
Surgical resection of mediastinal ectopic thyroid tissue: a case series
Highlight box
Key findings
• In this article, we present seven cases who underwent surgical resection of mediastinal ETT over the last 26 years at Stanford hospital.
What is known and what is new?
• Mediastinal ETT is a rare clinical entity that should be considered in the differential diagnosis of all mediastinal masses.
• Given the rarity of the condition, this case series reviews the clinical presentation, diagnostic workup and treatment for a large number of patients with ETT at a single institution to date.
What is the implication, and what should change now?
• With few recommendations and no guidelines in the literature, we recommend considering this diagnosis for a mediastinal mass and careful preoperative evaluation before surgical resection.
Introduction
Ectopic thyroid tissue (ETT) is defined as thyroid tissue located anywhere other than its normal anatomical location in the neck, adjacent to the trachea just below the larynx. ETT most commonly occurs secondary to a developmental abnormality involving variation from normal embryologic thyroid descent from the floor of the primitive foregut to its final location anterior to the trachea (1-3). The most common location for ETT is the base of tongue but locations include the submandibular or sublingual region, larynx, trachea, mediastinum, or even heart (2,4). ETT is a rare phenomenon with an overall prevalence of 1 per 100,000–300,000 in the general population, and 1 per 4,000–8,000 in patients with thyroid disease (5). It has been reported to be more common in women and can diagnosed at any age, but most cases are identified during childhood, adolescence and peri-menopause (6).
Thyroid function tests are recommended in patients with ETT, given that a high percentage of patients have evidence of hypothyroidism (7). To detect ectopic thyroid and evaluate for the presence of thyroid in its normal location, nuclear medicine radioiodine thyroid uptake scan is the most effective diagnostic tool. Ultrasound (US), computed tomography (CT), magnetic resonance imaging (MRI), and single photon emission computed tomography (SPECT) with CT (SPECT-CT) are additional modalities used to better delineate the location and extent of ectopic thyroid and for pre-surgical evaluation (5). If there is high concern for malignancy, fine needle aspiration (FNA) or tissue biopsy are recommended in patients with ETT (7).
There is no consensus about the optimal therapeutic strategy for ETT. Surgical resection of ETT depends on size, symptoms, risk of complications, and concern for malignant transformation. In cases with mild symptoms and hypothyroidism, treatment with levothyroxine may lead to significant mass size reduction and symptom relief. Asymptomatic euthyroid patients do not require any intervention and should be followed up for any clinical symptoms (5,8).
Mediastinal ectopic thyroid tissue is a rare subtype of ETT and accounts for approximately 1% of all ETT cases (6,9). Although it is a rare diagnosis, it should be considered in the differential diagnosis of all mediastinal masses, as it usually requires management and treatment different from those of other mediastinal masses. Here we retrospectively review our institution’s experience with patients who underwent surgical resection of mediastinal ETT. We present the following article in accordance with the AME Case Series reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-479/rc).
Case presentation
A search for “ectopic thyroid” was performed in the Stanford pathology database from 1996 to June 2021. Patients under 18 years of age and those with known history of thyroid neoplasm were excluded. Among a total of 202 specimens that were identified, seven were classified as mediastinal. These seven patients’ electronic medical records were then reviewed for demographics, preoperative evaluation, surgical procedure, and postoperative complications. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Stanford University Institutional Review Board, with protocol number 59223. Publication of this case series and accompanying images was waived from patient consent according to the Stanford University Institutional Review Board. We used descriptive statical analysis for this case series.
Patient demographics
We identified seven patients who underwent surgical resection for mediastinal ETT (Table 1). The mean age was 54 years (range, 30–75 years) at the time of surgery. Four of the patients were female.
