
Study on the predictive ability of emergency CHADS2 score and CHA2DS2-VASc score for coronary artery disease and prognosis in patients with acute ST-segment elevation myocardial infarction
Introduction
Acute ST-segment elevation myocardial infarction (STEMI) occurs with significantly higher than normal levels of serum myocardial injury markers in patients with ischemic chest pain, and most of these patients have a poor prognosis (1). Acute STEMI mostly manifests as myocardial ischemic necrosis, associated with coronary atherosclerotic plaque rupture leading to angiogenesis and coronary occlusion; a study (2) has found that the morbidity and mortality of acute STEMI are high, and most patients have a poor prognosis, which seriously affects the life safety of these patients. Acute STEMI has now become one of the most important causes of death worldwide, so it is particularly important to perform an assessment of emergency coronary lesion extent and prognosis prediction after admission to reduce clinical mortality in patients with acute STEMI. The congestive heart failure, hypertension, age, diabetes, previous stroke/transient ischemic attack (TIA) (2 points)(CHADS2) score (3) and CHADS2 score with 2 points assigned for age >75 years-vascular disease (CHA2DS2-VASc) score (4) are risk stratification management scores that are widely used in non-valvular atrial fibrillation stroke, and with the continuous application of the above scoring systems in clinical practice, have been found to be of high value in predicting patient prognosis in cardiovascular disease. Most of the components of the CHADS2 and CHA2DS2-VASc scores are also risk factors for coronary atherosclerosis and can therefore be used to predict the severity of CAD. There are many methods to predict the severity of CAD and the prognosis of STEMI, such as monitoring by ECG, monitoring by laboratory tests, angiographic intervention, etc. However, these methods are time-consuming, lagging, and complicated to perform. CHADS2 and CHA2DS2-VASc scores are simple to administer and provide a basic understanding of the patient’s condition in a short period of time. However, by searching the relevant literature, we were unable to locate any study that used both scoring systems to predict coronary lesions and prognosis in patients with acute STEMI. Therefore, we hypothesized that both scores could predict the severity of coronary lesions and prognosis in patients, and to verify this hypothesis, this study was designed and is reported below. We present the following article in accordance with the STARD reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-763/rc).
Methods
Objective
A total of 524 consecutive acute STEMI patients admitted to the Emergency Department of the Chinese PLA General Hospital from May 2018 to October 2021 were enrolled in the present retrospective, cohort study. All patients had undergone emergency CHADS2 and CHA2DS2-VASc scoring. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Chinese PLA General Hospital (No. 20220079). Individual consent for this retrospective analysis was waived.
Inclusion and exclusion criteria
In line with the clinical diagnosis of the disease, all cases had manifestations of chest pain in the precordial region, duration of chest pain ≥0.5 hours, ST-segment elevation in electrocardiogram (ECG) leads, and markedly elevated markers of myocardial injury such as troponin and creatine kinase isoenzymes.
The exclusion criteria were as follows: previous history of coronary artery bypass grafting or percutaneous coronary intervention; congenital heart disease; combined pulmonary and urinary tract infection; combined lung and liver cancer; organ insufficiency; incomplete clinical data; and communication and mental abnormalities.
Research methods
Clinical data collection
Clinical data were collected from all patients, including gender, age, body mass index (BMI), comorbidities (hypertension, diabetes, stroke, TIA, congestive heart failure, hyperlipidemia), family history of myocardial infarction, history of smoking, history of alcohol consumption, Killip class ≥2, and laboratory indices [triglycerides (TG), total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), creatinine (Crea), cystatin C (CysC), hemoglobin (Hb), white blood cell count (WBC), and left ventricular ejection fraction (LVEF)].
Evaluation of the degree of coronary artery lesion
After hospital admission, cases underwent coronary angiography [a common and effective method for diagnosing coronary artery disease (CAD) which is a safe and reliable invasive diagnostic technique that is now widely used in clinical practice and is considered the “gold standard” for the diagnosis of CAD] using the standard Jundkin’s technique (5). The SYNTAX score (https://syntaxscore.org/) calculation was performed by two experienced physicians without knowledge of the baseline clinical features and clinical findings. The degree of coronary artery lesions was evaluated according to the SYNTAX score, with higher scores indicating more severe coronary artery lesions in patients with severe lesions, as follows: ≥33 points, moderate lesions: 23–32 points, and mild lesions: ≤22 points. Cases were divided into mild to moderate and severe groups according to their SYNTAX score.
