatigue or stress (16.9%). The top 3 diagnosis for rehospitalizations lasting 7 days or less in other departments were acute coronary syndrome (ACS) (24.1%), blood pressure fluctuations (22.5%), and arrhythmia (14.7%) (Figure 1).
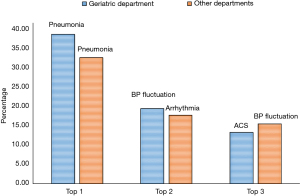
The top 3 diagnosis for rehospitalizations that lasted more than 7 days in the geriatric department were pneumonia (38.5%), blood pressure fluctuations (19.4%), and ACS (13.3%); while for readmission to the other departments, the top 3 diagnosis were pneumonia (32.5%), arrhythmia (17.7%), and blood pressure fluctuations (15.5%) (Figure 2).
There was no statistical difference in the costs associated with pneumonia readmissions to the geriatric department compared to other departments ($5,159±351 vs. $5,435±489, P=0.12). However, in patients readmitted without pneumonia, the cost was significantly different between departments ($2,575±453 in the geriatric department vs. $3,433±504 in other departments, P<0.0001) (Table 2).
Table 2
| Cost ($) | Geriatric department (n=858) | Other departments (n=458) | P value |
|---|---|---|---|
| With pneumonia, mean ± SD | 5,159±351 | 5,435±489 | 0.12 |
| Without pneumonia, mean ± SD | 2,575±453 | 3,433±504 | <0.0001 |
SD, standard deviation.
Discussion
In this present study, the readmission rate for Chinese senile patients with acute decompensated heart failure was 33.55%, which was much higher than the 16.8–32.6% reported by other researchers (14-16). There is a high prevalence of heart failure in the senile population and old age is a risk factor for readmission. Furthermore, older patients have higher incidence of geriatric syndromes which are also associated with early readmission. These factors may contribute to the higher readmission rates observed in this study.
The mean length of stay (LOS) in the geriatric department and other departments was 24.38 and 15.65 days, respectively. Both were much longer than the target “9 days” which is the average LOS in our hospital. The duration of hospitalization has prognostic implications, and 7 days is used as the cut-off to define prolonged hospital stay. However, the appropriate hospital stay length should be adjusted due to great variability between countries (17). The REDUCE-AHF study showed that Spanish heart failure patients have an average 9-day LOS (18), while in-hospital mortality has been reported to range from 2.7–2.9% in different countries (19,20). Significant efforts must be made to reduce the LOS. In-hospital mortality information was not available in the present study since those who died within 30 days after discharge or in-hospital were excluded.
The LOS has been adopted to identify the severity of illnesses and healthcare resource utilization (21), and can be influenced by numerous factors (22). It is not easy to specify the underlying diagnosis for the prolonged LOS in our study. However, various factors may contribute to the postponed time to discharge, such as multiple chronic conditions, polypharmacy, frailty and geriatric syndromes, and delayed discharge. The latter has been mentioned by Europe practitioners and much effort has been made to develop approaches that focus on arranging swift and effective discharge from acute settings, thereby reducing cases of delayed discharge (23-25).
With the increase in the aging population, many hospitals in China have already established a geriatric department. However, long-term care, short-term care, and home care remain inadequate, while specialized care cannot be extensively provided for elderly patients (26). Therefore, these patients and their relatives may be concerned about discharge from the hospital to return home directly. Staying at the hospital may appear to be a safer solution. However, this unnecessary hospital stay may be costly and harmful to the elderly patient, and wasteful to the public health system. Therefore, there is an urgency to establish and improve the level of geriatric care in the country.
Surprisingly, the present findings revealed that there was no statistical difference in the total cost between different wards, even if patients in the geriatric department had longer LOSs. This may be attributed to less drug use, fewer operations, and more palliative skills provided by the geriatricians. However, further research with more extensive and intensive data is needed for justification.
