
Effect of different pre-hospital first aid methods on the efficacy and prognosis of acute myocardial infarction with left heart failure: a systematic review and meta-analysis
Highlight box
Key findings
• In this study, the meta-analysis showed that pre-hospital first aid can significantly improve the clinical treatment effect of patients with AMI and left heart failure.
What is known and what is new?
• AMI with acute left heart failure has the characteristics of acute onset and great changes. At this stage, there is no consensus on the method of pre-hospital first aid in clinical practice;
• In this study, we conducted a systematic evaluation and meta-analysis of the 2 pre-hospital first aid methods to determine the efficacy and prognostic impact of first aid, then transport, or first transport and then first aid for AMI with left heart failure.
What is the implication, and what should change now?
• This study provides evidence-based medical data in support of the clinical application and promotion of the pre-hospital first aid method of first aid and then transport.
Introduction
Acute myocardial infarction (AMI) is a serious cardiovascular disease mainly caused by coronary artery occlusion and myocardial ischemia, and it is common in elderly patients with high morbidity and mortality (1-3). Acute stress, such as a burst of anger, bereavement, or strong emotions such as fear or extreme excitement, can lead to a heart attack or sudden death (4). In addition, coronary artery obstruction, high-intensity labor, and overeating may also cause AMI. A high rate of sudden death is associated with untimely effective treatment measures (5-7). A sharp reduction or complete interruption of coronary artery blood supply in patients with AMI leads to severe and long-lasting acute ischemia, which can cause myocardial cell necrosis and abnormal heart function. Acute left heart failure is one of the common complications (8-10). AMI complicated with acute left ventricular failure has a rapid onset and great physiological changes. In order to effectively save the life of the patient, prompt emergency treatment at the hospital is necessary (11,12), therefore, there are higher requirements for pre-hospital first aid. However, there is currently no unified consensus on the methods of pre-hospital first aid in clinical practice. Some studies suggest that first aid and then transportation treatment is more effective than direct transport, but it also carries risks such as prolonged emergency department stays and increased rescue efforts (13,14). On the other hand, study also shown that direct transport can reach the hospital more quickly and can start treatment more quickly, but may also lead to reduced rescue efficiency, more complications, and so on (15). In this paper, we conducted a systematic review and meta-analysis of the 2 pre-hospital first aid methods to determine whether first aid should be implemented before transportation or after transportation by assessing the curative effect and prognostic impact of AMI with left heart failure, in order to find the optimal method of pre-hospital first aid. We present the following article in accordance with the MOOSE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-195/rc).
Methods
Literature search
We searched the databases of PubMed, OVID, Web of Science, Embase, China National Knowledge Infrastructure (CNKI), VIP, and Wanfang to retrieve articles related to pre-hospital first aid for AMI with left heart failure. The formulation of the literature retrieval formula adopted subject words combined with free words. Chinese and English keywords included pre-hospital first aid, out-of-hospital first aid, emergency medical services, AMI, left heart failure, efficacy, and prognosis. The search time was updated from the establishment of the database to 23 November 2022, and the language scope of the searched documents was limited to Chinese and English. The literature retrieval method takes PubMed database retrieval as an example, as shown below:
- #1 “pre-hospital first aid” OR “out-of-hospital first aid” OR “emergency medical services”;
- #2 “acute myocardial infarction” OR “left heart failure”;
- #3 “efficacy” OR “prognosis”;
- #4 #1 AND #2 AND #3.
Literature inclusion and exclusion criteria
Literature inclusion criteria
(I) Cohort research literature published in various databases; (II) the research content is an article related to the efficacy and prognosis of pre-hospital first aid on AMI with left heart failure; (III) in the intervention methods in the literature, the observation group received first aid and then transportation, whereas the control group received transportation and then first aid.
Literature exclusion criteria
(I) The full text cannot be obtained, only the title and abstract of the literature can be found; (II) non-cohort studies such as case reports, reviews, and news; (III) the data in the literature is missing or the main data cannot be extracted (such as standard deviation); (IV) duplicate publications.