Table 1
| Patient | Age (years)/sex | Initial presentation | Imaging finding | Pre-Op TSH (mIU/L) | Post-Op TSH (mIU/L) | Surgical indication |
|---|---|---|---|---|---|---|
| 1 | 67/M | Hoarseness, dysphagia | 2 cm upper mediastinal mass anterior to the trachea | N/A | N/A | Concern for malignancy (metastasis) |
| 2 | 52/M | Night sweats | 6 cm heterogenous mass, centered in the right paratracheal region with mild narrowing | N/A | N/A | Symptomatic |
| 3 | 30/F | Cough, chest pressure | 2.7 cm anterior mediastinal mass | N/A | 1.43 | Symptomatic |
| 4 | 34/F | Incidental | 4 cm mass adjacent to the lower pole of the right lobe of the thyroid | N/A | N/A | Concern for malignancy (thymoma) |
| 5 | 75/M | Neck pain | 5 cm well-circumscribed mass in the posterior mediastinum immediately posterior to the esophagus | 0.06 | 0.08 | Concern for malignancy (paraganglioma or neuroendocrine tumor due to heterogenous and highly vasculature nature and location) |
| 6 | 65/F | Chest pressure, neck pain, cough | 2.4 cm right paratracheal posterior mediastinal mass | 0.72 | 0.92 | Concern for malignancy (metastasis) |
| 7 | 46/F | Neck swelling, dysphagia | 3.3 cm enhancing soft tissue in the right tracheoesophageal groove | 1.2 | N/A | Symptomatic |
F, female; M, male; TSH, thyroid stimulating hormone; N/A, not applicable; Op, operation.
Clinical presentation
Chest pressure and cough were reported in two patients. One patient had worsening hoarseness and occasional dysphagia for six months. Two patients reported neck pain (one after a mechanical fall), which led to further work up. One patient noticed swelling at the right base of the neck followed by dysphagia. Two of the patients had no significant presenting symptoms and the thoracic mass was an incidental finding, but in further investigations, one reported intermittent night sweats.
Thyroid function tests were checked in four of the cases. Two of the patients had thyroid stimulating hormone (TSH) checked before and after surgery, one only before surgery, and one only after surgery. All TSH values were within normal limits.
Before surgery, ectopic thyroid was a possibility in all patients, but no one had a biopsy proven diagnosis. Patient 2 underwent mediastinoscopy and Patient 6 underwent endobronchial ultrasound (EBUS) guided biopsy. For Patient 1, the surgeon noted a clinical diagnosis of ectopic thyroid, although there was also concern for malignancy. In four patients, there was a concern for malignancy. Patients 1 and 6 had a history of malignancy and there was concern for metastasis. Patient 4 had an anterior mediastinal mass concerning for thymoma. Patient 5 had a heterogeneous and highly vascular mass concerning for paraganglioma or neuroendocrine tumor.
Radiology
Details are summarized in Table 1. All patients in our study underwent CT scans of the chest. Locations of ETT, using the 4-compartment model of the mediastinum (10), included three lesions in the superior mediastinum, one anterior, one middle, and two in the posterior mediastinum. The mean lesion diameter was 3.6 cm (range, 2–6 cm).
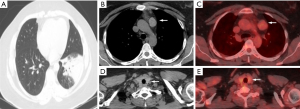
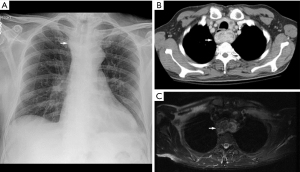
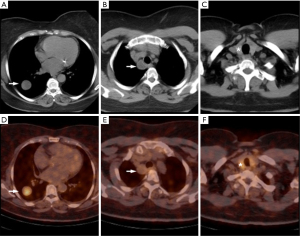
Patient 1 underwent thyroid uptake scan which revealed radioactive iodine uptake, suggesting that the mediastinal lesion was probably thyroid tissue. Patient 3 underwent fluorodeoxyglucose positron emission tomography computed tomography (FDG PET-CT) scan, which showed mild increase in size of the known homogeneous anterior mediastinal soft tissue mass (Figure 1). Patient 5 underwent a cervical MRI after a fall which revealed the 6.9 cm prevertebral heterogeneously enhancing mass (Figure 2). Patient 6 presented with right lung neuroendocrine tumor, as demonstrated by dotaTATE-PET-CT scan, with lack of avidity of the posterior mediastinal mass (Figure 3).