The most common factors for readmission and hospital stays longer than 7 days were identified as pneumonia in both the geriatric department and other departments. Ogbemudia et al. also reported the same results (27). Patients with acute decompensated heart failure are vulnerable to chest infections because of pulmonary edema, duripulmonary edema promotes the multiplications of pathogens in the airways. Recurrent aspiration or dysphagia may increase the infectious risk for the senile patients (28). Interestingly, the costs associated with patients with pneumonia were comparable in the geriatric department and other departments.
For those who stayed in hospital less than 7 days, the most common factors in the geriatric department and other departments was blood pressure fluctuations and ACS, respectively. This is in contrast to the findings reported by Kapoor et al., that pneumonia and arrhythmias as the two most common precipitants of heart failure (29).
There were some limitations in this study. First, as a retrospective study, the classification of diagnoses was conducted using diagnosis codes, and therefore some admissions may have been misclassified. Second, the data of patients who died at home within 30 days of discharge were not available in the hospital database or medical records, and this may reduce the effect of variables reflecting higher illness severity. Furthermore, survey logistic regression was used to assess the relationship between potential predictors for readmissions, but no positive results were found.
In conclusion, this study identified a high readmission rate in senile patients hospitalized with acute decompensated heart failure. The top 3 factors for readmissions were identified. For patients who stayed longer than 7 days in hospital, pneumonia, blood pressure fluctuations, and ACS were the top 3 factors in both the geriatric department and other departments. Furthermore, the total cost incurred by stays in the geriatric department was comparable to stays in other departments, despite the overall length of hospital stay being longer in the geriatric department than in other departments. Further studies to determine the diagnosis underlying delayed discharge is urgently needed, and improvements in the long-term care for elderly patients are warranted. Future investigations should assess the efficacy of such interventions.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-433/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-433/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-433/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics Committee of The People’s Hospital of Sichuan Province (No. 2019034). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Heidenreich PA, Albert NM, Allen LA, et al. Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 2013;6:606-19. [Crossref] [PubMed]
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation 2015;131:e29-322. Erratum in: Circulation 2015;131:e535 Erratum in: Circulation 2016;133:e417. [Crossref] [PubMed]
- Madanat L, Saleh M, Maraskine M, et al. Congestive Heart Failure 30-Day Readmission: Descriptive Study of Demographics, Co-morbidities, Heart Failure Knowledge, and Self-Care. Cureus 2021;13:e18661. [Crossref] [PubMed]
- Wang H, Chai K, Du M, et al. Prevalence and Incidence of Heart Failure Among Urban Patients in China: A National Population-Based Analysis. Circ Heart Fail 2021;14:e008406. [Crossref] [PubMed]
- Shakib S, Clark RA. Heart Failure Pharmacotherapy and Supports in the Elderly - A Short Review. Curr Cardiol Rev 2016;12:180-5. [Crossref] [PubMed]
- Kimmoun A, Takagi K, Gall E, et al. Temporal trends in mortality and readmission after acute heart failure: a systematic review and meta-regression in the past four decades. Eur J Heart Fail 2021;23:420-31. [Crossref] [PubMed]
- Greene SJ, Fonarow GC, Vaduganathan M, et al. The vulnerable phase after hospitalization for heart failure. Nat Rev Cardiol 2015;12:220-9. [Crossref] [PubMed]
- Schmidt S, Hendricks V, Griebenow R, et al. Demographic change and its impact on the health-care budget for heart failure inpatients in Germany during 1995-2025. Herz 2013;38:862-7. [Crossref] [PubMed]
