
A randomized comparison between the VivaSight double-lumen tube and standard double-lumen tube intubation in thoracic surgery patients
Introduction
One of the key characteristics of thoracic surgery is the need for mechanical separation of ventilation between the two lungs. One-lung ventilation (OLV) is performed to provide access to the surgical field or isolate the pathological process in the other lung (1). It is achieved with the use of a double-lumen tube (DLT) or a single-lumen tube with a bronchial blocker. In recent years, despite the introduction of several new bronchial blockers, DLT has remained the most common method of OLV (2). The design of conventional DLTs is also being modified and new concepts of tubes with special characteristics are introduced to clinical use (3). Still, the proper positioning of the DLT is crucial for safe conduct of anesthesia during one lung ventilation. The intraoperative prevalence of DLT malposition is high and repeated movement can cause the injury to the airways (4). The complications of DLT use may vary from light injuries of mucous membrane of bronchi to most severe airway ruptures (5).
To obtain proper DLT placement, which may in some cases be challenging, fiberoptic bronchoscopy (FOB) is applied as the gold standard since auscultation alone can be unreliable (6). In 2012, a new option for OLV with DLT was proposed: a video double-lumen tube (VDLT), which enables constant visualization of the trachea and carina during insertion, placement, and operation of the tube during OLV. Up to date, the clinical application of the VDLTs was presented in few prospective studies focusing on the FOB use comparison. Little is known regarding complications of VDLT intubation and use, as one trial was terminated early due to VDLT overheating (7-11).
We therefore tested the hypothesis that intubation with the VDLT (VivaSight 2DL, Ambu, Vallerup, Denmark) would be easier and faster than that with a standard DLT. We present the following article in accordance with the CONSORT reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-451/rc) (12).
Methods
This randomized, prospective, controlled study was approved by the Bioethics Committee of Medical University of Silesia in Katowice, Poland (identifier: KNW/0022/KB1/43/I/16). Written informed consent was obtained from all participants. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was registered in the ClinicalTrials.gov registry, ID: NCT04101734. The research was conducted in the Department of Anaesthesiology and Critical Care, Medical University of Silesia in Katowice, Poland, between June and October 2019. Eighty adult patients undergoing consecutive elective thoracic procedures requiring general anaesthesia and OLV with DLT were enrolled. Patients requiring emergency procedures with visible anatomic abnormalities and scheduled for awake fiberoptic intubation were excluded from the trial. The primary outcome measure for this study was time of intubation.
During routine preoperative anaesthetic visits, carried out at least 24 hours prior to the operation, an anaesthesiologist, one of the study team members, collected anamnesis and performed a physical examination. The patient’s age, sex, weight, body mass index, type of surgery, side of surgery, dentition, and history of difficult intubation were noted. The following anthropometric measurements were obtained:
- Thyromental height: the distance between the anterior border of the thyroid cartilage and the anterior border of the mentum was measured with an electronic depth gauge (21460605, Limit, Alingsås, Sweden) with the patient in the supine position and mouth closed. The cut-off point for difficult intubation prediction was proposed at 50 mm (13).
- Thyromental distance: the distance between the thyroid prominence and the most anterior part of the mental prominence of the mandible was measured with a centigrade ruler (Standard, Hoechstmass, Sulzbach, Germany) with the patient in the supine position, head fully extended, and mouth closed. The cut-off point for difficult intubation prediction was proposed at 6.5 cm (14).
- Sternomental distance: the distance between the superior border of the manubrium sterni and the bony point of the mentum was measured with a centigrade ruler (Standard, Hoechstmass) with the patient in the supine position, head fully extended, and mouth closed. The cut-off point for difficult intubation prediction was proposed at 12.5 cm (14).
- Modified Mallampati test: the oropharyngeal view was evaluated by using the modified Mallampati classification with the patient in the sitting position, mouth maximally open, tongue protruded, without phonation.
- Mouth opening: the mouth opening was measured as a distance between the lower and upper incisors with a tape measure (Standard, Hoechstmass). The patient was sitting with their mouth maximally open, tongue retracted, and without phonation. The cut-off point for difficult intubation prediction was proposed at 3.5 cm (14).
Several opaque, numbered randomization envelopes containing cards that read ‘VDLT’ or ‘DLT’ were prepared with a random number generator by a research team member not involved with anaesthesia or intubation. Only the patients were blinded to the allocation, as it was impossible to blind anaesthesiologists during the surgical procedures.