Outcome indicators
A total of 7 outcome indicators were included in this paper: (I) clinical effect after pre-hospital emergency treatment; (II) respiratory rate of patients after treatment; (III) heart rate of patients after treatment; (IV) systolic blood pressure (SBP) of patients after treatment; (V) diastolic blood pressure (DBP) of patients after treatment; (VI) survival status of patients after treatment; (VII) incidence of complications after treatment.
Literature quality evaluation and data extraction
According to the established search formula and inclusion and exclusion criteria, 2 researchers independently read the titles and abstracts for preliminary screening, read the full text for re-screening, included articles that met our requirements, and extracted the required data from the included literature. The data to be extracted included baseline data and outcome indicators, the former mainly including the author of the literature, year of publication, sample size, patient age, and so on. The latter comprised the value of 7 outcome indicators. After literature and data extraction, the 2 researchers conducted cross-checking, and if there was any disagreement, a third researcher was invited to arbitrate. The quality evaluation of the included studies was carried out by the Newcastle-Ottawa scale (NOS). The scale has a total of 8 items, including study population selection, comparability, exposure evaluation or result evaluation. The total score is 9 points, and the scores of 1–3, 4–6 and 7–9 are low, medium and high quality, respectively, with high, medium and low risk of bias.
Statistical analysis
All data were analyzed using R 4.0.5 (The R Foundation for Statistical Computing, Vienna, Austria. The risk ratio (RR) coefficient and 95% confidence interval (CI) were used to describe the count data, and the mean difference (MD) and 95% CI were used to describe the measurement data. Data analysis was performed using fixed or random effects models. The heterogeneity test between different studies was represented by I2. When I2>50%, it was considered that there was heterogeneity among studies, and a random effect model is used; otherwise, when I2≤50%, there was no heterogeneity, and a fixed effect model was used. The publication bias of the literature was estimated by funnel plot and Egger’s test, and the results of meta-analysis were considered statistically significant when two-sided P<0.05.
Results
Literature search results
A total of 853 articles were obtained in the preliminary examination, and 721 articles remained after the software had removed duplicate articles. After reading the title and abstract, 613 articles that were obviously inconsistent with the theme of this article were removed, and 95 documents that might meet the theme of this article were obtained. After being included in this article for full-text reading, a further 62 articles without a control group and 17 articles without reliable important data were excluded; a total of 16 papers were finally included (Figure 1).
Basic characteristics and quality evaluation of included literature
A total of 16 documents were included in this study (a total of 732 patients in the observation group and 733 patients in the control group were included). There was no statistical difference in the baseline data of the included patients. Among the included articles, 15 reported the clinical effect after treatment, 8 reported the patient’s respiratory rate and survival status after treatment, 7 reported the patient’s heart rate and SBP and 6 reported the patient’s DBP, and 5 articles reported the incidence of complications in patients. The literature quality evaluation found that 8 articles were rated as low risk of bias and 8 articles were rated as grade moderate risk of bias, and the quality met the requirements (Table 1).
Table 1
