Primary pleural intermediate hemangioendothelioma with pleural effusion as the only manifestation
Introduction
Intermediate hemangioendothelioma is the term used to name those vascular tumors that show a borderline biological behavior between benign hemangiomas and malignant angiosarcomas. In the latest WHO/ISSVA classification, it is further subdivided into locally aggressive and rarely metastasizing hemangioendothelioma, including kaposiform hemangioendothelioma (KHE), retiform hemangioendothelioma (RHE), composite hemangioendothelioma (CHE) and pseudomyogenic hemangioendothelioma (PHE) (1,2). Generally, they are characterized by single or multiply solitary exo-endophytic cutaneous and soft tissue masses with slow growth. Therefore, primary pleural intermediate hemangioendothelioma presenting as pleural effusion only is exceedingly rare and also easily misdiagnosed.
Case presentation
A 48-year-old male presented with a one-month history of left-sided chest pain. Before his admission to our hospital, he was diagnosed as “tuberculous pleuritis” in the local clinic and was given oral administration of levofloxacin for 6 days. His symptoms achieved significant remission then. But 1 month later, chest pain recurred and even worsened. His medical history was type 2 diabetes mellitus for four years, and the medication included Glipizide and Xiaotangling capsule (a Chinese patent drug). He had a chronic tobacco-use history of 20 pack-years but quit it 3 years ago. Physical examination showed lymphadenectasis in bilateral supraclavicular fossa, moist rales in right lung, decreased breath sounds and percussion dullness in left lung. The patient’s social history, family history and review of system were otherwise unremarkable.
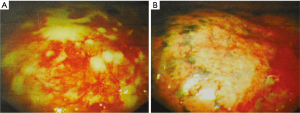
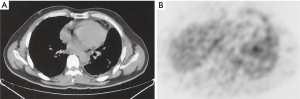
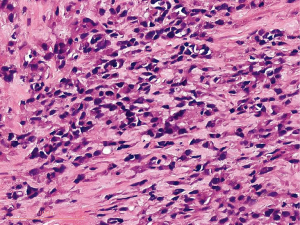
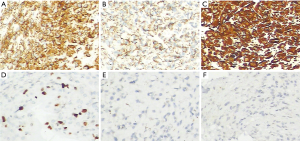
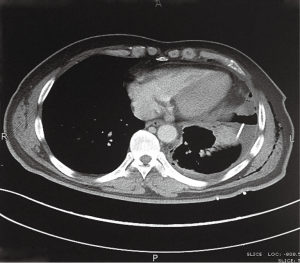
On admission, his blood examination revealed the following abnormal values: white blood cell count, 11.8×109/L (neutrophils 9.2×109/L); hemoglobin, 134 g/L; platelet count, 364×109/L; blood glucose, 7.98 mmol/L; erythrocyte sedimentation rate (ESR), 44 mm/h; serum anti-tuberculosis IgG antibody was positive while IgM antibody was negative; the tuberculin test showed the diameter of induration area was about 13 mm, referring to moderately positive. The liver function, renal function and serum tumor markers were in normal range, and [1,3]-β-D-glucan and galactomannan test were also negative. A thoracocentesis revealed a light-red and highly cellular exudative effusion which contained total protein 40.7 g/L, albumin 25.6 g/L, lactic dehydrogenase 301.0 U/L, adenosine deaminase 7.8 U/L. But no acid-resistant bacilli or neoplastic cells were found. Computed tomography (CT) scan of the chest (axial view) showed left-sided pleural effusion and patchy exudation shadows in left lung (Figure 1). To exclude the presence of malignant tumors, positron emission tomography (PET)/CT scan was performed, showing left-sided pleural thickening and a thick shadow with uneven density in the corresponding position (SUVmax =4.6), which suggested the possibility of benign lesions (Figure 2), and no evidence of extra-pleural lesion was noted. Subsequently a thoracoscopic pleural biopsy through medical thoracoscopy was performed. Lots of fibrinous exudation on pleura surface could be seen through thoracoscope (Figure 3). Pathology of the specimen revealed abnormally active proliferation of several spindle cells (Figure 4). These cells were positive for CD31, CD34, Ki67 (about 8%), vimentin, CD68 (focal) and factor VIII (sporadic), and negative for cytokeratin 5/6, cytokeratin 7, calretinin, epithelial membrane antigen, MC, napsin-A, P63, thyroid transcription factor-1, CD99, CD117 and S-100 (Figure 5).

