
Narrowing the therapeutic window?—A case-control study on the influence of the COVID-19 pandemic on the primary UICC stage of NSCLC
Highlight box
Key findings
• The SARS-CoV-2 pandemic led to a delay in the diagnosis of non-small cell lung cancer (NSCLC). This resulted in higher UICC stages upon diagnosis.
• No pandemic phase showed a significant difference in operability of NSCLC.
• Sole implementation of security measures such as the imposed curfews had no negative impact on the diagnosis of NSCLC.
What is known and what is new?
• Clinical experience suggests a drop in diagnosis and treatment of lung cancer during the second and third waves of the SARS-CoV-2 pandemic. Early diagnosis of NSCLC is crucial in surgical therapeutic regimes.
• No increase in inoperable stages was shown. The results indicate that already inoperable stages shifted to higher staged cases.
• The effect of securitization on NSCLC progress seems negligible during the SARS-CoV-2 pandemic.
What is the implication, and what should change now?
• The shift of tumor stages very likely influenced the prognosis. Future investigations should study long-term effects on prognosis.
Introduction
The pandemic spread of SARS-CoV-2 has influenced every area of patient care. Clinical experience of German thoracic surgeons suggests a drop in diagnosis and treatment of lung cancer during the second and third waves of the pandemic. This is consistent with results from retrospective analyses of cancer registers showing a decrease in cancer-related medical consultations during the pandemic in various countries (1-3). This decline may be associated with a significant delay in diagnosis and later tumor stages in the initial diagnosis. Early diagnosis of non-small cell lung cancer (NSCLC) is crucial in the therapeutic regime facing that early staged NSCLC is potentially curable by operation alone or combined therapy. Lung cancer remains the most common cause of cancer deaths accounting for approximately 1.8 million deaths worldwide in 2020 (4). Besides severe individual suffering, late-stage lung cancer has a significant socioeconomic impact. Extrapolation models proved the considerable health and economic burden of delayed cancer diagnosis and treatment during the COVID-19 pandemic (5). The authors estimated that delayed diagnosis of lung cancer by 3 or 6 months would result in progress of 2.1% and 8% leading to a loss of 44 or 98 years in a 5-year time horizon, respectively (5). It is well known that COVID-19 had a tremendous impact on patient care, workflow, and diagnostic as well as therapeutic standards of thoracic surgery clinics leading to a change in staff composition of interdisciplinary tumor boards, prolonged diagnostic workup, a decrease in surgical activity and modification of standard protocols (6-8). However, data on the extent of diagnostic prolongation and whether it influenced the therapeutic regime is rare. This study aims to identify how COVID-19 affected the distribution of the Union for International Cancer Control (UICC) stage in NSCLC at first diagnosis. We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1091/rc).
Methods
A retrospective case-control study was conducted, including all patients receiving the first diagnosis of NSCLC in the regions of Leipzig and Mecklenburg-Vorpommern (MV) between January 2019 and March 2021. Patient data were retrieved from clinical cancer registries of the city of Leipzig and the federal state of MV. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval for this retrospective evaluation of archived, anonymized patient data was waived by the Scientific Ethical Committee at the Medical Faculty, Leipzig University. Informed consent from patients was not needed as the data was anonymized.
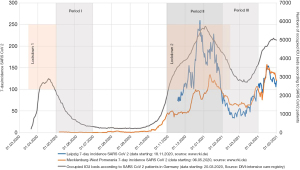
Three investigation periods were defined to study the effects of enacted security measures and a high caseload of SARS-CoV-2 separately and combined.
- Period I (curfew without high incidences, May 1st to June 30th, 2020): during the initial phase of the SARS-CoV-2 pandemic, Germany enacted national wide security measures such as curfews to contain the infectious spread. However, the incidence of SARS-CoV-2 was initially low in Leipzig and MV. The aftermath of this phase is set as Period I, investigating the effects of imposed security measures without the overload of the health system due to high incidences.