Surgical resection
Surgical approach varied by location. Two of the superior mediastinal ETT were resected through a cervical approach, and the remaining one resected through a median sternotomy, combined with a cardiac valve operation. The remaining four mediastinal ETT were resected through the chest, two with a robot-assisted approach and two with a posterolateral thoracotomy. One of the patients who had a robot-assisted approach had a combined lobectomy for neuroendocrine tumor. One of the patients who had a thoracotomy was converted from a video-assisted approach due to bleeding that was subsequently easily controlled.
In three cases, the surgeons noted that the ETT was not adherent to surrounding structures; in the remaining cases, they did not remark on the adherence or difficulty. All the masses were found to be separate from the thyroid gland on pathology with no connecting tissue noted by either the surgeon or pathologist. For Patient 3, the anterior mediastinal ETT was resected en bloc with the thymus and pericardial fat, and the others were completely excised with no additional margin.
The mean length of stay was 4.3 days (standard deviation, 1.8 days). There was only one postoperative complication. Patient developed a chyle leak that resolved with conservative management, as well as phrenic nerve injury that did not require intervention.
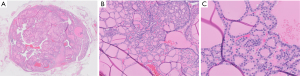
Pathology
Histopathology of the mediastinal mass revealed thyroid epithelium arranged as variably sized follicles with colloid, and bland follicular epithelial cells with round, well-spaced nuclei, characterized by speckled chromatin and scant delicate cytoplasm. There were no features of classic papillary thyroid carcinoma, including enlarged pale nuclei, irregular nuclear contours, longitudinal nuclear grooves, intranuclear pseudoinclusions, or dense squamous cytoplasm are seen. There was no marked cytologic atypia, elevated mitotic activity, or necrosis (Figure 4).
Discussion
Mediastinal ETT is a rare clinical entity that should be considered in the differential diagnosis of all mediastinal masses, requiring individualized management and treatment. In our retrospective review of seven patients who underwent surgical resection of mediastinal ETT over a 26-year period at our institution, we found some commonalities but many differences. With few recommendations and no guidelines in the literature, we recommend considering this diagnosis for a mediastinal mass and careful preoperative evaluation before surgical resection.
Mediastinal ectopic thyroid masses are often asymptomatic and incidentally identified on imaging studies (11-22). Some cases exhibit compressive symptoms such as: dyspnea (9,22), cough (6), difficulty in swallowing (23-25), voice hoarseness (23), and chest pain (6). In our patients, the indication for surgery was either compressive symptoms or concern for malignancy.
Thyroid function tests are recommended in patients with ETT given that high percentage of patients with lingual ETT have evidence of hypothyroidism (3,26). In reports of mediastinal ectopic thyroid masses, most cases were found to be euthyroid (27-29). However, both hypothyroidism and hyperthyroidism have been reported (30). Similarly, all four cases in which TSH levels were checked were found to be euthyroid.
The differential diagnosis for mediastinal mass is broad and include thymoma, germ cell tumors, lymphoma, neurogenic tumors, benign cysts, lipoma, esophageal lesions, paragangliomas, metastases, and mediastinal ETT (31). Imaging can help distinguish ectopic thyroid tissue from other lesions found in the mediastinum. Similar to the thyroid, ectopic thyroid generally demonstrates higher density on CT, as measured in Hounsfield Units (HU), due to physiologic intra-cellular accumulation of iodine in functional follicular thyroid cells. HU values of 70±10 in thyroid tissue are typically seen on CT performed without intravenous contrast (32). On MRI, normal thyroid tissue exhibits iso-intense to slightly hyper-intense homogeneous signal intensity on T1 and T2-weighted images as compared to adjacent muscle. Thyroid tissue typically exhibits avid intravenous contrast enhancement on CT and MRI, due to its highly vascular nature. Mediastinal ectopic thyroid tissues are not typically visualized using ultrasound (US), due to their atypical locations and difficulty in accessing sonographic windows to the mediastinum. Functional nuclear medicine radioiodine imaging using I-123 or I-131 can show the iodine-avid nature of suspected ectopic thyroid tissue, and thus enabling high confidence for ETT. Although uptake and retention in rebound thymic tissue and in esophagus and esophageal diverticula can result in false-positive reading (6,33). Use of cross-sectional SPECT with CT correlation enable improved anatomic evaluation and spatial localization of over planar imaging (33).
