Features and applications of energy devices for prone robot-assisted minimally invasive esophagectomy: a narrative review
Introduction
Robot-assisted minimally invasive esophagectomy (RAMIE) for esophageal cancer has rapidly become widespread since its first introduction by Kernstine in 2004 (1). Robot-assisted surgery is particularly useful in esophagectomy, which requires precise manipulation in the limited space of the thoracic cavity, because robotic systems have stable high-resolution three-dimensional (3D) and 10 times-enlarged imaging, tremor filtering, articulated instruments, and natural hand-eye coordination axis (2). Thus, robot-assisted surgery was recognized to be useful, providing precise lymphadenectomy with less bleeding (3). In addition, compared to conventional endoscopic surgery, RAMIE was reported to have equivalent oncological outcomes and lower incidence of morbidity (4,5).
In esophageal cancer surgery, damage to vital organs such as the aorta, pulmonary vein, and trachea may be fatal. In addition, precise and meticulous dissection is required, such as for preserving recurrent laryngeal nerve function, and it is imperative to understand the features of energy devices and maximize robotic advantages. However, there are not as many options for energy devices in robot-assisted surgery as there are in conventional endoscopic surgery. There have been reports mentioning surgical techniques of RAMIE, but few have referred to esophagectomy in terms of the features of energy devices. In this review article, we describe the features of various energy devices and the parts most suitable for manipulation in esophagectomy. We present the following article in accordance with the Narrative Review reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-559/rc).
Methods
A narrative search of Medline (PubMed interface) was performed for articles published using the keywords “robot-assisted esophagectomy”, “technique”, “postoperative complication”, and “short-term outcomes”. The search strategy was summarized in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | 20 July 2022 |
| Databases and other sources searched | Medline (PubMed interface) |
| Search terms used | Robot-assisted esophagectomy, technique, postoperative complication, short-term outcomes |
| Timeframe | From 1 January 2004 to 20 July 2022 |
| Inclusion and exclusion criteria | Inclusion criteria: Original Article, Research Article, Full paper, Studies included at least ten patients |
| Exclusion criteria: Editorial, Comments, Letters, Proceedings, Case reports, Non-English papers | |
| Selection process | Three authors (Noriyuki Hirahara, Takeshi Matsubara, Hikota Hayashi) independently conducted the selection process, assessed all the identified studies based on the eligibility criteria. If there were any disagreements, the inconsistencies were solved by another reviewer (Yoshitsugu Tajima) after discussion |
Features of various devices
Monopolar scissors
Monopolar scissors® (Intuitive Surgical, Inc., Sunnyvale, CA, USA) are electrocautery scissors with a sharp tip that enables the dissectible layer to be spread from a point to a line and then to a plane. The device has an articulating function that allows sharp dissection, ensuring a safety margin between adjacent organs, and faster incision, which maximize robotic advantages. In esophagectomy, the fibrous layer between organs is dissected, and a device with strong hemostatic ability is not essential. However, scissors-type devices cannot compress the organ, and their hemostatic ability is rather weak. Additionally, their limited ability to seal the lymphatic vessels may increase postoperative effusion.
Therefore, monopolar scissors demonstrate advantages in all surgical manipulations in esophagectomy. The advantages of robots with tremor filtering and motion scaling can be maximized in recurrent laryngeal lymph node dissection, which requires precise manipulation. Another advantage of monopolar scissors is that they can sharply dissect without an electrical source, as traction and thermal injury can cause recurrent laryngeal nerve palsy (6). However, because of the monopolar electrode, contact with adjacent organs may cause fatal damage and complications; therefore, effective use of the articulated instrument, tremor filtering, and motion scaling to avoid contact with adjacent organs is imperative (Figure 1).
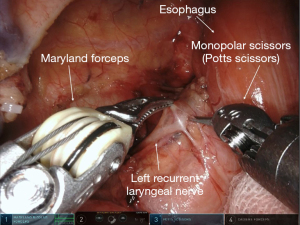
Maryland bipolar
Maryland bipolar forceps® (Intuitive Surgical, Inc., Sunnyvale, CA, USA) have a very thin tip, identical to monopolar scissors. They can be used for accurate dissection similar to monopolar scissors, and by closing the forceps to compress tissue and applying electric current, stronger hemostatic ability can be achieved. These forceps can be used at low- or high-voltage generator setting. At high voltage, the tissue is dissected by the spark between the forceps blades; at low voltage, the tissue is coagulated and denatured, and tension and clamp pressure are required for transection (7). Transpiration of moisture from the tissue when an electric current passes between the bipolar forceps tips results in transection; therefore, thermal effect on adjacent organs is minor. In addition, because of the shape of the tip, the bleeding point can be clamped and bleeding easily stopped (8). The disadvantage of Maryland bipolar forceps is that its use is time consuming because the forceps need to be constantly closed and reopened (Figure 2).