- Period II (curfew and high incidences, November 1st, 2020, to January 31st, 2021): SARS-Cov-2 caseload increased substantially in autumn 2020. The number of intensive care unit (ICU) beds occupied by SARS-CoV-2 patients multiplied dramatically. The German government imposed a second curfew. This phase was selected as Period II to study the effects of high occupancy rates of health services in combination with imposed nationwide security measures.
- Period III (aftermath of curfew and high incidences, February 1st to March 31st, 2021): period III is defined to determine how a combination of overload of the health system and the imposed security measures influenced the UICC stage of NSCLC in the medium term. Assuming a mean time to diagnosis of 30 days (9), the effects of missed or prolonged diagnosis due to high incidence and security measures were anticipated for spring 2021.
Figure 1 displays the defined investigation periods in relation to the 7-day incidence of SARS-Cov-2 in Leipzig and MV, as well as the ICU beds occupied by SARS-CoV-2 patients in Germany and the imposed curfew periods in Germany. Incidence rates were retrieved from official records of the German central scientific institute of biomedicine Robert-Koch-Institute (RKI). Data on occupied ICU beds were extracted from the German register of ICU capacity run by the RKI and the German Interdisciplinary Association of Intensive and Emergency Care (DIVI).
The investigation periods (IP) were compared to the NSCLC incidences and UICC stages in the corresponding months of the previous year (control periods, CP). Table 1 shows the investigation and control periods.
Table 1
| Study period | IP | CP | Explanation |
|---|---|---|---|
| Period I | May 1st to June 30th, 2020 | May 1st to June 30th, 2019 | Aftermath of imposed security measures, i.e., curfew without significant incidence of COVID-19 |
| Period II | November 1st, 2020, to January 31st, 2021 | November 1st, 2019, to January 31st, 2020 | Imposed security measures, i.e., curfew with high incidence of COVID-19 |
| Period III | February 1st to March 31st, 2021 | February 1st to March 31st, 2020 | Aftermath of imposed security measures, i.e., curfew and high incidence of COVID-19 |
IP, investigation period; CP, control period.
Statistical analysis
UICC tumor stages were calculated according to the 8th edition (10). The influence of pandemic periods on the UICC stage was studied by Mann-Whitney U Test. UICC stages were differentiated into T and N stages. To assess whether a potential impact on T, N, or UICC stage also altered the therapeutic regime, cases were divided into curative intended operable and not curative intended operable. In compliance with German Guidelines for the Prevention, Diagnostic, Therapy, and Follow-Up of Lung Cancer (11), curative-intended surgery was subsumed for cases lower or equivalent to UICC IIIA. Pearson’s correlation was calculated and tested for significance. Analysis was performed using SPSS Version 27 (IBM).
Results
A total of 3,372 patients had their first diagnosis of NSCLC in MV (N=1,774) and Leipzig (N=1,598) from January 1st, 2019, to March 31st, 2021. Due to incomplete or inconclusive data, some cases had to be excluded. Data enrollment is reported according to CONSORT guidelines in Figure 2 (12).
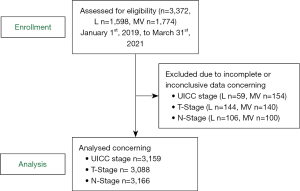
The number of patients diagnosed with NSCLC dropped substantially, especially during period III. This effect was most substantial in Leipzig, where patient numbers decreased by nearly 30 percent in period III. Table 2 displays the development of the number of patients during the COVID-19 periods and its trend in percentage.
Table 2
| Study region | Period I | Period II | Period III | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IP | CP | Trend in % | IP | CP | Trend in % | IP | CP | Trend in % | |||
| MV | 143 | 127 | −11.2 | 197 | 187 | −5.1 | 156 | 134 | −14.1 | ||
| Leipzig | 125 | 130 | +4 | 150 | 122 | −18.6 | 103 | 74 | −28.2 | ||
| In total | 268 | 257 | −4.1 | 347 | 309 | −10.9 | 259 | 208 | −19.7 | ||
IP, investigation period; CP, control period; MV, Mecklenburg-Vorpommern.