Definitive imaging of ectopic thyroid tissue can obviate surgery. Three of our cases were rare scenarios in which CT was not definitive. In the third case, the lesion was distant from the thyroid and in a location more typical for thymic lesions, and the lesion showed relative lower density than expected for thyroid tissue at 50 HU. In the fifth case, the lesion’s heterogenous and highly vasculature nature and location in the middle mediastinum elicited considerations for other rare pathologies such as paraganglioma and neuroendocrine tumor, which in retrospect, reflected goitrous change of the ectopic thyroid tissue. In the sixth case, the lesion was found along the lymphatic drainage pathway of a diagnosed lung carcinoid tumor which increased clinical impetus for definitive resection. Imaging characteristics that are similar to the normally positioned thyroid can help confirm ETT. Although the sixth cases is one exception, in which the cystic nature of the ETT led to imaging characteristics that are different from the normal thyroid.
Currently, there is not consensus on the optimal therapeutic strategy for the management of mediastinal ectopic thyroid due to rare prevalence of this entity and variable clinical course. Most publications recommend surgical resection based on the patient’s age, size, local or compressive symptoms, thyroid function status, and complications of the mass (ulceration, bleeding, or risk of malignancy) (3). Some authors recommend surgical resection for all ETT cases given the possibility, albeit low, of malignant transformation (34,35). Symptomatic mediastinal ETT is managed surgically either through thoracotomy or sternotomy (36), and more recently, with minimally invasive approaches. Majority of our cases were symptomatic and there was concern for malignancy in four cases based on the medical history. Mediastinal ETT has been reported to imitate metastases (37). One of the limitations of the study is that we reviewed pathology database, so we do not have a comparison group for non-surgical patients.
Malignant transformation of ETTs happens very rarely and has been reported in few case reports (34,35,38,39). Most cases are diagnosed after surgical resection and based on the histopathologic examination. Hu et al. reported a case of papillary carcinoma in a mediastinal ETT diagnosed by endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) (35). Two of our cases also underwent biopsy of the mediastinal masses. In the second case, the biopsy result was nondiagnostic and in the sixth case, it revealed bland cystic lesion. Finally, all of our patients underwent surgical resection of their mediastinal masses, with pathology demonstrating ectopic thyroid tissue and negative for malignancy in all samples.
Conclusions
Ectopic mediastinal thyroid tissue is a rare clinical entity that should be considered in the differential diagnosis of all mediastinal masses, requiring individualized management and treatment. Diagnostic imaging with radioactive iodine uptake scan and thyroid function should be checked pre-operatively if there is a high suspicion for ETT. All patients with confirmed ETT should undergo post-operative thyroid function evaluation.