The anaesthesiologist performing the procedures in the operating theatre had a minimum of three years of experience in thoracic anaesthesia and OLV with both DLT and VDLT, and was blinded to the results of airway assessment.
All patients were anaesthetized in accordance with a standardized protocol. They were routinely monitored with an electrocardiogram, non-invasive arterial blood pressure measurement, and pulse oximetry before the induction of anaesthesia. Premedication was achieved with midazolam administered intravenously in a dose of 2 mg before the onset of anaesthesia. The patients were placed in the supine position on the operating table and pre-oxygenated with 100% oxygen breathed through a face mask for 5 min. General anaesthesia was induced with 2 mg/kg propofol and 2 µg/kg fentanyl. Muscle relaxation was accomplished with cis-atracurium in a dose 0.15 mg/kg and confirmed with muscular blockade monitoring when there were no palpable twitches in response to the train-of-four stimulation of the peripheral nerve. The direct laryngoscopy was performed in an optimal sniffing position, with an appropriate Macintosh blade size 3 or 4. If a technique modification was needed, the anaesthesiologist used a McCoy blade size 4, a video laryngoscope (McGrath MAC, Medtronic, Minneapolis, MN, USA), or a bougie (Single Use Bougie, Portex, Smiths Medical, Ashford, UK) in order to secure the airways.
In the DLT group, patients were then intubated with a left-side Robertshaw DLT size 35–39 (Shiley, Medtronic, Dublin, Ireland). The tube size was chosen depending on the patient’s height and gender (15); if any additional factors that could influence the choice existed, the anaesthesiologist decided on a different tube size. The intubation was defined as successful when the tube was introduced into the airways, the tracheal and bronchial cuffs were filled and the placement of the tube was confirmed with auscultation and capnography. If the tube was not inserted properly or was displaced during the intubation, after the repositioning or intraoperatively, FOB was performed for repositioning. The targeted position was achieved during FOB when the main carina and the bronchial cuff edge in the left bronchus were seen from the tracheal port. In this group, FOB was performed routinely in all cases after anaesthesia induction to confirm the proper tube position. Only the FOBs that led to repositioning of the tube were noted.
In the VDLT group, patients were intubated with a left-side VDLT size 35–39 (VivaSight 2DL, Ambu). The tube size was chosen in the same way as in the DLT group. Before the insertion, the tube was connected to the compatible monitor positioned beside the operating table. The patient was intubated and the introduction of the tube through the airways was observed on the monitor until the view of the main carina with the bronchial cuff edge in the left bronchus was established. In the case of a dissatisfactory view of the airways owing to excessive secretions, the camera port was repeatedly flushed with 0.9% saline and air. If the positioning of the tube was unsuccessful, FOB was performed in the same manner as in the DLT group. No routine FOB after anaesthesia induction to confirm the proper tube position was performed.
In both groups, the tubes were fixed with a bandage and the patients were placed in a lateral position, adequately to the operated side. During the operation, in the VDLT group, the view of the airways was monitored; in any case of dislocation, the position of the tube was readjusted. In the DLT group, if a dislocation of the tube was identified, FOB was performed, and the position of the tube was readjusted. Throughout the operation, the temperature at the edge of the tracheal port was continuously monitored with a thermometer (CarestationTM 600, GE, USA). During anaesthesia induction, the following variables were recorded: intubation time (measured from the beginning of direct laryngoscopy to the proper placement of DLT or VDLT in the respective groups), Cormack-Lehane grade (16), number of intubation attempts, subjective assessment of intubation difficulty (defined as easy, moderate, or difficult), technique modification (the use of a McCoy blade, video laryngoscopy, or a bougie), and tube size. Next, the events of DLT dislocation and FOB use (during intubation, after repositioning the patient, or intraoperatively) were noted throughout anaesthesia. When the chest wall was opened, the lung collapse was graded as follows: fully collapsed lung, non-collapsed lung with no visible ventilation, or fully ventilated lung. The temperature of the tracheal port area was measured at 15-minute intervals (Carestation 650, GE). In the VDLT group, the quality of the airways visualization was determined in the intraoperative period and graded as (I) full visualization of airways, (II) partial visualization of airways enabling correct VDLT positioning, (III) partial visualization of airways preventing correct VDLT positioning.
After the surgery, the patients were extubated, and the laryngeal mask was introduced to secure the airways to perform FOB and assess potential airway trauma. Trauma, defined as redness, oedema, haematoma, or active bleeding, was reported during FOB at the level of vocal cords, trachea, tracheal bifurcation, or main bronchus. Also, as part of a standard practice, the bronchial stump was examined for closure failure, and excessive secretions were suctioned.