Mann-Whitney U test was calculated to determine changes in the distribution of UICC-stage, T- and N-status during the pandemic phases. For all periods, distributions differed between investigation and control groups, Kolmogorov-Smirnov P<0.05. For period III, UICC-stage differed significantly between CP and IP in Leipzig. Moreover, N-status showed statistically significant changes during period III. Table 3 shows the results of Mann-Whitney-U-tests for UICC-stage, T- and N-status for the pandemic periods.
Table 3
| Tumor classification per period and region | Kolmogorov-Smirnov | Mann-Whitney U | ||||
|---|---|---|---|---|---|---|
| Z | P | U | Z | P | ||
| UICC (n=3,159) | ||||||
| Period I | ||||||
| In total (n=525) | 3.505 | 0.000 | 32,878.5 | −0.915 | 0.36 | |
| L (n=255) | 2.171 | 0.001 | 7,602 | −0.907 | 0.364 | |
| MV (n=270) | 2.753 | 0.001 | 8,823.5 | −0.41 | 0.682 | |
| Period II | ||||||
| In total (n=656) | 4.137 | 0.000 | 51,548.5 | −0.867 | 0.386 | |
| L (n=272) | 2.242 | 0.001 | 8,287 | −1.365 | 0.172 | |
| MV (n=384) | 2.986 | 0.001 | 18,353.5 | −0.062 | 0.951 | |
| Period III | ||||||
| In total (n=467) | 3.027 | 0,001 | 24,576.5 | −1.661 | 0.097 | |
| L (n=177) | 1.656 | 0.008 | 3,019.5 | −2.413 | 0.016* | |
| MV (n=290) | 2.558 | 0.001 | 10,265 | −0.267 | 0.789 | |
| T-status (n=3,088) | ||||||
| Period I | ||||||
| In total (n=511) | 3.952 | 0.000 | 32,232.5 | −0.237 | 0.813 | |
| L (n=240) | 3.150 | 0.000 | 6,751 | −0.879 | 0.380 | |
| MV (n=271) | 2.492 | 0.001 | 8,695 | −0.708 | 0.477 | |
| Period II | ||||||
| In total (n=647) | 4.427 | 0.000 | 52,146 | −0.039 | 0.968 | |
| L (n=250) | 3.256 | 0.000 | 7,314 | −0.742 | 0.457 | |
| MV (n=397) | 3.104 | 0.000 | 19,222 | −0.434 | 0.665 | |
| Period III | ||||||
| In total (n=458) | 3.845 | 0.000 | 25,654 | −0.223 | 0.824 | |
| L (n=165) | 2.807 | 0.001 | 3,191 | −0.47 | 0.640 | |
| MV (n=293) | 2.664 | 0.001 | 10,623.5 | −0.075 | 0.945 | |
| N-status (n=3,166) | ||||||
| Period I | ||||||
| In total (n=534) | 3.488 | 0.000 | 33,757.5 | −1.101 | 0.271 | |
| L (n=253) | 2.306 | 0.001 | 7,239.5 | −1.349 | 0.178 | |
| MV (n=281) | 2.552 | 0.001 | 9,744.5 | −0.160 | 0.874 | |
| Period II | ||||||
| In total (n=669) | 4.187 | 0.000 | 53,317.5 | −1.059 | 0.29 | |
| L (n=259) | 2.295 | 0.001 | 7,443.5 | −1.458 | 0.145 | |
| MV (n=410) | 3.489 | 0.000 | 20,767 | −0.213 | 0.832 | |
| Period III | ||||||
| In total (n=402) | 2.484 | 0.001 | 16,059.5 | −2.294 | 0.022* | |
| L (n=170) | 1.906 | 0.001 | 2,964.5 | −1.865 | 0.063 | |
| MV (n=232) | 1.878 | 0.002 | 5,107 | −1.342 | 0.18 | |
*, P<0.05. UICC, Union for International Cancer Control; L, Leipzig; MV, Mecklenburg-Vorpommern.
The drop in patient numbers showed no significant change in T-status distribution. There was a significant difference in UICC status between CP and IP of period III in Leipzig (P=0.016). Effect size according to the Pearson correlation coefficient was low (r=−0.181). The distribution of UICC status during the pandemic phases in Leipzig is shown in Figure 3. There was a substantial increase in UICC status IVB during phase III (P=0.007). Share of UICC status IA was significantly smaller in IP than CP during period III (P=0.049). This effect was the same in period II, with a drop of 10 percent from CP to IP (P=0.012). There was no significant difference between IP and CP in any period when comparing UICC status lower and equivalent to IIIA.