Prognostic evaluation
Whether major adverse cardiovascular events (MACE) occurred during hospitalization was used as the endpoint event, and MACE events mainly included all-cause death of disease and recurrent myocardial infarction, which were divided into good and poor groups according to whether MACEs had occurred.
Scoring method
(I) The CHADS2 score scoring method is as follows: 1 point for congestive heart failure, hypertension, age ≥75 years, and diabetes mellitus, and 2 points for stroke or TIA, respectively. (II) The CHA2DS2-VASc score scoring method is as follows: 1 point for congestive heart failure, hypertension, diabetes mellitus, vascular disease, age 65–75 years, and gender (female), and 2 for stroke or TIA, and age ≥75 years, respectively. The scorers were blinded to the baseline clinical characteristics and clinical outcomes of cases in each group.
Indicator observation
(I) To count the general data of patients in different coronary lesion subgroups and different prognosis subgroups, and to compare the CHADS2 score and CHA2DS2-VASc score between different subgroups. (II) To analyze the factors affecting the coronary artery lesions and prognosis of acute STEMI patients. (III) To analyze the predictive value of the two scores on the coronary artery lesions and prognosis of acute STEMI patients.
Statistical analysis
The measures were first analyzed using the Kolmogorov-Smirnov test, and if the results showed conformity to a normal distribution, they were described using (), and independent samples t-test was used for comparison between groups. If they did not conform to a normal distribution, they were described using the median and quartiles [M(P25, P75)], and the Mann-Whitney test was used for comparisons between groups. The statistical data were expressed as ratios, and the chi-square test was used for comparison. Logistic regression analysis was applied to the risk factors affecting coronary artery lesions, prognosis in patients with acute STEMI. The receiver operating characteristic (ROC) curve was applied to analyze the predictive value of CHADS2 score and CHA2DS2-VASc score on coronary artery lesions and the prognosis of patients. All statistics were tested using a two-sided test at α=0.05. A statistically significant difference was indicated when P<0.05, with a 95% confidence interval (CI). All data were analyzed using the software SPSS 22.0 (IBM Corp., Armonk, NY, USA).
Results
Comparison of various indexes in different coronary lesion subgroups
A total of 524 patients with acute STEMI, 238 men and 286 women, aged 48–80 years, were included in the study. The patients were grouped according to the degree of coronary artery lesions, including 385 cases in the mild to moderate group and 139 cases in the severe group. As shown in Table 1, the differences between the two groups were statistically significant when comparing diabetes mellitus, stroke or TIA, congestive heart failure, smoking history, percentage of Killip class ≥2, CysC, LVEF, CHADS2 score, and CHA2DS2-VASc score. The percentage of diabetes mellitus, stroke or TIA, congestive heart failure, smoking history, and Killip class ≥2 was higher in the severe group than in the mild to moderate group, and the CysC, CHADS2 score, and CHA2DS2-VASc score were higher than in the mild to moderate group, and LVEF was lower than in the mild to moderate group (P<0.05).
