
Global, regional, and national time trends in disability-adjusted life years, mortality, and variable risk factors of non-rheumatic calcified aortic valve disease, 1990–2019: an age-period-cohort analysis of the Global Burden of Disease 2019 study
Highlight box
Key findings
• Totally, 122 countries and territories worldwide showed increasing trends in mortality or stagnant declines.
• Over the past 30 years, adverse period and cohort effects have been discovered in many countries and regions with different SDI levels, especially lower levels.
What is known?
• CAVD has resulted in a high burden of disease for people worldwide.
What is new?
• Health disparities between regions are expanding and could lead to a heavy burden of disease in the future.
What is the implication, and what should change now?
• Lower SDI regions may need to strengthen the prevention and control of the primary variable risk factors “high sodium diet”, “high systolic blood pressure”, and “lead exposure”, to reduce the burden of disease.
• Health authorities and policy makers must consider improving the allocation of resources, increasing access to health care resources, controlling variable risk factors, and urgently improving efforts to curb growth of the disease burden.
Introduction
Non-rheumatic heart valve disease (NRVD) is a common and treatable cardiovascular disease; however, it can lead to very high morbidity and mortality rates, and requires considerable health resources (1). Calcific aortic valve disease (CAVD) is the fastest-growing type of NRVD in terms of mortality and disability-adjusted life years (DALYs) (2). During the 30 years from 1990 to 2019, there was a significant increase in the global population from 5.3 [95% uncertainty interval (UI): 5.2–5.5] to 7.7 (95% UI: 7.5–8.0) billion, an increase of 44.6% (2,3). During the same period, global CAVD deaths increased from 12.1 (95% UI: 11.4–12.6) to 18.6 (95% UI: 17.1–19.7) million, an increase of 53.7% (2,4), and CAVD-based deaths increased from 53,300 (95% UI: 47,760–59,730) to 126,830 (95% UI: 105,600–1413,900), an increase of 138% (2). Thus, the CAVD disease burden (number of deaths) is growing 3 and 2.6 times faster than the population and cardiovascular disease burden (number of deaths), respectively. Although the trend and extent of the disease burden differ greatly from region to region and country to country (1,5,6), CAVD has undoubtedly poses a major challenge for human health in the future.
Studies have reported the disease burden of NRVD and proposed that CAVD is an important cause of disease burden in older people, which is consistent with the findings of published analyses (1,7). However, these analyses have not distinguished between the relative contributions of period, age, and cohort to the impact of mortality. Moreover, the disease characteristics and patient overall survival (OS) rates of the main subtypes, degenerative mitral valve disease (DMVD) and CAVD, are very different (1,4,6); thus, further analysis of CAVD is needed. There is also a lack of reliable evidence on changing trends in the main variable risk factors of CAVD in different countries and regions, which is essential to propose effective prevention and treatment strategies. To obtain relevant information for tracking the epidemic trend of disease and determining the priority directions of medical resource investment, in-depth analysis of the mortality rates of these diseases and time trends of DALYs in all countries and regions is needed, as is identifying the changing trends of risk factors. In analysis of the time trends of disease, time variables are often used as a substitute for causal factors that change over time. In the case of patients with CAVD, the risk of death can be categorized according to period, age, and birth cohort effects (8,9). The mortality risks in these patients not only differ depending on biological age (age effect) but may also vary between birth cohorts owing to the presence of economic and social developmental factors and new diagnostic and therapeutic methods. Thus, analysis of DALY and mortality trends, particularly focusing on their relationship with age, period, and cohort effects, can help to identify the successes and shortcomings of current health care systems and clarify where improvements are needed (8,9).
As far as we know, this is the first study to utilize the 2019 Global Burden of Disease (GBD) data and employ an age-period-cohort (APC) model to investigate trends in CAVD mortality, DALY, and key variable risk factors from 1990 to 2019 in 204 countries and territories. This manuscript was produced as part of the GBD Collaborator Network and in accordance with the GBD Protocols (Contact ID: 0034o00001nHH4NAAW). We present the following article in accordance with the STROBE reporting checklist (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-480/rc).