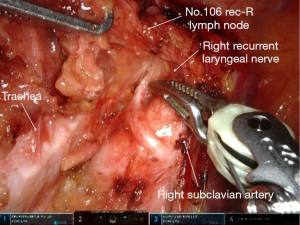
Long Maryland bipolar grasper® (Intuitive Surgical, Inc., Sunnyvale, CA, USA) is another feasible option. A notable difference between these forceps and Cadiere forceps is that if the hand control in the surgeon’s console is 30 degrees open, Cadiere forceps would be 30 degrees open; Maryland bipolar forceps would be 45 degrees open, and long Maryland bipolar grasper would be 70 degrees open. In other words, the opening angle of hand control in the surgeon’s console and the opening angle of most instruments in the patient cart are not the same, particularly in the case of the long Maryland bipolar grasper, which would be open at an angle that is more than twice that of the hand control. As such, it is necessary to operate with greater care when using these instruments. The tip of the long Maryland bipolar grasper is slightly blunt and unsuitable for precise dissection, but has the advantage of versatility because it can grip the tissue more delicately than fenestrated forceps. It is particularly suitable, for example, in tissue traction as forceps to be held in the operator’s left hand during recurrent laryngeal lymph node dissection (Figure 3).
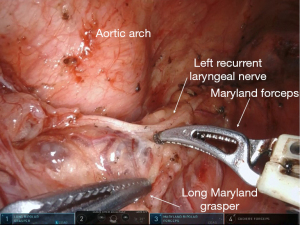
Thus, we believe that bipolar forceps can be used in all steps of esophagectomy procedures and can be used for resection by occasionally securing hemostasis using the clip, at the cost of longer surgical time.
Harmonic ACE curved shears
The ultrasonic scalpel is a popular choice of energy device not only in conventional endoscopic surgery but also in laparotomy and thoracotomy (9). Harmonic ACE Curved Shears® (Intuitive Surgical, Inc., Sunnyvale, CA, USA) can transect and coagulate tissues speedily without bleeding, and operation time is shortened. Because the device is manipulated using robotic instruments with tremor filtering, it can move more accurately than in conventional endoscopic surgery. However, since it uses ultrasonic vibration, it is structurally single swing forceps, one of the two jaws is articulated and the other is not, and fine dissection is impossible; the lack of articulating function is a major drawback for its use in robotic surgery. Furthermore, due to the structural requirement for ultrasonic vibration, the shaft length is approximately 12 cm shorter than that of other forceps. Therefore, depending on the patient’s physique, the device may not be able to reach the supradiaphragmatic region in some cases, and it may be necessary to change the manipulating robotic arm. In addition, the mist resulting from the use of this device is exaggerated because of the high-definition 3D camera used and may interfere with the surgical field view. To maintain a clear surgical field, the mist should be exhausted via a port away from the camera port or using other means (10). Although thermal spread to the surroundings is relatively narrow, activation time is increased as the amount of tissue to be grasped increases; this raises the temperature above that of the vessel sealer (≥100 ℃), and therefore, careful attention is warranted when used near vital organs (11). In addition, it should be noted that high-temperature steam containing large amount of moisture is generated during coagulation and transection of tissues, although the temperature is not as high as that of the vessel sealer (12).
The aforementioned features limit the suitable surgical manipulation steps for ultrasonic scalpels. This device is not suitable because dissection around the recurrent laryngeal nerve lymph nodes requires precise and meticulous manipulation. The ultrasonic scalpel is advantageous for the dissection of adhesions between the pericardium or right pulmonary vein and esophagus because the vector of the forceps coincides with the surface to be dissected. As these parts are the most affected by thermal injury, the device should be used with the utmost care considering that although thermal spread around the device is relatively narrow, cavitation is induced from the tip of the active blade (Figure 4).
Vessel sealer extend
The vessel sealer extend® (Intuitive Surgical, Inc., Sunnyvale, CA, USA), one of the most powerful hemostatic energy devices, is based on the principle of coagulation by bipolar electrodes. It performs coagulation and hemostasis with a pulsed output and transects the hemostatic tissue with an internal knife or tissue incision electrode (13). The jaws on both sides are articulated, and articulated instruments do not diminish the advantages of the robotic system, but the device tip is rather thick and unsuitable for precise manipulation. In addition, speedy manipulation is difficult because the tissue is transected only a few millimeters from the tip. Since the device has a strong sealing ability, it may seal even the dissected loose connective tissue layer. Furthermore, the relatively long length between the joint and tip may be an advantage or a disadvantage, depending on the surgical procedure. It is also important to note that the vessel sealer is a device that produces widespread high-temperature steam, although the surrounding tissue is unlikely to reach temperatures above 80 ℃ (9,11).