| First author | Years | Sample size | Sex ratio (F/M) | Age (years), mean ± SD | NYHA cardiac function class [n] | Outcome indicators* | Literature quality | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Experimental group | Control group | Experimental group | Control group | Experimental group | Control group | Experimental group | Control group | |||||||
| Cui (16) | 2020 | 36 | 36 | 19/17 | 20/16 | 54.60±5.20 | 53.90±5.00 | III [22], IV [14] | III [21], IV [15] | 2, 3, 4, 5, 7 | Low risk of bias | |||
| Wang (17) | 2016 | 100 | 100 | 54/46 | 39/61 | 77.2±2.3 | 76.4±2.5 | III [39], IV [61] | III [40], IV [60] | 1, 2, 3, 4, 5, 6, 7 | Low risk of bias | |||
| Liu (18) | 2017 | 33 | 33 | 18/15 | 19/14 | 70.42±9.65 | 70.15±9.46 | – | – | 1, 2, 6 | Moderate risk of bias | |||
| Xiong (19) | 2021 | 42 | 44 | 23/19 | 23/21 | 67.2±3.2 | 67.2±3.3 | III [23], IV [19] | III [25], IV [19] | 1 | Moderate risk of bias | |||
| Dong (20) | 2020 | 43 | 43 | 28/25 | 29/14 | 68.04±5.16 | 68.53±5.81 | – | – | 1 | Moderate risk of bias | |||
| Qi (21) | 2017 | 50 | 50 | 23/27 | 24/26 | 69.12±3.43 | 69.20±3.21 | III [20], IV [30] | III [21], IV [29] | 1 | Moderate risk of bias | |||
| Wang (2) | 2015 | 40 | 40 | 22/18 | 23/17 | 70.03±6.08 | 70.31±6.92 | III [15], IV [25] | III [16], IV [24] | 1, 2, 3, 4, 5, 7 | Low risk of bias | |||
| Guo (10) | 2018 | 45 | 45 | 24/21 | 26/19 | 64.85±2.36 | 64.56±2.12 | III [18], IV [27] | III [20], IV [25] | 1, 6, 7 | Low risk of bias | |||
| Tan (22) | 2019 | 27 | 27 | 12/15 | 14/13 | 64.37±5.55 | 64.44±5.76 | – | – | 1, 6 | Moderate risk of bias | |||
| Jin (23) | 2019 | 37 | 40 | 26/11 | 28/12 | 63.3±4.2 | 64.1±4.5 | – | – | 1, 2, 3, 4, 5 | Low risk of bias | |||
| Han (24) | 2021 | 32 | 32 | 21/11 | 21/11 | 67.26±5.09 | 67.26±5.09 | – | – | 1, 2, 3, 4, 5, 6 | Low risk of bias | |||
| Li (25) | 2018 | 30 | 30 | 20/10 | 19/11 | 71.24±1.26 | 71.44±1.56 | – | – | 1, 6 | Low risk of bias | |||
| Ye (15) | 2019 | 44 | 40 | 25/19 | 23/17 | 64.18±7.66 | 65.22±7.85 | III [24], IV [20] | III [22], IV [18] | 1, 2, 3, 4, 5, 7 | Moderate risk of bias | |||
| Liu (11) | 2019 | 30 | 30 | 20/10 | 18/12 | 51.45±4.69 | 52.65±5.59 | III [12], IV [18] | III [13], IV [17] | 1, 2, 3, 4, 6 | Low risk of bias | |||
| Zhang (26) | 2021 | 43 | 43 | 25/18 | 23/20 | 69.65±6.84 | 70.58±6.94 | – | – | 1 | Moderate risk of bias | |||
| Chen (27) | 2016 | 42 | 42 | 22/20 | 25/17 | 64.9±NA | 61.9±NA | III [16], IV [26] | III [18], IV [24] | 1, 6 | Moderate risk of bias | |||
*, [1] clinical effect after treatment; [2] respiratory rate; [3] heart rate; [4] systolic blood pressure; [5] diastolic blood pressure; [6] survival status; [7] complications. NYHA cardiac function classification: Class III, the patient has no symptoms at rest, but symptoms appear when their daily activities are less severe, with moderate heart failure; Class IV, patients have symptoms of heart failure or angina during rest, are unable to engage in any physical activity, and have severe heart failure. F, female; M, male; NYHA, New York Heart Association; SD, standard deviation.
Meta-analysis results
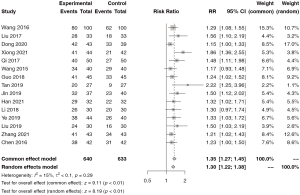
Comparison of clinical effects after treatment
A total of 15 articles contained data on clinical outcomes after treatment. There was no heterogeneity among the studies (I2=15%), so the meta-analysis was carried out by the fixed effect model. The results showed that the clinical effect of pre-hospital first aid first aid and then transportation was significantly better than that of the control group (RR =1.35, 95% CI: 1.27 to 1.45, P<0.01; Figure 2).
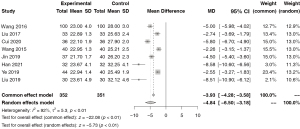
Comparison of respiratory rate after treatment
A total of 8 papers reported data on the respiratory rate of patients after treatment. There was high heterogeneity among the studies (I2=92%), so meta-analysis was carried out by random effect model. The results showed that the respiratory rate of the patients was significantly reduced after the first aid and then transportation (MD =−4.84, 95% CI: −6.50 to −3.18, P<0.01; Figure 3).