Table 1
| Clinical indicators | Mild to moderate group (n=385) | Severe group (n=139) | χ2/t | P value |
|---|---|---|---|---|
| Gender (male/female) | 173/212 | 65/74 | 0.138 | 0.711 |
| Average age (years) | 62.43±5.43 | 62.87±5.13 | 0.831 | 0.406 |
| Average BMI (kg/m2) | 23.45±2.93 | 23.76±3.00 | 1.041 | 0.289 |
| Hypertension | 102 (26.49) | 34 (24.46) | 0.261 | 0.610 |
| Diabetes mellitus | 54 (14.03) | 65 (46.76) | 62.355 | <0.001 |
| Stroke or TIA | 62 (16.10) | 53 (38.13) | 28.923 | <0.001 |
| Congestive heart failure | 71 (18.44) | 56 (40.29) | 26.544 | <0.001 |
| Hyperlipidemia | 67 (17.40) | 23 (16.55) | 0.053 | 0.819 |
| Family history of heart attack | 85 (22.08) | 24 (17.27) | 1.435 | 0.231 |
| Smoking history | 71 (18.44) | 48 (34.53) | 26.209 | <0.001 |
| Drinking history | 87 (22.60) | 39 (28.06) | 1.667 | 0.197 |
| Killip class ≥2 | 89 (23.12) | 51 (36.69) | 9.611 | 0.002 |
| TG (mmol/L) | 1.50±0.28 | 1.53±0.32 | 1.041 | 0.298 |
| TC (mmol/L) | 4.27±0.65 | 4.32±0.76 | 0.742 | 0.458 |
| HDL-C (mmol/L) | 1.13±0.17 | 1.15±0.19 | 1.152 | 0.250 |
| LDL-C (mmol/L) | 2.93±0.43 | 2.98±0.32 | 1.251 | 0.211 |
| Crea (μmol/L) | 70.98±5.17 | 71.23±5.10 | 0.490 | 0.624 |
| CysC (μmol/L) | 1.00±0.11 | 1.29±0.17 | 22.790 | <0.001 |
| Hb (g/L) | 138.11±14.62 | 137.96±14.54 | 0.104 | 0.917 |
| WBC (×109/L) | 7.23±0.84 | 7.17±0.82 | 0.726 | 0.468 |
| LVEF (%) | 60.98±7.65 | 52.18±5.13 | 12.580 | <0.001 |
| CHADS2 score (points) | 1.10±0.21 | 2.34±0.56 | 39.570 | <0.001 |
| CHA2DS2-VASc score (points) | 2.17±0.34 | 5.62±0.87 | 65.290 | <0.001 |
BMI, body mass index; TIA, transient ischemic attack; TG, triglycerides; TC, total cholesterol; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; Crea, creatinine; CysC, cystatin C; Hb, hemoglobin; WBC, white blood cells; LVEF, left ventricular ejection fraction; CHADS2, congestive heart failure, hypertension, age, diabetes, previous stroke/transient ischemic attack (2 points); CHA2DS2-VASc, CHADS2 score with 2 points assigned for age >75 years-vascular disease.
Analysis of factors affecting coronary artery lesions in patients with acute STEMI
As shown in Table 2, the severity of coronary artery lesions in patients with acute STEMI was used as the dependent variable (mild to moderate =0, severe =1), and the indicators with differences in the above table were used as independent variables to establish a logistic regression model, and the results showed that diabetes, CHADS2 score, and CHA2DS2-VASc score were independent risk factors (P<0.05).
Table 2
| Clinical indicators | β | SE | Wald χ2 | OR | 95% CI | P value |
|---|---|---|---|---|---|---|
| Diabetes mellitus | 0.765 | 0.238 | 10.922 | 3.678 | 2.876–5.872 | 0.008 |
| Stroke or TIA | 0.778 | 0.226 | 1.112 | 1.029 | 0.754–2.387 | 0.339 |
| Congestive heart failure | 0.654 | 0.279 | 1.087 | 1.276 | 0.812–2.549 | 0.487 |
| Smoking history | 0.526 | 0.228 | 1.022 | 1.236 | 0.765–2.834 | 0.256 |
| Killip ≥ grade 2 | 0.487 | 0.217 | 1.991 | 1.037 | 0.827–2.765 | 0.098 |
| CysC | 0.678 | 0.321 | 1.768 | 1.002 | 0.910–2.338 | 0.273 |
| LVEF | 0.662 | 0.227 | 1.636 | 1.132 | 0.876–2.239 | 0.128 |
| CHADS2 score | 0.519 | 0.256 | 15.223 | 3.829 | 2.310–5.832 | 0.003 |
| CHA2DS2-VASc score | 0.556 | 0.231 | 16.198 | 4.671 | 3.125–6.187 | 0.000 |
STEMI, ST-segment elevation myocardial infarction; SE, standard error; OR, odds ratio; CI, confidence interval; TIA, transient ischemic attack; CysC, cystatin C; LVEF, left ventricular ejection fraction; CHADS2, congestive heart failure, hypertension, age, diabetes, previous stroke/transient ischemic attack (2 points); CHA2DS2-VASc, CHADS2 score with 2 points assigned for age >75 years-vascular disease.