- Viganego F, Um EK, Ruffin J, et al. Impact of Global Budget Payments on Cardiovascular Care in Maryland: An Interrupted Time Series Analysis. Circ Cardiovasc Qual Outcomes 2021;14:e007110. [Crossref] [PubMed]
- Voors AA, Ouwerkerk W, Zannad F, et al. Development and validation of multivariable models to predict mortality and hospitalization in patients with heart failure. Eur J Heart Fail 2017;19:627-34. [Crossref] [PubMed]
- Ahmed A, Aronow WS, Fleg JL. Higher New York Heart Association classes and increased mortality and hospitalization in patients with heart failure and preserved left ventricular function. Am Heart J 2006;151:444-50. [Crossref] [PubMed]
- Choi ES, Wiseman T, Betihavas V. Biomedical, Socioeconomic and Demographic Predictors of Heart Failure Readmissions: A Systematic Review. Heart Lung Circ 2021;30:817-36. [Crossref] [PubMed]
- Lan T, Liao YH, Zhang J, et al. Mortality and Readmission Rates After Heart Failure: A Systematic Review and Meta-Analysis. Ther Clin Risk Manag 2021;17:1307-20. [Crossref] [PubMed]
- Ayatollahi Y, Liu X, Namazi A, et al. Early Readmission Risk Identification for Hospitalized Older Adults With Decompensated Heart Failure. Res Gerontol Nurs 2018;11:190-7. [Crossref] [PubMed]
- Drozda JP Jr, Smith DA, Freiman PC, et al. Heart Failure Readmission Reduction. Am J Med Qual 2017;32:134-40. [Crossref] [PubMed]
- Matsukawa R, Masuda S, Matsuura H, et al. Early follow-up at outpatient care after discharge improves long-term heart failure readmission rate and prognosis. ESC Heart Fail 2021;8:3002-13. [Crossref] [PubMed]
- López-Vilella R, Marqués-Sulé E, Sánchez-Lázaro I, et al. Creatinine and NT-ProBNP levels could predict the length of hospital stay of patients with decompensated heart failure. Acta Cardiol 2021;76:1100-7. [Crossref] [PubMed]
- Miró Ò, Carbajosa V, Peacock WF, et al. The effect of a short-stay unit on hospital admission and length of stay in acute heart failure: REDUCE-AHF study. Eur J Intern Med 2017;40:30-6. [Crossref] [PubMed]
- Martín-Sánchez FJ, Carbajosa V, Llorens P, et al. Prolonged hospitalization in patients admitted for acute heart failure in the short stay unit (EPICA-UCE study): study of associated factors. Med Clin (Barc) 2014;143:245-51. [PubMed]
- Akintoye E, Briasoulis A, Egbe A, et al. National Trends in Admission and In-Hospital Mortality of Patients With Heart Failure in the United States (2001-2014). J Am Heart Assoc 2017;6:006955. [Crossref] [PubMed]
- Awad A, Bader-El-Den M, McNicholas J. Patient length of stay and mortality prediction: A survey. Health Serv Manage Res 2017;30:105-20. [Crossref] [PubMed]
- Lei P, Feng Z, Wu Z. The availability and affordability of long-term care for disabled older people in China: The issues related to inequalities in social security benefits. Arch Gerontol Geriatr 2016;67:21-7. [Crossref] [PubMed]
- Butt M, Jabri A, Messeh H, et al. The Effect of Early Aggressive Diuresis on Hospital Length of Stay in Acute Congestive Heart Failure. Heart Views 2021;22:108-14. [PubMed]
- Tal S. Length of hospital stay among oldest-old patients in acute geriatric ward. Arch Gerontol Geriatr 2021;94:104352. [Crossref] [PubMed]
- Al-Tamimi MA, Gillani SW, Abd Alhakam ME, et al. Factors Associated With Hospital Readmission of Heart Failure Patients. Front Pharmacol 2021;12:732760. [Crossref] [PubMed]
- Lu B, Liu X, Yang M. A Budget Proposal for China's Public Long-Term Care Policy. J Aging Soc Policy 2017;29:84-103. [Crossref] [PubMed]
- Ogbemudia EJ, Obasohan AO. Association between Common Etiologies and Precipitants of Acute Decompensated Heart Failure. Niger Med J 2019;60:113-6. [Crossref] [PubMed]
- Omori M, Chojin Y, Hashiki S, et al. A Simple Assessment of the Eating and Swallowing Functions in Elderly Patients with Pneumonia. J UOEH 2019;41:283-94. [Crossref] [PubMed]
- Kapoor JR, Kapoor R, Ju C, et al. Precipitating Clinical Factors, Heart Failure Characterization, and Outcomes in Patients Hospitalized With Heart Failure With Reduced, Borderline, and Preserved Ejection Fraction. JACC Heart Fail 2016;4:464-72. [Crossref] [PubMed]
(English Language Editor: J. Teoh)