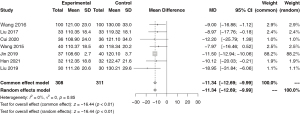
Comparison of heart rate after treatment
A total of 7 papers reported data on heart rate of patients after treatment. There was no heterogeneity among the studies (I2=0%), so the meta-analysis was carried out by the fixed effect model. The results showed that the heart rate of the patients was significantly reduced after the pre-hospital first aid method of first aid and then transportation (MD =−11.34, 95% CI: −12.69 to −9.99, P<0.01; Figure 4).
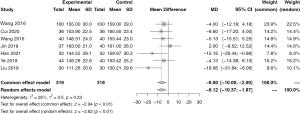
Comparison of SBP after treatment
A total of 7 papers reported data on patients’ SBP after treatment. There was no heterogeneity among the studies (I2=26%), so the meta-analysis was carried out by the fixed effect model. The results showed that the SBP of the patients was significantly reduced after the pre-hospital first aid method of first aid and then transportation (MD =−6.00, 95% CI: −10.00 to −2.00, P<0.01; Figure 5).
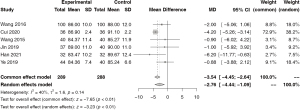
Comparison of DBP after treatment
A total of 6 papers reported data on DBP of patients after treatment. There was no heterogeneity among the studies (I2=40%), so the meta-analysis was carried out by the fixed effect model. The results showed that the DBP of the patients was significantly reduced after the first aid and then transportation (MD =−3.54, 95% CI: −4.45 to −2.64, P<0.01; Figure 6).
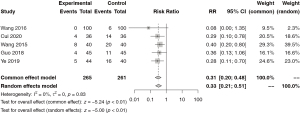
Comparison of survival status after treatment
A total of 8 papers reported data on patient survival after treatment. There was no heterogeneity among the studies (I2=0%), so the meta-analysis was carried out by the fixed effect model. The results showed that the survival status of the patients after the first aid and then transportation was significantly improved (RR =1.29, 95% CI: 1.18 to 1.41, P<0.01; Figure 7).

Comparison of incidence of complications after treatment
A total of 5 papers reported data on the incidence of complications in patients after treatment. There was no heterogeneity among the studies (I2=0%), so the meta-analysis was carried out by the fixed effect model. The results showed that the incidence of complications after treatment in the pre-hospital first aid mode of first aid and then transportation was significantly reduced (RR =0.31, 95% CI: 0.20 to 0.48, P<0.01; Figure 8).
Publication bias
The funnel plot analysis of the outcome indicators with more than 10 articles included in this article shows that although 1 piece of data was outside the funnel, the overall symmetry was still present (Figure 9). The results of Egger’s test showed that there was no publication bias among the included articles (P>0.05).
Discussion
AMI is a critical disease with increasing clinical morbidity, rapid onset, and critical condition, and its long-term prognosis is closely related to infarct heart failure (11,21,28,29). Since patients with left ventricular failure usually deteriorate rapidly into cardiogenic shock, coma, or even direct endangerment of life, timely symptomatic treatment should be administered to the patient to save the patient’s life (17,20). Pre-hospital first aid is an emergency rescue method for critically ill patients such as AMI with left heart failure. The effect of pre-hospital first aid will directly affect the treatment effect and prognosis of patients. Traditionally, patients with sudden AMI complicated with acute left heart failure should be transported to the hospital for treatment as soon as possible. However, if the transfer is implemented first, the supine position of the patient may increase the amount of blood returned to the heart during the transfer process, and because the patient’s condition is unstable and the external environment is in a panic, emotional stress or mood swings can easily affect the patient, which can worsen their condition further (19). At present, there is no global consensus on the method of pre-hospital first aid. First aid is the main method in Europe, transfer is the main method in the United States, and transfer is the main method in China. Therefore, our study used meta-analysis to explore the optimal first aid method.