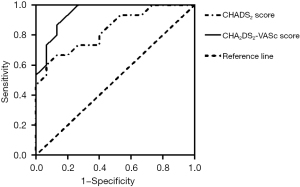
Analysis of the predictive value of CHADS2 score and CHA2DS2-VASc score on the severity of coronary artery lesions in patients with acute STEMI
As shown in Table 3 and Figure 1, AUC value of CHA2DS2-VASc score in evaluating the severity of coronary artery lesions was 0.947, significantly higher than that of CHADS2 (0.836) (Z=3.424, P<0.05), suggesting that CHA2DS2-VASc score was more suitable for predicting the severity of coronary artery lesions in patients with acute STEMI than the CHADS2 score.
Table 3
| Clinical indicators | Area under curve | 95% CI | Cut off value | Sensitivity | Specificity | P value |
|---|---|---|---|---|---|---|
| CHADS2 score | 0.836 | 0.693–0.978 | 2.00 | 85.14% | 77.86% | 0.002 |
| CHA2DS2-VASc score | 0.947 | 0.873–1.000 | 4.50 | 89.90% | 75.17% | <0.001 |
CHADS2, congestive heart failure, hypertension, age, diabetes, previous stroke/transient ischemic attack (2 points); CHA2DS2-VASc, CHADS2 score with 2 points assigned for age >75 years-vascular disease; STEMI, ST-segment elevation myocardial infarction; CI, confidence interval.
Comparison of various indicators in different prognostic subgroups
As shown in Table 4, the differences between the two groups were statistically significant in hypertension, diabetes, stroke or TIA, congestive heart failure, smoking history, Killip class ≥2, Crea, CysC, Hb, LVEF, CHADS2 score, and CHA2DS2-VASc score. The percentage of hypertension, diabetes mellitus, stroke or TIA, congestive heart failure, smoking history, and Killip class ≥2 was higher in the poor prognosis group than in the good prognosis group; Crea, CysC, Hb, CHADS2 score, and CHA2DS2-VASc score were higher than in the good prognosis group; and LVEF was lower than in the good prognosis group (P<0.05).
Table 4
| Clinical indicators | Good group (n=368) | Poor group (n=156) | χ2/t | P value |
|---|---|---|---|---|
| Gender (male/female) | 157/211 | 81/75 | 3.790 | 0.052 |
| Average age (years) | 62.86±5.33 | 63.02±5.28 | 0.295 | 0.768 |
| Average BMI (kg/m2) | 23.76±3.24 | 23.88±3.12 | 0.392 | 0.695 |
| Hypertension | 79 (21.47) | 57 (36.54) | 7.074 | 0.008 |
| Diabetes mellitus | 65 (17.66) | 54 (34.62) | 17.937 | <0.001 |
| Stroke or TIA | 69 (18.75) | 46 (29.49) | 7.373 | 0.007 |
| Congestive heart failure | 64 (17.39) | 63 (40.38) | 41.544 | <0.001 |
| Hyperlipidemia | 66 (17.93) | 24 (15.38) | 0.501 | 0.479 |
| Family history of heart attack | 54 (14.67) | 25 (16.03) | 0.156 | 0.693 |
| Smoking history | 68 (18.48) | 51 (32.69) | 12.611 | <0.001 |
| Drinking History | 79 (21.47) | 27 (17.31) | 1.175 | 0.278 |
| Killip class ≥2 | 85 (23.10) | 55 (35.26) | 8.272 | 0.004 |
| TG (mmol/L) | 1.52±0.41 | 1.56±0.35 | 1.065 | 0.287 |
| TC (mmol/L) | 4.18±0.33 | 4.25±0.46 | 1.962 | 0.052 |
| HDL-C (mmol/L) | 1.11±0.23 | 1.08±0.32 | 1.208 | 0.228 |
| LDL-C (mmol/L) | 2.79±0.37 | 2.87±0.54 | 1.958 | 0.051 |
| Crea (μmol/L) | 76.81±6.12 | 88.65±10.33 | 16.270 | <0.001 |