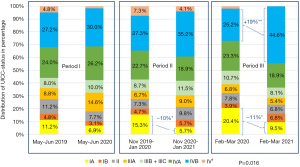
N-status differed significantly between IP and CP of period III (P=0.022). Effect size according to the Pearson correlation coefficient was low (r=−0.114). The change in N-status is shown in Figure 4. There was a significant decrease in N0-status (P=0.04) and an increase in N3-status (P=0.027), while N1- and N2-status remained unaffected (P=0.509 and P=0.57, respectively). During period II share of N1 increased significantly from CP to IP (P=0.046).
A chi-square test was calculated to determine whether there is a significant correlation between pandemic phases and operability. Cases with less or equal UICC status IIIA were rated as curative intended operable. Table 4 shows the results for the chi-square test for each period indicating χ2 and P value. No expected cell frequencies were below 5. The distribution of cases less or equal to UICC status IIIA did not significantly differed between the periods. Thus, no pandemic phase showed a significant difference in curative intended operability.
Table 4
| Study period per region | Chi-square test | |
|---|---|---|
| χ2 | P | |
| Period I | ||
| In total (n=525) | 1.367 | 0.241 |
| L (n=255) | 0.387 | 0.534 |
| MV (n=270) | 0.929 | 0.335 |
| Period II | ||
| In total (n=656) | 0.1 | 0.751 |
| L (n=272) | 0.415 | 0.520 |
| MV (n=384) | 0.69 | 0.406 |
| Period III | ||
| In total (n=467) | 0.996 | 0.318 |
| L (n=177) | 2.085 | 0.149 |
| MV (n=290) | 0.04 | 0.841 |
L, Leipzig; MV, Mecklenburg-Vorpommern.
Discussion
Our findings show a substantial drop in diagnosed NSCLC during all pandemic phases compared to the previous year. This may be due to a missed or later diagnosis. Reasons for late diagnosis during the COVID-19 pandemic may differ individually. Security concerns impact surgical care during pandemics in a distinct matter (13). Patients may avoid consulting doctors for fear of infection or skip regular health screenings. Besides the prolongation of diagnostics during the epidemic, overall changes in daily routines may have significantly impacted risk factors. Tseng et al. showed that smokers who qualified for low-dose computed tomography (LDCT) screening developed adverse habits and increased risky behavior, such as increased cigarette smoking, less physical activity, and gaining more body weight (14). This may influence the incidence of lung cancer in the long run as well. Security concerns, however, also affected the daily routine in hospitals, leading to deferred operations. A Canadian study group showed that while waiting times for lung cancer diagnosis were not prolonged during COVID-19 and met international recommendations (9,15), the wait time for surgery was significantly delayed (16). A large multicenter study including all Veterans Health Admissions patients in the USA found that LDCT screening decreased in the first half of 2020 but rebounded in the second half without an overall annual deficit (17). However, lung cancer diagnoses shrunk by 13 percent (17). This effect might be even more profound in Germany, as structured lung cancer screening programs for high-risk groups such as LDCT screening are not established in Germany. While the reasons for the drop in caseloads may be multifaceted, its implications uniformly anticipate severe consequences for lung cancer care in the future. Missed diagnosis of early-stage diseases surmises more patients with advanced diseases in the future. In the same way, the number of undiagnosed patients that die from lung cancer is expected to be higher. This predicts a relevant impact on patients’ prognosis. Though the overall prognosis has not been studied, one can derive that the decrease in patient numbers likely means that overall survival will be worse.
Symptoms of NSCLC are often unspecific, including dyspnea, cough, sputum, fatigue, or fever, and can mimic a common cold. Patients with respiratory symptoms may have been sent home when testing for SARS-CoV-2 remained negative due to an overload of health systems. Tumor staging may have been prolonged due to excessive demand for pneumologists. However, incidental findings of NSCLC during diagnostic or therapy of COVID-19 are also cogitable.