After full emergence from anaesthesia, the patients were moved to the recovery room and were monitored for 2 hours; if no complications arose, the patients were then transferred to the Thoracic Surgery Ward. A member of the study team blinded to the results of the previous stages of the study visited the patient in the Thoracic Surgery Ward 24 hours after the surgery and recorded the occurrence of the following potential complications: sore throat (during swallowing or constant), cough (occasional or moderate), hoarseness of voice (noticed by the patient only or by the patient and the study team member).
Statistical analysis
The sample size was calculated by using the MedCalc software, version 14 (MedCalc, RRID:SCR_015044), to detect the area under the receiver operating characteristic (AUROC) curve of 0.70. The null hypothesis for the AUROC curve was set at 0.5. Finally, the minimum number of patients needed to provide a study power of 80% and alpha error of 0.05 equalled 62 (at least 31 cases per group).
Data in the interval scale were presented as mean ± standard deviation if normally distributed and as median (lower–upper quartile) in the case of non-normal or skewed distribution. The normality of the data distribution was assessed with the Shapiro-Wilk test and the quantile-quantile plot (Q–Q). Qualitative data are presented as numbers and percentages. The χ2 test was used to compare variables on the nominal and ordinal scales, including dichotomous ones, and the χ2 test with Yates’ correction (for two-way tables) was applied if the size of the expected number was smaller than 5. The two-group comparison was performed with the Student t-test for independent variables or the Mann-Whitney U test in accordance with the data distribution. Regarding primary outcome measure sensitivity analysis was performed including patients excluded from the study due to discontinued the intervention or that were lost to follow up. The temperature measurement analysis was based on the repeated measures analysis of variance with a post-hoc contrast analysis. Factors related to adverse events were determined with multivariable (backward stepwise) logistic regression. Parameters were considered statistically significant with P<0.05. The following software was used for calculations: Statistica 13.0 (STATISTICA, RRID:SCR_014213); Microsoft Office Excel (Microsoft Excel, RRID:SCR_016137).
Results
A total of 80 patients undergoing elective surgical procedures with the use of DLT for OLV who met the inclusion criteria were enrolled in this study. One patient was excluded from randomization owing to the withdrawal of consent before recruiting. Overall, 79 patients were subjected to randomization and were divided into 2 study groups: the DLT group (n=40) and the VDLT group (n=39). Eventually, after randomization, 8 participants were excluded from the trial: 1 patient from the DLT group was lost to follow-up and 7 patients from the VDLT were lost to follow-up or discontinued the intervention (Figure 1). From among the patients who discontinued the intervention in the VDLT group, 3 were transferred to the intensive care unit (ICU) for observation owing to comorbidities in the postoperative period, and 2 were scheduled for reoperation by the attending thoracic surgeon. These events prevented following the study protocol and proper postoperative evaluation of complications related to the use of VDLT and DLT, thus in these cases patients were excluded. Factors that influenced these two scenarios were not related to the study. Overall, 71 patients (44 males and 27 females) completed the trial. There were no significant differences regarding sex, age, or body mass index between the study groups. Furthermore, the statistics on surgical procedures, type of surgery, operated side, and operation time did not differ significantly. The demographic and clinical data are presented in Table 1.
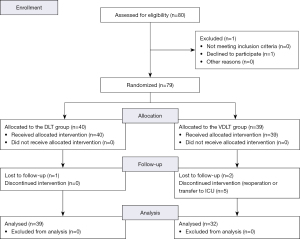
Table 1
| Parameter | DLT (n=39; 54.9%) | VDLT (n=32; 45.1%) | P |
|---|---|---|---|
| Female/male | 18/21 (46.2/53.8) | 9/23 (28.1/71.9) | 0.12 |
| Age (years) | 60±17 | 63±14 | 0.35 |
| Height (cm) | 168.6±9.6 | 171.7±8.4 | 0.11 |
| Body mass index (kg/m2) | 26.3±62 | 26.9±4.6 | 0.67 |
| The surgical procedure | |||
| Thoracotomy | 9 (23.1) | 9 (28.1) | 0.63 |
| Video thoracoscopy | 30 (76.9) | 23 (71.9) | |
| Operated side, left/right | 17/22 (43.6/56.4) | 9/23 (28.1/71.9) | 0.18 |
| Operation time (min) | 95±38 | 105±41 | 0.30 |
| Type of surgery | |||
| Lobectomy | 21 (53.8) | 19 (59.4) | 0.78 |
| Bilobectomy | 2 (5.1) | 2 (6.2) | |
| Wedge lung resection | 7 (18.0) | 3 (9.4) | |
| Other | 9 (23.1) | 8 (25.0) |
Data are presented as n (%) or mean ± standard deviation. DLT, double-lumen tube; VDLT, video double-lumen tube.