| CysC (μmol/L) | 1.00±0.14 | 1.34±0.21 | 21.710 | <0.001 |
| Hb (g/L) | 130.23±13.65 | 139.98±12.34 | 7.688 | <0.001 |
| WBC (×109/L) | 7.18±0.25 | 7.22±0.31 | 1.555 | 0.121 |
| LVEF (%) | 61.29±7.85 | 50.53±4.87 | 15.870 | <0.001 |
| CHADS2 score (points) | 1.04±0.12 | 3.27±0.43 | 91.530 | <0.001 |
| CHA2DS2-VASc score (points) | 2.45±0.55 | 5.12±0.86 | 42.510 | <0.001 |
BMI, body mass index; TIA, transient ischemic attack; TG, triglycerides; TC, total cholesterol; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; Crea, creatinine; CysC, cystatin C; Hb, hemoglobin; WBC, white blood cells; LVEF, left ventricular ejection fraction; CHADS2, congestive heart failure, hypertension, age, diabetes, previous stroke/transient ischemic attack (2 points); CHA2DS2-VASc, CHADS2 score with 2 points assigned for age >75 years-vascular disease.
Multivariate analysis of affecting the prognosis of patients with acute STEMI
As shown in Table 5, a logistic regression model was developed using the severity of coronary artery lesions in patients with acute STEMI as the dependent variable (good =0, poor =1) and the indicators that differed in the above table as independent variables, and the results showed that diabetes, Killip class ≥2, LVEF, CHADS2 score, and CHA2DS2-VASc score were all independent risk factors (P<0.05).
Table 5
| Clinical indicators | β | SE | Wald χ2 | OR | 95% CI | P value |
|---|---|---|---|---|---|---|
| Diabetes mellitus | 0.657 | 0.186 | 10.987 | 3.287 | 2.231–5.123 | 0.012 |
| Stroke or TIA | 0.764 | 0.241 | 1.078 | 1.182 | 0.542–1.578 | 0.346 |
| Congestive heart failure | 0.662 | 0.189 | 1.004 | 1.876 | 0.675–1.965 | 0.417 |
| Smoking history | 0.546 | 0.228 | 1.289 | 1.227 | 0.778–1.398 | 0.552 |
| Killip ≥ grade 2 | 0.625 | 0.254 | 5.224 | 2.212 | 1.023–2.987 | 0.045 |
| CysC | 0.629 | 0.286 | 1.072 | 1.231 | 0.765–1.876 | 0.281 |
| LVEF | 0.576 | 0.267 | 7.054 | 3.110 | 2.124–5.031 | 0.023 |
| CHADS2 score | 0.633 | 0.334 | 15.387 | 3.228 | 2.133–5.886 | 0.005 |
| CHA2DS2-VASc score | 0.572 | 0.231 | 18.970 | 3.988 | 2.987–5.873 | 0.001 |
STEMI, ST-segment elevation myocardial infarction; SE, standard error; OR, odds ratio; CI, confidence interval; TIA, transient ischemic attack; CysC, cystatin C; LVEF, left ventricular ejection fraction; CHADS2, congestive heart failure, hypertension, age, diabetes, previous stroke/transient ischemic attack (2 points); CHA2DS2-VASc, CHADS2 score with 2 points assigned for age >75 years-vascular disease.
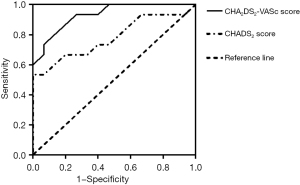
Analysis of the predictive value of CHADS2 score and CHA2DS2-VASc score on the prognosis of patients with acute STEMI
As shown in Table 6 and Figure 2, AUC value of CHA2DS2-VASc score in evaluating the prognosis of patients with acute STEMI was 0.931, significantly higher than that of CHADS2 (0.812) (Z=3.633, P<0.05), suggesting that the CHA2DS2-VASc score was more suitable for predicting the prognosis of patients with acute STEMI than the CHADS2 score.