Acknowledgments
The abstract of this study was presented as a poster at the American Thyroid Association annual meeting, September 30-October 3, 2021.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-479/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-479/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-479/coif). Natalie Lui reports consulting fees from Intuitive Surgical and a research grant from Intuitive Foundation. Natalie Lui serves as an unpaid editorial board member of Journal of Thoracic Disease from September 2021 to August 2023. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Stanford University Institutional Review Board, with protocol number 59223. Publication of this case series and accompanying images was waived from patient consent according to the Stanford University Institutional Review Board.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Di Benedetto V. Ectopic thyroid gland in the submandibular region simulating a thyroglossal duct cyst: a case report. J Pediatr Surg 1997;32:1745-6. [Crossref] [PubMed]
- Adelchi C, Mara P, Melissa L, et al. Ectopic thyroid tissue in the head and neck: a case series. BMC Res Notes 2014;7:790. [Crossref] [PubMed]
- Noussios G, Anagnostis P, Goulis DG, et al. Ectopic thyroid tissue: anatomical, clinical, and surgical implications of a rare entity. Eur J Endocrinol 2011;165:375-82. [Crossref] [PubMed]
- El Haj NI, Hafidi S, Khoaja A, et al. Ectopic mediastinal thyroid removed by U-VATS approach. A case report. Int J Surg Case Rep 2021;78:284-7. [Crossref] [PubMed]
- Ozturk A, Cicek T, Aktas Z, et al. Mediastinal ectopic thyroid diagnosed by endobronchial ultrasound-guided transbronchial needle aspiration: Report of three cases. J Clin Ultrasound 2018;46:299-301. [Crossref] [PubMed]
- Regal M, Kamel MM, Alyami H, et al. Mediastinal ectopic thyroid mass with normal thyroid function and location: Case report. Int J Surg Case Rep 2018;52:5-7. [Crossref] [PubMed]
- Alanazi SM, Limaiem F. Ectopic thyroid. StatPearls. Treasure Island (FL): StatPearls Publishing, 2020.
- Hummel J, Wachsmann J, Carrick K, et al. Ectopic Thyroid Tissue in the Mediastinum Characterized by Histology and Functional Imaging with I-123 SPECT/CT. Case Rep Radiol 2017;2017:9084207. [Crossref] [PubMed]
- Spinner RJ, Moore KL, Gottfried MR, et al. Thoracic intrathymic thyroid. Ann Surg 1994;220:91-6. [Crossref] [PubMed]
- Liu W, Deslauriers J. Mediastinal divisions and compartments. Thorac Surg Clin 2011;21:183-90. viii. [Crossref] [PubMed]
- Mussak EN, Kacker A. Surgical and medical management of midline ectopic thyroid. Otolaryngol Head Neck Surg 2007;136:870-2. [Crossref] [PubMed]
- Gamblin TC, Jennings GR, Christie DB 3rd, et al. Ectopic thyroid. Ann Thorac Surg 2003;75:1952-3. [Crossref] [PubMed]
- Kim SY. A Case of Right Paratracheal Ectopic Thyroid, Mimicking Metastasis on CT and 18F-FDG PET CT. Open J Med Imaging 2013;03:82-5. [Crossref]
- Abdel Aal M, Scheer F, Andresen R. Ectopic mediastinal thyroid tissue with a normally located thyroid gland. Iran J Radiol 2015;12:e7054. [PubMed]
- Mace AD, Taghi A, Khalil S, et al. Ectopic sequestered thyroid tissue: an unusual cause of a mediastinal mass. ISRN Surg 2011;2011:313626. [Crossref] [PubMed]
- Uludag M, Isgor A, Yetkin G, et al. Ectopic mediastinal thyroid tissue: cervical or mediastinum originated? BMJ Case Rep 2009;2009:bcr09.2008.1004.