The preoperative analysis of difficult intubation predictive parameters, history of difficult intubation, and dentition also did not show significant differences between the groups (Table 2).
Table 2
| Parameter | DLT | VDLT | P |
|---|---|---|---|
| Mallampati scale | |||
| 1 | 10 (25.6) | 11 (34.4) | 0.72 |
| 2 | 17 (43.6) | 12 (37.5) | |
| 3 | 12 (30.8) | 9 (28.1) | |
| Thyromental distance (cm) | 9.14±1.56 | 9.55±1.54 | 0.28 |
| Sternomental distance (cm) | 17.76±2.35 | 17.84±1.90 | 0.86 |
| Thyromental distance ≥6.5 cm | 37 (94.9) | 30 (93.8) | 0.84 |
| Sternomental distance ≥12.5 cm | 39 (100.0) | 32 (100.0) | – |
| Thyromental height (mm) | 48.58±7.40 | 49.28±8.80 | 0.71 |
| Thyromental height ≥50 mm | 20 (51.3) | 16 (50.0) | 0.91 |
| Mouth opening (cm) | 4.95±0.60 | 5.09±0.90 | 0.44 |
| Mouth opening ≤3.5 cm | 0 (0.0) | 1 (3.1) | 0.45 |
| Full dentition | 11 (28.2) | 8 (25.0) | 0.76 |
| Upper partial dentition | 14 (35.9) | 11 (34.4) | 0.89 |
| Lower partial dentition | 13 (33.3) | 11 (34.4) | 0.93 |
| History of difficult intubation | 1 (2.6) | 0 (0.0) | 0.55 |
Data are presented as n (%) or mean ± standard deviation. DLT, double-lumen tube; VDLT, video double-lumen tube.
The assessment of the intubation procedure demonstrated that tube sizes 35 and 39 were used significantly more often in the DLT group and in the VDLT group, respectively. Meanwhile, no significant differences in the Cormack-Lehane grade of larynx visualization during direct laryngoscopy were noted between the study groups. Even though the number of intubation attempts and the need for technique modification did not differ, the time of intubation was significantly shorter in the VDLT group (P<0.001). Also, in the DLT group, intubation was more frequently described as difficult or moderate (P<0.05). The use of FOB to correctly position the tube during intubation and after repositioning the patient and intraoperatively was needed significantly more frequently in the DLT group (P<0.05). On the other hand, no significant differences were found in the assessment of OLV or the incidence of tube repositioning (Table 3). Additionally, due to high incidence of exclusion of the patients from the VDLT group (n=7) and DLT group (n=1) sensitivity analysis of primary outcome was performed. The comparison of intubation time including all randomized patients show similar results [DLT group: 125 (111–166) vs. VDLT group: 45 (33–67) s; P<0.001] as seen in primary analysis [DLT group: 125 (110–172) vs. VDLT group: 44 (33–66); P<0.001].
Table 3
| Parameter | DLT | VDLT | P |
|---|---|---|---|
| Tube size | |||
| 35 | 10 (25.6) | 1 (3.1) | <0.05* |
| 37 | 18 (46.2) | 14 (43.8) | |
| 39 | 11 (28.2) | 17 (53.1) | |
| Cormack-Lehane grade ≥2 | 25 (64.1) | 20 (62.5) | 0.89 |
| Cormack-Lehane grade I/II/III/IV | 14 (35.90)/19 (48.72)/5 (12.82)/1 (2.56) | 12 (37.50)/18 (56.25)/2 (6.25)/0 | – |
| Number of attempts ≥2 | 8 (20.5) | 3 (9.4) | 0.34 |
| Technique modification | 5 (12.8) | 1 (3.1) | 0.21 |
| Intubation grade | |||
| Easy | 17 (43.6) | 23 (71.9) | <0.05* |
| Moderate | 17 (43.6) | 8 (25.0) | |
| Difficult | 5 (12.8) | 1 (3.1) | |
| Intubation time (s) | 125 (110–172) | 44 (33–66) | <0.001* |
| Image quality I/II/III | – | 26/5/1 (81.3/15.6/3.1) | – |
| FOB | |||
| None | 31 (79.5) | 32 (100.0) | <0.05* |
| During intubation | 3 (7.7) | 0 (0.0) | |
| After patient repositioning | 3 (7.7) | 0 (0.0) | |
| Intraoperatively | 2 (5.1) | 0 (0.0) | |
| One-lung ventilation | |||
| Fully collapsed lung | 30 (76.9) | 27 (84.4) | 0.56 |
| Non-collapsed lung with no visible ventilation | 8 (20.5) | 5 (15.6) | |
| Ventilated lung | 1 (2.6) | 0 (0.0) | |
| Tube repositioning | |||
| None | 29 (74.4) | 17 (53.1) | 0.056 |
| After patient repositioning | 7 (17.9) | 14 (43.8) | |
| Intraoperatively | 3 (7.7) | 1 (3.1) |
Data are presented as n (%) or median (lower–upper quartile). *, statistically significant value. FOB, fiberoptic bronchoscopy; OLV, one-lung ventilation; DLT, double-lumen tube; VDLT, video double-lumen tube.