Yet, the prognostic relevance of diagnostic or therapeutic prolongation seems to be small in early-stage lung cancer, allowing for a postponement of surgery by 3–4 months for stage I indolent lung tumors or part-solid ground glass lung nodules without significant differences in 5-year survival rates (18-20). This is consistent with our results. Though there was a shift to higher stages in UICC status in Leipzig and overall N-Status during the third period, no significant difference was found concerning operability.
A particularly conspicuous aspect is the increase in cases diagnosed in status N3 and UICC IVA, while operability is not significantly influenced. On the one hand, this result contradicts surgeons’ perception that the number of surgeries shrunk during pandemic periods. On the other hand, this outcome indicates that already inoperable stages shifted to higher staged cases. In the case of N3, this is explainable by a shift from T3-4N2 to T3-4N3 according to UICC IIIB to IIIC. The authors acknowledge that operability is discussed controversially, especially concerning UICC IIIA. This is particularly relevant considering the shift from IVA to IVB in period III. Paying attention to the promising results on the role of surgery in oligometastatic NSCLC (21,22), the turn from oligometastatic to multi-metastatic tumor stage influences the assignment of surgery as well and may predict a severe loss of life expectancy.
Notwithstanding, it is very likely that the shift of tumor stages influenced the prognosis. The study period only allows for short-term observation. Future investigations may use our data as a connecting point for studying long-term effects on prognosis.
Regarding health security, it is remarkable that the sole implementation of security measures such as the imposed curfew (period I) had no negative impact on the diagnosis of NSCLC. Significant changes in tumor stages only occurred in the aftermath of high incidence rates and imposed restrictions. Thus, the effect of securitization on NSCLC progress seems negligible during the SARS-CoV-2 pandemic.
This study has several limitations. First, the study results of this retrospective two-center analysis may be challenging to transfer to other settings and are not representative of Germany. Second, due to data availability, study periods are limited to the early phases of the pandemic, and no long-term effects can be derived. This can be an interesting connecting point for future studies. Third, data showed a significant increase in N3 status during period III. This implies a substantial increase in patients not curable on the first diagnosis. However, this effect was no longer significant when comparing operability. The authors acknowledge that UICC state IIIA is considerably heterogeneous and of limited use for the distinction in operability. Fourth, the overload of the health system probably influenced the time from diagnosis to therapy as well, which is substantial for prognosis. This effect has not been measured in our study.
Conclusions
The pandemic spread of SARS-CoV-2 was associated with a decline in the diagnosis of NSCLC in Leipzig and MV. A significant change in UICC stages was seen in Leipzig as well as a shift to a higher N-status in total in the aftermath of increased incidence rates and the imposed security measures. However, no significant change in operability was seen during the investigated pandemic phases.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1091/rc
Data Sharing Statement: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1091/dss
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1091/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-22-1091/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Ethical approval for this retrospective evaluation of archived, anonymized patient data was waived by the Scientific Ethical Committee at the Medical Faculty, Leipzig University. Informed consent from patients was not needed as the data was anonymized.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dolan DP, Lee DN, Polhemus E, et al. Report on lung cancer surgery during COVID-19 pandemic at a high volume US institution. J Thorac Dis 2022;14:2874-9. [Crossref] [PubMed]
- London JW, Fazio-Eynullayeva E, Palchuk MB, et al. Effects of the COVID-19 Pandemic on Cancer-Related Patient Encounters. JCO Clin Cancer Inform 2020;4:657-65. [Crossref] [PubMed]
- Morais S, Antunes L, Rodrigues J, et al. The impact of the coronavirus disease 2019 pandemic on the diagnosis and treatment of cancer in Northern Portugal. Eur J Cancer Prev 2022;31:204-14. [PubMed]
- Ferlay J, Ervik M, Lam F, et al. Global Cancer Observatory: Cancer Today. Lyon, 2020.