The patient was finally diagnosed as primary pleural intermediate hemangioendothelioma on the basis of clinical manifestations, radiographic findings and histopathological examination. Neither radical resection nor systemic drug treatment was applied because the patient got great symptomatic remission after thoracentesis and drainage. His pleural effusion decreased significantly while patchy exudative shadows still remained in lung (Figure 6). During his follow-up for 10 months, there is no evidence of recurrence or metastasis.
Discussion
Intermediate hemangioendothelioma is a group of rare vascular tumors with intermediate grade of malignancy that can settle on any organ. Generally, they are slow-growing and flat masses commonly found in infants, children and young adults, and clinical appearance of the lesions includes nodules, plaques, and ulcerated tumors (3). However, pleural involvement or pleural effusion is very uncommon presentation. According to the published case reports, only 3 cases of intermediate hemangioendothelioma presented with pleural effusion. However, all of them did not arise in pleura initially and showed serious lesions in soft tissue (4-6). Our case is unique in that it is the first case of primary pleural intermediate hemangioendothelioma involving pleura only and presenting with pleural effusion. The mechanism of pleural effusion for intermediate hemangioendothelioma patients remains unknown. But it is recognized that these cases with or without pleura involvement can all developed pleural effusion, so we tentatively hypothesize that it is probably associated with pleural inflammation and obstruction of lymph circulation caused by these tumors.
Clinical recognition of intermediate hemangioendothelioma is troublesome because of its non-specific appearances. It has to be differentiated from hemangioma, angiosarcoma, blue-rubber bleb nevus syndrome, dermatofibrosarcoma protuberans and cutaneous metastases (7). In addition, differential diagnosis also includes mesotheliomas, metastases and tuberculosis if the tumor is originally located in pleura like our case. The definitive diagnosis is based on histopathologic examination.
Systemic treatment must be applied for patients with clinically significant lesions. The definitive treatment for them is surgical excision. Immunologic and chemotherapeutic agents are also the mainstay of therapy for KHE patients, such as corticosteroids, interferon-α, vincristine, cyclophosphamide, etc. In addition, radiotherapy is also confirmed to be effective in a few patients of KHE and RHE (8). But response to these treatment options is unpredictable and variable. In our case, surgery was unnecessary because of his mild and atypical symptoms, and other drug treatment wasn’t applied because the patient got great remission after drainage. Of great interest in this patient was the fact that his chest pain and pleural effusion almost disappeared and had never recurred during the 10-month follow-up, even though without any systemic treatment. That is, the patient got partly spontaneous regression. The mechanism of this interesting phenomenon remains unclear, and it may be attributed to self-limitation and extremely slow growth of this tumor. However, in view of the low-grade recurrence and malignancy of this tumor (8), a longer period of close follow-up for our patient is necessary although there is no evidence of recurrence so far.
In summary, this case highlights the fact that intermediate hemangioendothelioma can sometimes originate in and involve pleura only, which has never been reported before. This must be taken into consideration in the differential diagnosis of pleural effusion, especially for those patients who don’t show any other symptoms. Once the possibility of this rare tumor exists, histopathological examination is necessary to determine a definitive diagnosis. Personal treatment and close follow-up are needed due to the low-grade malignancy and recurrence of this tumor.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Jo VY, Fletcher CD. WHO classification of soft tissue tumours: an update based on the 2013 (4th) edition. Pathology 2014;46:95-104. [Crossref] [PubMed]
- Dasgupta R, Fishman SJ. ISSVA classification. Semin Pediatr Surg 2014;23:158-61. [Crossref] [PubMed]
- Adams DM, Hammill A. Other vascular tumors. Semin Pediatr Surg 2014;23:173-7. [Crossref] [PubMed]
- Wallenstein MB, Hole MK, McCarthy C, et al. Mediastinal kaposiform hemangioendothelioma and Kasabach-Merritt phenomenon in a patient with no skin changes and a normal chest CT. Pediatr Hematol Oncol 2014;31:563-7. [Crossref] [PubMed]
- Azma R, Alavi S, Khoddami M, et al. Multifocal kaposiform hemangioendothelioma of soft tissue with bilateral pulmonary involvement in an adolescent. Korean J Pediatr 2014;57:500-4. [Crossref] [PubMed]
- Chen RL, Chang PY, Hsu YH, et al. Recurrent life-threatening hemothorax in an infant with pleurocutaneous kaposiform hemangio-endothelioma. J Pediatr Hematol Oncol 2006;28:630-2. [Crossref] [PubMed]
- Mangham DC, Kindblom LG. Rarely metastasizing soft tissue tumours. Histopathology 2014;64:88-100. [Crossref] [PubMed]
- Requena L, Kutzner H. Hemangioendothelioma. Semin Diagn Pathol 2013;30:29-44. [Crossref] [PubMed]