Table 4 depicts the complications after intubation with DLT vs. VDLT. The overall number or severity of the assessed complications did not differ significantly between the groups. The only exception was higher incidence of occasional cough in the DLT group and higher incidence of moderate cough in VDLT group (P<0.05). Regression and multi-factor model analysis did not demonstrate a significant impact on the incidence of reported complications among the studied factors.
Table 4
| Complications | DLT | VDLT | P |
|---|---|---|---|
| Overall, n (%) | 32 (82.1) | 26 (81.3) | 0.93 |
| Vocal cords trauma, n (%) | 4 (10.2) | 2 (6.2) | 0.59 |
| Trachea trauma, n (%) | 6 (15.4) | 1 (3.1) | 0.12 |
| Bifurcation of trachea trauma, n (%) | 9 (23.1) | 6 (18.8) | 0.88 |
| Main bronchus trauma, n (%) | 10 (25.6) | 4 (12.5) | 0.28 |
| Sore throat, n (%) | 12 (30.8) | 8 (25.0) | 0.78 |
| None | 27 (69.2) | 24 (75.0) | 0.73 |
| During swallowing | 9 (23.1) | 5 (15.6) | |
| Constant | 3 (7.7) | 3 (9.4) | |
| Hoarseness of voice, n (%) | 21 (53.8) | 16 (50.0) | 0.93 |
| None | 18 (46.2) | 16 (50.0) | 0.69 |
| Noticed by the patient | 12 (30.8) | 7 (21.9) | |
| Noticed by the patient and study team member | 9 (23.1) | 9 (28.1) | |
| Cough, n (%) | 14 (35.9) | 11 (34.4) | 1.00 |
| None | 25 (64.1) | 21 (65.6) | <0.05* |
| Occasional | 12 (30.8) | 4 (12.5) | |
| Moderate | 2 (5.1) | 7 (21.9) |
*, statistically significant value. DLT, double-lumen tube; VDLT, video double-lumen tube.
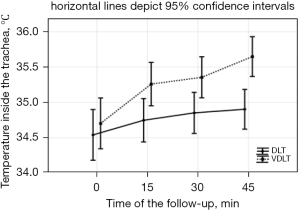
Two-way repeated-measures analysis of variance implied that the temperature measured in the trachea as a potentially hazardous factor for airway burns differed significantly between the study groups, as well as among the successive time points (P<0.05 and P<0.001, respectively) (Figure 2). A significant interaction between the group and time points was noted. The use of VDLT was associated with a greater temperature raise in consecutive time points. In both study groups, however, temperature increase in relation to the starting point (T0) was demonstrated in the following time points (P<0.001).
In univariable logistic regression, the following factors were included: type of tube used, body mass index, the Mallampati scale score, sternomental distance, thyromental distance, thyromental height, mouth opening, and the Cormack-Lehane scale score. Intubation with VDLT, in comparison with DLT, was characterized by a lower risk of difficult intubation (OR =0.30; 95% CI: 0.11–0.83; P<0.05), while higher values in the Cormack-Lehane scale (2 and 3) increased the risk of difficult intubation (OR =4.17; 95% CI: 1.37–12.64; P<0.05).
In the multivariable model, the relationship was similar in way and value: among the analysed parameters, only the use of VDLT was characterized by a lower risk of difficult intubation (OR =0.27; 95% CI: 0.09–0.79; P<0.05) and higher values in the Cormack-Lehane scale (2 and 3) increased the risk of difficult intubation (OR =4.67; 95% CI: 1.44–15.06; P<0.05).