Table 6
| Clinical indicators | Area under curve | 95% CI | Cut off value | Sensitivity | Specificity | P value |
|---|---|---|---|---|---|---|
| CHADS2 score | 0.812 | 0.608–0.952 | 2.19 | 82.14% | 77.98% | 0.009 |
| CHA2DS2-VASc score | 0.931 | 0.846–1.016 | 4.80 | 87.98% | 75.34% | <0.001 |
CHADS2, congestive heart failure, hypertension, age, diabetes, previous stroke/transient ischemic attack (2 points); CHA2DS2-VASc, CHADS2 score with 2 points assigned for age >75 years-vascular disease; STEMI, ST-segment elevation myocardial infarction; CI, confidence interval.
Discussion
The application of quantitative assessment systems of multiple risk factors is important for the identification and prognosis of patients with high-risk cardiovascular disease. Among them, the CHADS2 and CHA2DS2-VASc scoring systems are two of the more widely used scoring systems, and both were first used clinically in patients with atrial fibrillation (6,7). In recent years, the relationship between these two scoring systems and cardiovascular disease has become a hot topic of research, and Zorlu et al. (8) and Kilic et al. (9) both concluded in their studies that the two systems could predict the absence of reflow phenomenon and reperfusion failure after thrombolytic therapy in patients with acute STEMI, respectively. A study by Chen et al. (10) showed that both scores predicted prognostic death in patients with heart failure with or without an atrial fibrillation phase. This suggests that both may have the ability to predict the degree of CAD and prognosis in patients with acute STEMI and may play an important role in the assessment of the degree of CAD and prognosis.
The results of this paper showed that the CHADS2 score and CHA2DS2-VASc score were higher in patients with more severe coronary artery lesions and poorer prognosis. Further multifactorial analysis was used to determine whether they were risk factors affecting coronary artery lesions and prognosis in patients with acute STEMI, and the results showed that both were independent risk factors, which suggests that the two scoring systems may have the potential to predict patients’ coronary artery lesions and prognosis. In addition, although this paper concluded that both CHADS2 score and CHA2DS2-VASc score are related to the degree and prognosis of coronary artery lesions in patients with acute STEMI, it did not analyze their specific pathophysiological mechanisms in depth and concluded that their correlation may be related to the following points: (I) both the CHADS2 score and CHA2DS2-VASc scoring systems contain STEMI occurrence risk factors, such as hypertension, diabetes mellitus, stroke or TIA, and age ≥75 years, and both scoring systems are a combination of these factors (11-13). (II) Local inflammation in the body can mediate the development of STEMI, and a study has found that the two-scoring system is immune-related (14).
Several clinical studies have now found (15-17) that diabetes mellitus, hypertension, age, heart failure, and stroke are all risk factors that influence the development and prognosis of acute STEMI disease. Among them, stroke and peripheral vascular disease are not only manifested as peripheral and cerebral circulatory ischemia, but also associated with atherosclerosis including coronary artery-related atherosclerosis, and therefore stroke is considered an independent risk factor for CAD and prognosis in STEMI patients (18,19). The effect of gender on the development of acute STEMI disease and prognosis is still somewhat controversial, but studies have shown (20,21) that the risk of MACE is significantly higher in female than in male patients. Based on the above evidence, the ability of the two scores to predict CAD and prognosis in patients with acute STEMI is associated with a combination of the above factors. The content of the CHADS2 score includes only the above-mentioned factors, yet the CHA2DS2-VASc score has three new factors added on this basis, namely gender, vascular disease, and age 65–75 years, which may have a better predictive value for disease than the CHADS2 score (22-24). In this paper, we further analyzed the value of the two scoring systems in predicting coronary artery lesions and prognosis in patients with acute STEMI, and the results showed that the area under the curve (AUC) of CHADS2 score in predicting coronary artery lesions and prognosis in patients with acute STEMI was 0.836 and 0.812, respectively, and the AUC of CHA2DS2-VASc score in predicting coronary artery lesions and prognosis in patients with acute STEMI was 0.947 and 0.931, respectively. This indicates that the AUC of both was >0.7, suggesting that both can be predicted, but the CHA2DS2-VASc has a higher predictive value compared with that of the CHADS2; a better predictive value can be chosen in clinical practice to assess the coronary artery lesions of patients to the maximum extent, select the appropriate medication regimen, and improve the prognosis.