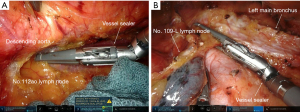
Therefore, the vessel sealer is highly recommended for lower mediastinal dissection that do not require manipulations as fine as those performed in the upper mediastinum. Dissection of the anterior thoracic paraaortic lymph node (No. 112aoA LN) can be easily and speedily performed using the articulated function to coagulate and dissect the proper esophageal artery (Figure 5A,5B). In addition, dissection of the No. 106tbL lymph node may be difficult in some cases because of the long length between the joint and tip, but careful lymph node dissection can minimize bleeding and shorten operation time. Furthermore, it is particularly useful for the transection of the border between the No. 110 and No. 111 lymph nodes in cases that do not require No. 111 lymph node dissection. This device is more suited for sharp transection of the endpoint of lymph node dissection, rather than for meticulous dissection, because of its powerful hemostatic force and blunt tip (14,15).
SynchroSeal
Improvements to the generator system have accelerated the sealing process and made it possible to use SynchroSeal® (Intuitive Surgical, Inc., Sunnyvale, CA, USA). SynchroSeal is intended for grasping, dissection, sealing and transection of tissue (13,16). SynchroSeal enables a secure seal and clean cut in vessels up to 5 mm in diameter with only 1–2 mm of lateral thermal spread, coupled with a faster cooldown time, helping the surgeon move onto the next task without unnecessary waiting time. In addition, the refined, curved jaw with 60° wristed articulation makes it easy to dissect and provides a secure tissue grasp (13,16). SynchroSeal offers enhanced efficiency through simplified operation and fast activation time. The disadvantage is that the sealed tissue cannot be cut off to the tip as well as the vessel sealer. Due to the slightly weaker cutting ability, it may be necessary to strain the tissue or rotate the device slightly.
As mentioned above, due to the tip of the SynchroSeal being finely divided as compared to that of the vessel sealer, it suitable for bilateral main bronchus lymph node and subcarinal lymph node excision, which requires relatively precise manipulation (Figure 6).
Discussion
It is important to understand and exploit the advantages of energy devices not only in robotic surgery but also in conventional surgery for safe and accurate dissection. Selecting the most appropriate device for use in each case and surgical situation is imperative.
Esophageal cancer is associated with a higher frequency of lymph node metastasis than other gastrointestinal cancers; additionally, the metastasis is widespread, necessitating reliable lymph node dissection. Furthermore, precise surgical techniques aimed at avoiding recurrent laryngeal nerve palsy and preserving function are needed, but there are restrictions on the movement of forceps due to the limited space between the ribs in thoracoscopic surgery. In addition, although there is a high risk of critical injury to other organs in conventional thoracoscopic surgery due to heartbeat and respiratory fluctuations, which are felt in the surgical field, robotic surgery with stable surgical field deployment and tremor filtering control seems to be the most suitable modality for esophagectomy.
In conclusion, monopolar scissors are suitable for precise and meticulous dissection, and sharp dissection using scissors without an electrical source is recommended to avoid secondary damage to adjacent organs in recurrent laryngeal lymph node dissection. Long Maryland bipolar grasper is suitable for use as grasping forceps, which can delicately grasp and dissect tissue. Vessel sealers, SynchroSeal, and ultrasonic scalpels have reliable hemostatic ability, making these devices suitable for sharp transection of the endpoint in lymph node dissection. SynchroSeal has particularly narrow lateral thermal spread, making it suitable for excision of the pericardium and pericardial surfaces. However, ultrasonic scalpels may have limited use due to the lack of articulating function.
Our article has several limitations. First, there are several reports of thermal spread to the surroundings in energy devices for conventional endoscopic surgery, but there are no reports on the temperature generated by robot energy devices and heat diffusion. Further experiments are required because the energy device generator used in robotic surgery is different from that in laparoscopic surgery. Second, different surgeons use the same device differently. It is important to be familiar with the features of the device and how to use it.
There are various problems, such as cost and time, in the process of changing forceps (17), but the field of robotic surgery is evolving rapidly, and improving technology and understanding its applications are essential to achieving the best performance. Prospective studies need to demonstrate the short- and long-term benefits of RAMIE, and cost-effectiveness in order to recommend robotic surgery. Robotic surgery can suppress postoperative complications which may lead to worsening prognosis.