In this article, we found that first aid and then transportation can significantly improve the clinical outcomes of patients, reducing shortness of breath, heart rate, and SBP and DBP. The reason may be that myocardial cells in patients with AMI combined with acute left heart failure lose function due to ischemia and have insufficient contractility; reperfusion therapy is urgently needed. This treatment has a strong time dependence. The shorter the time of reperfusion during treatment, the better the prognosis of the patient. Therefore, among patients who need pre hospital emergency treatment, if they are suspected of AMI with left heart failure, priority should be given to restoring myocardial perfusion. After the patient's respiratory, heart rate, and blood pressure symptoms have been alleviated, they can be transferred to a qualified medical institution for comprehensive treatment to improve the clinical treatment effect and prognosis of the patient.
The study also has some limitations and shortcomings. Firstly, when searching for documents in this article, we have collected documents and traced references as much as possible, but there may still be omissions. Secondly, the 16 articles included in this article are not randomized controlled studies (RCTs), and the level of research evidence is not as good as RCTs, which will have a certain impact on the conclusions. Finally, the high heterogeneity of individual results in this article (such as respiratory rate comparisons) can also affect the conclusion to a certain extent.
Conclusions
In summary, the pre-hospital first aid method of first aid and then transportation has significant clinical value in the treatment of patients with AMI complicated with left heart failure, which can effectively inhibit the deterioration of the condition, reduce the incidence of complications, and also shorten the time for patients to receive systemic treatment. But because the quality of the included literature is not high, the included literature is retrospective analysis literature, and the number of literature and sample size is limited. Because this conclusion needs to be further included in more high-quality randomized controlled studies to verify.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the MOOSE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-195/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-195/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-195/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lin B, Chen X, Lu C, et al. Loss of exosomal LncRNA HCG15 prevents acute myocardial ischemic injury through the NF-κB/p65 and p38 pathways. Cell Death Dis 2021;12:1007. [Crossref] [PubMed]
- Wang YY, Ju ZQ, Huang XS. Effects of different pre-hospital first aid methods on the treatment and prognosis of acute myocardial infarction complicated with acute left heart failure. Hebei Medicine 2015;21:1487-90.
- Ni X, Rui XW, Wu J, et al. Effect of Problem-Oriented Evidence-Based Nursing on Clinical Recovery and Prognosis in Patients with Arrhythmia after Acute Myocardial Infarction. Iran J Public Health 2022;51:814-20. [Crossref] [PubMed]
- Vaccarino V, Bremner JD. Behavioral, emotional and neurobiological determinants of coronary heart disease risk in women. Neurosci Biobehav Rev 2017;74:297-309. [Crossref] [PubMed]
- Liao S, Apaijai N, Luo Y, et al. Cell death inhibitors protect against brain damage caused by cardiac ischemia/reperfusion injury. Cell Death Discov 2021;7:312. [Crossref] [PubMed]
- Fabin N, Bergami M, Cenko E, et al. The Role of Vasospasm and Microcirculatory Dysfunction in Fluoropyrimidine-Induced Ischemic Heart Disease. J Clin Med 2022;11:1244. [Crossref] [PubMed]
- Chen L, Zhou SY, Zhu W, et al. Highly Sensitive Lanthanide-Doped Nanoparticles-Based Point-of-Care Diagnosis of Human Cardiac Troponin I. Int J Nanomedicine 2022;17:635-46. [Crossref] [PubMed]
- Xu L, Li Q, Yin D, et al. The clinical efficacy of integrated care in combination with vasopressin for cardiogenic shock induced by acute myocardial infarction: A randomized controlled study protocol. Medicine (Baltimore) 2022;101:e28985. [Crossref] [PubMed]
- Li Z, Hui Z, Zheng Y, et al. Efficacy of Phase II Remote Home Rehabilitation in Patients with Acute Myocardial Infarction after Percutaneous Coronary Intervention. Contrast Media Mol Imaging 2022;2022:4634769. [Crossref] [PubMed]
- Guo HM. Effect of different pre-hospital first aid methods on the treatment effect and prognosis of acute myocardial infarction complicated with acute left heart failure. The Medical Forum 2018;22:2772-3.
- Liu L. The effect of treatment first and transport later in the prehospital first aid of acute myocardial infarction with acute left heart failure and its significance on prognosis. The Medical Forum 2019;23:926-7.