This paper is innovative in that it used SYNTAX, which is widely used in clinical practice, to evaluate the degree of coronary artery lesions in patients, and this scoring system can more accurately reflect the degree of coronary artery lesions in patients. In addition, the CHA2DS2-VASc score is more suitable for evaluating the degree of coronary artery lesions and prognosis of patients than CHADS2 score, which has certain guiding significance for the study of acute STEMI.
The sample size included in this study was small, and the analysis of patient prognosis was limited to the prognosis during hospitalization. Changes in patients’ in-hospital medication regimens also affect prognosis and may influence the results, and the specific mechanisms were not analyzed in depth, so the results of this paper need to be verified through a large scale study with long-term follow-up.
Conclusions
In conclusion, the coronary artery lesions and prognosis of patients with acute STEMI are influenced by a combination of factors, including diabetes, Killip class ≥2, LVEF, CHADS2 score, and CHA2DS2-VASc score. The CHA2DS2-VASc score is more valuable than CHADS2 score in evaluating patients’ coronary artery lesions and prognosis, and has a better clinical application prospect.
Acknowledgments
Funding: This study was funded by a grant from the Military Medical Science and Technology Youth Cultivation Program (No. 20QNPY134) and the Military Health Care Project (No. 19BJZ27).
Footnote
Reporting Checklist: The authors have completed the STARD reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-763/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-763/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-763/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Chinese PLA General Hospital (No. 20220079). Individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Vogel B, Claessen BE, Arnold SV, et al. ST-segment elevation myocardial infarction. Nat Rev Dis Primers 2019;5:39. [Crossref] [PubMed]
- Armstrong R, De Maria GL, Scarsini R, et al. Assessing and managing coronary microcirculation dysfunction in acute ST-segment elevation myocardial infarction. Expert Rev Cardiovasc Ther 2019;17:111-26. [Crossref] [PubMed]
- Ma X, Shao Q, Dong L, et al. Prognostic value of CHADS2 and CHA2DS2-VASc scores for post-discharge outcomes in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Medicine (Baltimore) 2020;99:e21321. [Crossref] [PubMed]
- Sulzgruber P, Wassmann S, Semb AG, et al. Oral anticoagulation in patients with non-valvular atrial fibrillation and a CHA2DS2-VASc score of 1: a current opinion of the European Society of Cardiology Working Group on Cardiovascular Pharmacotherapy and European Society of Cardiology Council on Stroke. Eur Heart J Cardiovasc Pharmacother 2019;5:171-80. [Crossref] [PubMed]
- Page HL Jr. The Judkin's technique. Cathet Cardiovasc Diagn. 1979;5:187-9. [Crossref] [PubMed]
- Asher E, Abu-Much A, Bragazzi NL, et al. CHADS2 and CHA2DS2-VASc scores as predictors of platelet reactivity in acute coronary syndrome. J Cardiol 2021;77:375-9. [Crossref] [PubMed]
- Degirmenci H, Bakirci EM. The CHA2DS2-VASc Score and Acute Stent Thrombosis After Primary Percutaneous Coronary Intervention. Angiology 2021;72:492. [Crossref] [PubMed]
- Zorlu Ç, Köseoğlu C. Comparison of RCHA2DS2-VASc score and CHA2DS2-VASc score prediction of no-reflow phenomenon in patients with ST-segment elevation myocardial infarction. Turk Kardiyol Dern Ars 2020;48:664-72. [PubMed]