Discussion
No significant differences between number of intubation attempts were found among studied groups; first attempt success in VDLT group was noted at 90.6%, whereas in DLT group 79.5%. On the other hand, the time required for tracheal intubation by using VivaSight DLT was significantly shorter than that for the standard DLT technique (median: 44 vs. 125 s). The intubation time in the DLT group included correct positioning of the tube as verified with the auscultation method and FOB in 3 cases (7.7%). Previous studies show similar results despite some differences in the applied methods: 54 vs. 156 s in a study by Onifade et al. (11), 51 vs. 264 s in a study by Levy-Faber et al. (7), and 36 s for VDLT in a study by Massot et al. (8). In the DLT group both the intubation time is longer and intubation graded as more difficult compared to VDLT group. The presented material is based on elective procedures only, what is also demonstrated in previous observational and prospective trials. The use of VDLTs is potentially beneficial in time-sensitive environments such as the emergency thoracic surgery procedures that require one lung ventilation. In this scenarios preparation and execution of FOB for correct tube placement might be time consuming and not readily available. The ease of use of VDLT might be helpful in procuring a fast, safe and dependable airway management in emergency procedures, however it is yet to be seen in future trials.
In the VDLT group, FOB application for correct tube positioning was not reported; in the DLT group, the incidence of FOB was reported in 8 (20.5%) cases overall. The incidence of FOB used for correct VDLT positioning in other studies is also very low, in some cases equalling 0%, too (5-11). Even though the incidence is low, VDLT may never substitute for FOB, and the availability of FOB is a necessity in the case of thoracic surgery (6). Cost-effectiveness analysis was performed by Larsen et al. (17); with the assumption of 6.6% incidence of additional FOB for tube positioning, the use of VDLT turned out favourable. A different approach is discussed by Templeton et al. (18), as the cost of maintaining FOB for immediate use may vary among institutions; with four times higher cost of VDLT compared with DLT for a single tube, the cost-effectiveness may not always be favourable.
Our results imply no significant differences between the study groups in the incidence of tube dislocation or quality of lung separation. The incidence of tube dislocation in VDLT group was as high as 43.1% after patient repositioning and 3.1% intraoperatively, whereas in DLT group 17.9% and 7.7% respectively. One of the biggest advantages of VDLT is the constant visualization of the tube position in the airways. In the case of standard DLT, when an unanticipated dislocation occurs the anaesthesiologist has to perform FOB to diagnose and correct the position of the tube. The preparation of equipment and execution of the procedure may be time consuming, occupy additional personnel and increase overall costs. These activities, especially when prolonged, may disturb the ventilation, cause hypoxia and affect the surgical field (19). Contrary, the constant visualization of the airways during repositioning, when the most of displacements takes place and intraoperatively, when the highest risk of complications occur may prevent the dislocation from happening. If the dislocation occurs the management of the issue is usually fast and simple. Taking into account results of our study with high incidence of displacement of the tubes this characteristic of VDLTs is a great clinical strength.
VDLT provides a constant view of the airways owing to an external monitor and a built-in camera with a LED source of light. In a study conducted by Massot et al. (8), the distal port overheating and melting occurred; thus, the trial was terminated prematurely. The manufacturer addressed this issue and implemented necessary corrective actions. However, because of the specificity of thoracic surgery and, sometimes, prolonged interventions, we decided, while assessing the possible VDLT complications, to perform temperature measurements near the tracheal port and the location of the camera and light source. Our results demonstrated higher temperature values in the VDLT group compared with the DLT group and a trend of temperature increase in time in the VDLT group; the absolute values did not exceed the hazardous level. We believe that further studies with a longer exposition time should be carried out to entirely exclude the possibility of burns and lesions due to the LED light or camera overheating.
In a study by Hegland et al. (20), DLT and VDLT dimensions were compared. Considerable differences were found in similarly sized tubes of different brands. When VDLT and a standard DLT (Mallinckrodt, Covidien, Tullamore, Ireland) in size 39 were examined, the median dimensions in specific regions turned out as follows: outer diameter measured at the proximal edge of the tracheal cuff: 14.8 mm for VDLT vs. 14.2 mm for DLT; outer diameter measured at the distal edge of the bronchial cuff: 10.2 mm for VDLT vs. 10.5 mm for DLT; distance measured from bifurcation to the tip of the tube: 355.5 mm for VDLT vs. 361.2 mm for DLT. What is more, a considerably larger cross-sectional area calculated at the proximal edge of the tracheal cuff was noted when comparing VDLT with a specified DLT (168.5 vs. 148.8 mm).