- Topcu S, Liman ST, Elicora A, et al. A difficult case: ectopic thyroid, bronchial anomalies, and incidentaloma in a patient with lung carcinoma. J Thorac Cardiovasc Surg 2009;138:231-3. [Crossref] [PubMed]
- Wu MH, Chen KY, Liaw KY, et al. Primary intrathoracic goiter. J Formos Med Assoc 2006;105:160-3. [Crossref] [PubMed]
- Siddique M, Bashir H. 99mTc Sodium Pertechnetate Uptake in Ectopic Mediastinal Thyroid Tissue on Hybrid Thyroid Scintigraphy. Clin Nucl Med 2018;43:820-2. [Crossref] [PubMed]
- Kim DH, Kim DW, Shin GW, et al. Nodular hyperplasia presenting as a mediastinal mass: Three case reports. Medicine (Baltimore) 2018;97:e12050. [Crossref] [PubMed]
- Zhang W, Zhang H, Hou Q, et al. Ectopic thyroid microfollicular adenoma in the lung: A case report. Medicine (Baltimore) 2019;98:e16832. [Crossref] [PubMed]
- Kesici U, Koral Ö, Karyağar S, et al. Missed retrosternal ectopic thyroid tissue in a patient operated for multinodular goiter. Ulus Cerrahi Derg 2016;32:67-70. [Crossref] [PubMed]
- Chaudhry IU, Cheema AI, AlShamasi Z, et al. Hoarseness of voice, respiratory distress and dysphagia due to giant primary posterior mediastinal ectopic goitre: a rare clinical entity. BMJ Case Rep 2016;2016:bcr2016215132. [Crossref] [PubMed]
- Demirhan R, Onan B, Oz K, et al. Posterior mediastinal ectopic thyroid: an unusual cause for dysphagia. Ann Thorac Surg 2009;88:656-9. [Crossref] [PubMed]
- Walz PC, Iwenofu OH, Essig GF. Ectopic mediastinal goiter successfully managed via cervical approach: case report and review of the literature. Head Neck 2013;35:E94-7. [Crossref] [PubMed]
- Neinas FW, Gorman CA, Devine KD, et al. Lingual thyroid. Clinical characteristics of 15 cases. Ann Intern Med 1973;79:205-10. [Crossref] [PubMed]
- Roh E, Hong ES, Ahn HY, et al. A case of mediastinal ectopic thyroid presenting with a paratracheal mass. Korean J Intern Med 2013;28:361-4. [Crossref] [PubMed]
- Metere A, De Giacomo T, Vergine M, et al. Diagnosis and management of a mediastinal ectopic thyroid laying on the right bronchus: case report and review of literature. BMC Surg 2018;18:19. [Crossref] [PubMed]
- Thuillier F, Venot J. Ectopic thyroid tissue in the anterior mediastinum with a normally located gland: a case report. Ann Endocrinol (Paris) 2012;73:34-6. [Crossref] [PubMed]
- Santangelo G, Pellino G, De Falco N, et al. Prevalence, diagnosis and management of ectopic thyroid glands. Int J Surg 2016;28:S1-6. [Crossref] [PubMed]
- Juanpere S, Cañete N, Ortuño P, et al. A diagnostic approach to the mediastinal masses. Insights Imaging 2013;4:29-52. [Crossref] [PubMed]
- Zander DA, Smoker WR. Imaging of ectopic thyroid tissue and thyroglossal duct cysts. Radiographics 2014;34:37-50. [Crossref] [PubMed]
- Oh JR, Ahn BC. False-positive uptake on radioiodine whole-body scintigraphy: physiologic and pathologic variants unrelated to thyroid cancer. Am J Nucl Med Mol Imaging 2012;2:362-85. [PubMed]
- Sand J, Pehkonen E, Mattila J, et al. Pulsating mass at the sternum: a primary carcinoma of ectopic mediastinal thyroid. J Thorac Cardiovasc Surg 1996;112:833-5. [Crossref] [PubMed]
- Hu J, Li M, Xu L. Ectopic thyroid cancer diagnosed by endobronchial ultrasound-guided transbronchial needle aspiration. Thorac Cancer 2017;8:703-5. [Crossref] [PubMed]
- Sakorafas GH, Vlachos A, Tolumis G, et al. Ectopic intrathoracic thyroid: case report. Mt Sinai J Med 2004;71:131-3. [PubMed]
- Tsai A, Rafferty W, Ren S. Mediastinal ectopic thyroid tissue, an imitator of an enlarged lymph node with metastatic pulmonary neoplasia. Diagn Cytopathol 2021;49:E471-4. [Crossref] [PubMed]
- Ranaldi R, Morichetti D, Goteri G, et al. Immature teratoma of the mediastinum arising in ectopic thyroid tissue: a case report. Anal Quant Cytol Histol 2009;31:233-8. [PubMed]
- Lianos G, Bali C, Tatsis V, et al. Ectopic thyroid carcinoma. Case report. G Chir 2013;34:114-6. [PubMed]