- Kilic S, Kocabas U, Can LH, et al. Predictive value of CHA2DS2-VASc and CHA2DS2-VASc-HS scores for failed reperfusion after thrombolytic therapy in patients with ST-segment elevation myocardial infarction. Cardiol J 2019;26:169-75. [PubMed]
- Chen YL, Cheng CL, Huang JL, et al. Mortality prediction using CHADS2/CHA2DS2-VASc/R2CHADS2 scores in systolic heart failure patients with or without atrial fibrillation. Medicine (Baltimore) 2017;96:e8338. [Crossref] [PubMed]
- Ji C, Wu S, Shi J, et al. Baseline CHADS2 Score and Risk of Cardiovascular Events in the Population Without Atrial Fibrillation. Am J Cardiol 2020;129:30-5. [Crossref] [PubMed]
- Aksoy F, Baş HA, Bağcı A, et al. The CHA2DS2-VASc score for predicting atrial fibrillation in patients presenting with ST elevation myocardial infarction: prospective observational study. Sao Paulo Med J 2019;137:248-54. [Crossref] [PubMed]
- Li X, Zeng Z, Yang X, et al. Predictive value of CHADS2 and CHA2DS2-VASc scores for coronary artery lesions and in-hospital prognosis of patients with acute ST-segment elevation myocardial infarction. BMC Cardiovasc Disord 2021;21:439. [Crossref] [PubMed]
- Yılmaz S, Akboga MK. Is CHA2DS2-VASc Score Related to Inflammation in Patients With In-Stent Restenosis? Angiology 2018;69:90. [Crossref] [PubMed]
- Shehab A, AlHabib KF, Bhagavathula AS, et al. Clinical Presentation, Quality of Care, Risk Factors and Outcomes in Women with Acute ST-Elevation Myocardial Infarction (STEMI): An Observational Report from Six Middle Eastern Countries. Curr Vasc Pharmacol 2019;17:388-95. [Crossref] [PubMed]
- Lang Y, Ran X, Wang L, et al. Risk Factors of Death in Patients with Acute ST-segment Elevation Myocardial Infarction after PCI and the Combined Application of CTRP-1 with GRACE Score in Prognosis Evaluation of PCI Treated Patients. Sichuan Da Xue Xue Bao Yi Xue Ban 2019;50:941-5. [PubMed]
- Li Y. Risk factors of in-hospital death in patients with acute ST elevation myocardial infarction. Intern Emerg Med 2020;15:1335-7. [Crossref] [PubMed]
- Holovanova IA, Oksak GA, Tkachenko IM, et al. Risk factors associated with the occurrence of early complications of acute myocardial infarction after cardio-intervention treatment. Wiad Lek 2020;73:1245-51. [Crossref] [PubMed]
- Pryds K, Hjortbak MV, Schmidt MR. Influence of Cardiovascular Risk Factors, Comorbidities, Medication Use and Procedural Variables on Remote Ischemic Conditioning Efficacy in Patients with ST-Segment Elevation Myocardial Infarction. Int J Mol Sci 2019;20:3246. [Crossref] [PubMed]
- Zhang Z, Guo J. Predictive risk factors of early onset left ventricular aneurysm formation in patients with acute ST-elevation myocardial infarction. Heart Lung 2020;49:80-5. [Crossref] [PubMed]
- Obling L, Frydland M, Hansen R, et al. Risk factors of late cardiogenic shock and mortality in ST-segment elevation myocardial infarction patients. Eur Heart J Acute Cardiovasc Care 2018;7:7-15. [Crossref] [PubMed]
- Zhu WG, Xiong QM, Hong K. Meta-analysis of CHADS2 versus CHA2DS2-VASc for predicting stroke and thromboembolism in atrial fibrillation patients independent of anticoagulation. Tex Heart Inst J 2015;42:6-15. [Crossref] [PubMed]
- Yilmaz S, Yaylali YT, Kuyumcu MS, et al. Relationship between CHA2DS2-VASc and CHADS2 scores with pulmonary hypertension in patients with acute pulmonary embolism. Adv Respir Med 2019;87:203-8. [Crossref] [PubMed]
- Yu I, Song TJ, Kim BJ, et al. CHADS2, CHA2DS2-VASc, ATRIA, and Essen stroke risk scores in stroke with atrial fibrillation: A nationwide multicenter registry study. Medicine (Baltimore) 2021;100:e24000. [Crossref] [PubMed]