Acknowledgments
The authors would like to thank Editage (http://www.editage.jp) for the English language review.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-559/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-559/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-559/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kernstine KH, DeArmond DT, Karimi M, et al. The robotic, 2-stage, 3-field esophagolymphadenectomy. J Thorac Cardiovasc Surg 2004;127:1847-9. [Crossref] [PubMed]
- Hussein AA, Mohsin R, Qureshi H, et al. Transition from da Vinci to Versius robotic surgical system: initial experience and outcomes of over 100 consecutive procedures. J Robot Surg 2022; Epub ahead of print. [Crossref] [PubMed]
- Angeramo CA, Bras Harriott C, Casas MA, et al. Minimally invasive Ivor Lewis esophagectomy: Robot-assisted versus laparoscopic-thoracoscopic technique. Systematic review and meta-analysis. Surgery 2021;170:1692-701. [Crossref] [PubMed]
- Babic B, Müller DT, Jung JO, et al. Robot-assisted minimally invasive esophagectomy (RAMIE) vs. hybrid minimally invasive esophagectomy: propensity score matched short-term outcome analysis of a European high-volume center. Surg Endosc 2022;36:7747-55. [Crossref] [PubMed]
- Fujita T, Sato K, Ozaki A, et al. Propensity-Matched Analysis of the Short-Term Outcome of Robot-Assisted Minimally Invasive Esophagectomy Versus Conventional Thoracoscopic Esophagectomy in Thoracic Esophageal Cancer. World J Surg 2022;46:1926-33. [Crossref] [PubMed]
- Hosoda K, Niihara M, Ushiku H, et al. Prevention of intra-thoracic recurrent laryngeal nerve injury with robot-assisted esophagectomy. Langenbecks Arch Surg 2020;405:533-40. [Crossref] [PubMed]
- Kikuchi K, Suda K, Shibasaki S, et al. Challenges in improving the minimal invasiveness of the surgical treatment for gastric cancer using robotic technology. Ann Gastroenterol Surg 2021;5:604-13. [Crossref] [PubMed]
- Shibao K, Joden F, Adachi Y, et al. Repeated partial tissue bite with inadequate cooling time for an energy device may cause thermal injury. Surg Endosc 2021;35:3189-98. [Crossref] [PubMed]
- Iovino F, Gatta G, Auriemma PP, et al. Late Shoulder-Arm Morbidity Using Ultrasound Scalpel in Axillary Dissection for Breast Cancer: A Retrospective Analysis. J Surg Res 2019;233:88-95. [Crossref] [PubMed]
- Balayssac D, Selvy M, Martelin A, et al. Clinical and Organizational Impact of the AIRSEAL® Insufflation System During Laparoscopic Surgery: A Systematic Review. World J Surg 2021;45:705-18. [Crossref] [PubMed]
- Hayami M, Watanabe M, Mine S, et al. Lateral thermal spread induced by energy devices: a porcine model to evaluate the influence on the recurrent laryngeal nerve. Surg Endosc 2019;33:4153-63. [Crossref] [PubMed]
- Hayami M, Watanabe M, Mine S, et al. Steam induced by the activation of energy devices under a wet condition may cause thermal injury. Surg Endosc 2020;34:2295-302. [Crossref] [PubMed]
- Ibanez Jimenez C, Lath A, Ringold F. Novel multifunctional robotically assisted bipolar instrument for simultaneous radiofrequency sealing and transection: preclinical and single-center experience. BMC Surg 2022;22:37. [Crossref] [PubMed]
- Zhang X, Su Y, Yang Y, et al. Robot assisted esophagectomy for esophageal squamous cell carcinoma. J Thorac Dis 2018;10:3767-75. [Crossref] [PubMed]
- Abaza R, Henderson SJ, Martinez O. Robotic Vessel Sealer Device for Lymphocele Prevention After Pelvic Lymphadenectomy: Results of a Randomized Trial. J Laparoendosc Adv Surg Tech A 2022;32:721-6. [Crossref] [PubMed]
- Morizane S, Honda M, Shimizu R, et al. Initial Experience of Robot-Assisted Adrenalectomy in Japan: What is the Optimal Selection of Robotic Forceps for Adrenalectomy? Yonago Acta Med 2022;65:176-80. [Crossref] [PubMed]
- Di Franco G, Lorenzoni V, Palmeri M, et al. Robot-assisted pancreatoduodenectomy with the da Vinci Xi: can the costs of advanced technology be offset by clinical advantages? A case-matched cost analysis versus open approach. Surg Endosc 2022;36:4417-28. [Crossref] [PubMed]