Our study did not indicate significant differences in the incidence of airway trauma between the analysed groups. This can be attributed to the fact that the size, mechanical properties, and process of insertion of VDLT do not differ significantly from those for DLT. In most cases, the lesions were located in the distal part of the airways, specifically in the left main bronchus and bifurcation of the trachea, and were not severe. The existing reports regarding this subject focus on more serious complications, such as airway ruptures, collected in a review by Liu et al. (5). In that material, airway rupture was located in the trachea (n=98, 52.4%) and left main bronchus (n=70, 37.4%); among the possible contributing factors, the authors enumerate the use of a stylet, cuff overdistention, oversized DLT, difficult intubation, and multiple attempts to position the DLT correctly.
As for the complications assessed postoperatively in our study, the severity was low with a medium overall prevalence. It is fairly consistent with the existing reports (7,8). Only small differences were noted in frequency of occasional and moderate cough between studied groups.
Our study has several limitations. One of our concerns is that even though the sample size was comparable to previous studies regarding use of VDLT it is still small [VDLT group (n=32) vs. DLT group (n=39)]. Further prospective, randomized trials should be conducted in order to evaluate possible clinical differences in the use of VDLTs compared to DLTs. What is more, this comparison would be ideally shown in multicentre studies what can greatly improve the impact of such evidence. As the use of VDLTs and DLTs is not the only way to perform one lung ventilation we are looking forward to see the comparisons between those means of OLV and bronchial blockers.
The study revealed that in the VDLT group, the tubes were significantly larger, as their size mainly depended on the height and gender of the patient. We believe that a deficit of females in this group (28.1% females vs. 71.9% males) may be responsible for this result. We perceive the gender imbalance between the VDLT and DLT groups as a source of bias and a limitation of our study. What is more, the small size of the tube is linked with higher risk of the tube displacement. Considering the dimensions of similarly sized tubes (20) these relations may lead to miscalculation of FOB usage.
We have noted high incidence of exclusion from final data analysis patients in the VDLT group (n=7), whereas in DLT group fewer patients were excluded (n=1). The reason behind exclusion was reoperation or transfer to the ICU. None of the causes of these events were due to airway management or anaesthesia complications, yet we did not gather further data, as it was outside of the study protocol. We see this as a limitation of our study. To limit the possible bias of primary outcome measure analysis we have performed sensitivity analysis including all randomized patients that showed similar results.
Our study shows no significant differences in preoperative assessment of the possible difficult intubation and Cormack-Lehane grade between studied groups. However, some differences in distribution of Cormack-Lehane grade may be clinically relevant and bias the findings of our study, as it can influence the intubation procedure.
Another limitation due to the design of study protocol was the impossibility to blind anaesthesiologists to the interventions and the devices. The relative high volume of thoracic procedures requiring OLV in our hospital makes the use of DLTs and VDLTs a part of routine practice. All study group members were experienced in these practices, however, the need for OLV may arise in different clinical settings and be addressed by different healthcare professionals (21). We see potential benefit of VDLT use in hospitals were the use of OLV is not a common practice and healthcare providers are not accustomed to routine use of DLTs, what is yet to be proven in future studies.
We see a potential source of bias in a part of the study that relied on subjective opinion of a study group member regarding the grade of intubation and a participant account of postoperative complications such as cough, harness of voice and sore throat.
Conclusions
In conclusion, the use of VDLT when compared with standard DLT offers reduced intubation time and is relatively easier. Also, the reduced need for FOB may improve the cost-effectiveness of VDLT application. In addition, constant visualization of the airways during the procedure allows to quickly correct or even prevent the tube malposition.
Acknowledgments
Funding: This work was supported by Wroclaw Medical University (SUB.E080.19.013. to JS).