- Degeling K, Baxter NN, Emery J, et al. An inverse stage-shift model to estimate the excess mortality and health economic impact of delayed access to cancer services due to the COVID-19 pandemic. Asia Pac J Clin Oncol 2021;17:359-67. [Crossref] [PubMed]
- Martínez-Hernández NJ, Caballero Silva U, Cabañero Sánchez A, et al. Effect of COVID-19 on Thoracic Oncology Surgery in Spain: A Spanish Thoracic Surgery Society (SECT) Survey. Cancers (Basel) 2021;13:2897. [Crossref] [PubMed]
- Pasello G, Menis J, Pilotto S, et al. How the COVID-19 Pandemic Impacted on Integrated Care Pathways for Lung Cancer: The Parallel Experience of a COVID-Spared and a COVID-Dedicated Center. Front Oncol 2021;11:669786. [Crossref] [PubMed]
- Hilzenrat RA, Deen SA, Yee J, et al. Thoracic Surgeon Impressions of the Impact of the COVID-19 Pandemic on Lung Cancer Care-Lessons from the First Wave in Canada. Curr Oncol 2021;28:940-9. [Crossref] [PubMed]
- BTS recommendations to respiratory physicians for organising the care of patients with lung cancer. The Lung Cancer Working Party of the British Thoracic Society Standards of Care Committee. Thorax 1998;53:S1-8. [Crossref] [PubMed]
- Brierley J, Gospodarowicz M, Wittekind C. TNM classification of malignant tumours, 8th edition. Chicester: Wiley-Blackwell, 2016.
- German Cancer Society, German Cancer Aid, Association of the Scientific Medical Societies in Germany. Prevention, diagnosis, therapy and follow-up care of lung cancer. AWMFRegisternummer 020/007OL; 2018.
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomised trials. Lancet 2001;357:1191-4. [Crossref] [PubMed]
- Metelmann IB, Flessa S, Busemann A. Does health securitization affect the role of global surgery? Z Gesundh Wiss 2022;30:925-30. [Crossref] [PubMed]
- Tseng TS, Li M, Kao YH, et al. The Impact of COVID-19 on Risky Behaviors and Health Changes in African-American Smokers Who Are Eligible for LDCT Screening. Front Public Health 2021;9:745925. [Crossref] [PubMed]
- National Health Service England. National Health Service National Cancer Waiting Times Monitoring Dataset Guidance, 2020.
- Kasymjanova G, Anwar A, Cohen V, et al. The Impact of COVID-19 on the Diagnosis and Treatment of Lung Cancer at a Canadian Academic Center: A Retrospective Chart Review. Curr Oncol 2021;28:4247-55. [Crossref] [PubMed]
- Englum BR, Prasad NK, Lake RE, et al. Impact of the COVID-19 pandemic on diagnosis of new cancers: A national multicenter study of the Veterans Affairs Healthcare System. Cancer 2022;128:1048-56. [Crossref] [PubMed]
- Mayne NR, Elser H, Lin BK, et al. The Impact of Extended Delayed Surgery for Indolent Lung Cancer or Part-Solid Ground Glass Nodules. Ann Thorac Surg 2022;113:1827-34. [Crossref] [PubMed]
- Mazzone PJ, Gould MK, Arenberg DA, et al. Management of Lung Nodules and Lung Cancer Screening During the COVID-19 Pandemic: CHEST Expert Panel Report. Radiol Imaging Cancer 2020;2:e204013. [Crossref] [PubMed]
- Mayne NR, Elser HC, Darling AJ, et al. Estimating the Impact of Extended Delay to Surgery for Stage I Non-small-cell Lung Cancer on Survival. Ann Surg 2021;273:850-7. [Crossref] [PubMed]
- Casiraghi M, Bertolaccini L, Sedda G, et al. Lung cancer surgery in oligometastatic patients: outcome and survival. Eur J Cardiothorac Surg 2020;57:1173-80. [Crossref] [PubMed]
- Gomez DR, Tang C, Zhang J, et al. Local Consolidative Therapy Vs. Maintenance Therapy or Observation for Patients With Oligometastatic Non-Small-Cell Lung Cancer: Long-Term Results of a Multi-Institutional, Phase II, Randomized Study. J Clin Oncol 2019;37:1558-65. [Crossref] [PubMed]