- Gao N, Xu Y, Tu L, et al. Deep Learning-Based Emergency Care Process Reengineering of Interventional Data for Patients with Emergency Time-Series Events of Myocardial Infarction. J Healthc Eng 2022;2022:7339930. [Crossref] [PubMed]
- Wu MY, Li CJ, Hou YT, et al. Analysis of emergency air medical services over 9 years in the Penghu archipelago of Taiwan. Ci Ji Yi Xue Za Zhi 2020;32:82-7. [PubMed]
- Wu Y, Yang Y, Guo X, et al. Effect of pre-hospital early intervention combined with an in-hospital emergency model in the emergency care of patients with acute stroke. Am J Transl Res 2022;14:672-8. [PubMed]
- Ye Y. The first aid effect of different pre-hospital first aid methods on acute myocardial infarction complicated with acute left heart failure. Shanghai Medical & Pharmaceutical Journal 2019;(6): 29-30+34.
- Cui X. Influence of Different Pre-hospital First Aid Methods on the Treatment and Prognosis of Acute Myocardial Infarction Complicated with Acute Left Heart Failure. Guide of China Medicine 2020;109-10.
- Wang F, Zhang M. Effect and Prognosis of Different Patterns of Pre-hospital Emergency on Patients with Acute Myocardial Infarction Complicated with Acute Left Ventricular Failure. Medical Recapitulate 2016;22:827-30.
- Liu K. Effect of Different Pre Hospital Care Methods on the Prognosis and Prognosis of Acute Myocardial Infarction Complicated with Acute Left Heart Failure. Modern Diagnosis and Treatment 2017;28:1379-81.
- Xiong Z. Exploration on the rescue effect of different pre-hospital emergency methods for acute myocardial infarction complicated with acute left heart failure and their effect on the prognosis. Chinese Community Doctors 2021;70-1.
- Dong JC, Zhang YM, Wang ZX, et al. Effects of different pre-hospital emergency approaches on the curative effects and prognosis of patients with acute myocardial infarction complicated by acute left heart failure. Hebei Medical Journal 2020;42:554-7.
- Qi XY. Research on the effect and prognosis of different pre-hospital first aid methods on acute myocardial infarction complicated with acute left heart failure. World Latest Medicine Information 2017;40.
- Tan Y. Comparative analysis of the treatment effect and prognosis of two pre-hospital first aid methods on acute myocardial infarction complicated with acute left heart failure. Chinese Community Doctors 2019;64.
- Jin ZJ. Observing the effects of different pre-hospital first aid methods on the treatment and prognosis of acute myocardial infarction complicated with acute left heart failure. Prevention and Treatment of Cardiovascular Disease 2019;42-4.
- Han Y. Effects of Two Different Pre-hospital First Aid Modes on the First Aid Effect and Prognosis of Acute Myocardial Infarction Complicated with Acute Left Heart Failure. Chinese Journal of Modern Drug Application 2021;45-7.
- Li N. Research on the effect and prognosis of different pre-hospital first aid methods on acute myocardial infarction complicated with acute left heart failure. Health Literature 2018;130.
- Zhang L. Effects of different pre-hospital emergency treatment programs on the efficacy and prognosis in patients with acute myocardial infarction and heart failure. Medical Journal of Liaoning 2021;46-8.
- Chen Y. Clinical effect observation of different pre-hospital emergency way in the treatment of acute myocardial infarction patients complicated with acute left heart failure. Clinical Research and Practice 2016;1:84+86.
- Yu H, Wang X, Deng X, et al. Correlation between Plasma Macrophage Migration Inhibitory Factor Levels and Long-Term Prognosis in Patients with Acute Myocardial Infarction Complicated with Diabetes. Mediators Inflamm 2019;2019:8276180. [Crossref] [PubMed]
- Zhang Y, Chen G, Huang D, et al. Clinical Nursing Pathway Improves Therapeutic Efficacy and Quality of Life of Elderly Patients with Acute Myocardial Infarction. Comput Math Methods Med 2022;2022:3484385. [Crossref] [PubMed]
(English Language Editor: J. Jones)