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-451/rc
Trial Protocol: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-451/tp
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-451/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-451/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The trial was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ethics Committee of Medical University of Silesia in Katowice, Poland (identifier: KNW/0022/KB1/43/I/16) and informed consent was taken from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- McGrath B, Tennuci C, Lee G. The History of One-Lung Anesthesia and the Double-Lumen Tube. J Anesth Hist 2017;3:76-86. [Crossref] [PubMed]
- Narayanaswamy M, McRae K, Slinger P, et al. Choosing a lung isolation device for thoracic surgery: a randomized trial of three bronchial blockers versus double-lumen tubes. Anesth Analg 2009;108:1097-101. [Crossref] [PubMed]
- Kim N, Byon HJ, Kim GE, et al. A Randomized Controlled Trial Comparing Novel Triple-Cuffed Double-Lumen Endobronchial Tubes with Conventional Double-Lumen Endobronchial Tubes for Lung Isolation. J Clin Med 2020;9:977. [Crossref] [PubMed]
- Lieberman D, Littleford J, Horan T, et al. Placement of left double-lumen endobronchial tubes with or without a stylet. Can J Anaesth 1996;43:238-42. [Crossref] [PubMed]
- Liu S, Mao Y, Qiu P, et al. Airway Rupture Caused by Double-Lumen Tubes: A Review of 187 Cases. Anesth Analg 2020;131:1485-90. [Crossref] [PubMed]
- de Bellis M, Accardo R, Di Maio M, et al. Is flexible bronchoscopy necessary to confirm the position of double-lumen tubes before thoracic surgery? Eur J Cardiothorac Surg 2011;40:912-6. [Crossref] [PubMed]
- Levy-Faber D, Malyanker Y, Nir RR, et al. Comparison of VivaSight double-lumen tube with a conventional double-lumen tube in adult patients undergoing video-assisted thoracoscopic surgery. Anaesthesia 2015;70:1259-63. [Crossref] [PubMed]
- Massot J, Dumand-Nizard V, Fischler M, et al. Evaluation of the Double-Lumen Tube Vivasight-DL (DLT-ETView): A Prospective Single-Center Study. J Cardiothorac Vasc Anesth 2015;29:1544-9. [Crossref] [PubMed]
- Heir JS, Guo SL, Purugganan R, et al. A Randomized Controlled Study of the Use of Video Double-Lumen Endobronchial Tubes Versus Double-Lumen Endobronchial Tubes in Thoracic Surgery. J Cardiothorac Vasc Anesth 2018;32:267-74. [Crossref] [PubMed]
- Rapchuk IL, Kunju S, Smith IJ, et al. A six-month evaluation of the VivaSight™ video double-lumen endotracheal tube after introduction into thoracic anaesthetic practice at a single institution. Anaesth Intensive Care 2017;45:189-95. [Crossref] [PubMed]
- Onifade A, Lemon-Riggs D, Smith A, et al. Comparing the rate of fiberoptic bronchoscopy use with a video double lumen tube versus a conventional double lumen tube-a randomized controlled trial. J Thorac Dis 2020;12:6533-41. [Crossref] [PubMed]
- Moher D, Hopewell S, Schulz KF, et al. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c869. [Crossref] [PubMed]
- Panjiar P, Kochhar A, Bhat KM, et al. Comparison of thyromental height test with ratio of height to thyromental distance, thyromental distance, and modified Mallampati test in predicting difficult laryngoscopy: A prospective study. J Anaesthesiol Clin Pharmacol 2019;35:390-5. [Crossref] [PubMed]
- Roth D, Pace NL, Lee A, et al. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database Syst Rev 2018;5:CD008874. [Crossref] [PubMed]
- Slinger P. A view of and through double-lumen tubes. J Cardiothorac Vasc Anesth 2003;17:287-8. [Crossref] [PubMed]
- Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984;39:1105-11. [Crossref] [PubMed]
- Larsen S, Holm JH, Sauer TN, et al. A Cost-Effectiveness Analysis Comparing the VivaSight Double-Lumen Tube and a Conventional Double-Lumen Tube in Adult Patients Undergoing Thoracic Surgery Involving One-Lung Ventilation. Pharmacoecon Open 2020;4:159-69. [Crossref] [PubMed]
- Templeton TW, Morris BN, Royster RL. The Video Double-Lumen Endobronchial Tube: Is the Benefit Worth the Cost? J Cardiothorac Vasc Anesth 2018;32:275-6. [Crossref] [PubMed]
- Inoue S, Nishimine N, Kitaguchi K, et al. Double lumen tube location predicts tube malposition and hypoxaemia during one lung ventilation. Br J Anaesth 2004;92:195-201. [Crossref] [PubMed]
- Hegland N, Schnitzler S, Ellensohn J, et al. Dimensional Variations of Left-Sided Double-Lumen Endobronchial Tubes. Anesthesiol Res Pract 2019;2019:3634202. [Crossref] [PubMed]
- Pedersen CM, Green JS, Bigler DR, et al. Evaluation of time to intubation and rate of success for different healthcare professionals using a double-lumen left-sided endotracheal video tube: A prospective observational study. J Perioper Pract 2020;30:383-8. [Crossref] [PubMed]