Methods
Data and definitions
The Institutional Review Committee at the University of Washington approved the GBD study’s use of de-identified data and waived the requirement for informed consent. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The GBD 2019 offers the latest descriptive epidemiological data for 369 diseases and illnesses in 204 countries and territories over the 30 years between 1990 and 2019 (6,10). Each event (morbidity, mortality, and health loss) is attributed to some unique and mutually exclusive root cause (including all types of diseases and injuries) (10). The GBD network uses standardized tools in the Bayesian framework to generate disease estimates using all existing data across age, time, and geographic region, and across different health causes and domains. This approach enables information to be gathered from available data to estimate the burden of disease in countries and regions where no primary data sources are available, allowing estimation of the global disease burden for all countries and regions.
The analysis applied the socio-demographic index (SDI) in every country and region, which is a composite indicator describing the per capita income, average duration of education, and fertility rate among women below 25 years of age (6). The SDI ranges between 0 and 1, where higher values indicate higher socioeconomic levels. Based on SDI values in 2019, all countries and regions were divided into 5 categories according to SDI levels, from highest to lowest. Indicators of CAVD deaths, DALYs lost, and risk factors in this study were obtained directly from the GBD database. The reliability of the data has been demonstrated in previous studies (1,4,5).
Analysis of overall time trends of mortality and DALYs in patients with CAVD
The time trends of mortality in this study were assessed using age-standardized mortality rates, and relative changes in the percentage of mortality over the 30 years between 1990 and 2019 were determined. Age-standardized mortality rates were estimated using global age-standardized population data derived from the GBD 2019 (10). The mortality population was categorized into 5 age groups (0–49, 50–59, 60–69, 70–79, and 80+ years) and the proportion of mortality was calculated in every age group. Time trends of DALYs in this study were evaluated using age-standardized DALYs and the relative change percentage of DALYs between 1990 and 2019. Detailed methods for calculating mortality and DALYs are accessible in available publications (3,11).
Analysis with the APC model
The APC model was used in this study to examine prospective trends in mortality and DALYs by birth cohort, period, and age (12). Using conventional epidemiological methods, it is difficult to determine the contributions made to disease trends by age-related biological factors, social factors, and technology (13). This approach has been used in epidemiological analyses of some chronic diseases (e.g., cardiovascular diseases and tumors) (14,15). Typically, the APC model estimates the additive effects of age, period, and birth cohort by fitting a log-linear Poisson model using the Lexis plot of observed rates. Given the exact linearity of the connection between age, period, and cohort (birth cohort equals period minus age), the so-called identification issue (12,13) cannot be solved statistically to evaluate their independent effects. Here, this issue could be circumvented by developing estimable APC variables and functions without setting unnecessary restrictions on model design variables (12). The APC model was constructed using R programming language (R Foundation for Statistical Computing, Vienna, Austria); the precise methodology and details have been presented in earlier studies (3,16).
In this study, input data of the APC model were population data and mortality and estimated DALY values for patients with CAVD in each country/region during 1990–2019. In a general APC model, the period and age intervals should be equal, but in this study, the GBD data were generated in an unequal interval data format (5-year age groups using annual data). Hence, the population, mortality, and DALY data in this study were divided into consecutive 5-year periods from 1990 to 2019 {1990–1994 [1992], 1995–1999 [1997], ..., 2015–2019 [2017]}, with consecutive 5-year age intervals of 50–54, 55–59, ..., 85–85 years, and 85 years and older. The sample included 13 consecutive groups, such as those born between 1903 and 1907 (median, 1905) to those born between 1963 and 1967 (median, 1965), with those born in 1948 to 1952 (median, 1950) birth cohorts regarded as a reference group. The fitted APC model calculated the overall time trends of mortality and DALYs after combining age, period, and cohort effects, which are presented using net drift (annual percentage change obtained after accounting for the above effects) (16). The net drift was determined using the combination of a trend component attributed to calendar time and a trend component attributed to the continuous cohort (16). To reflect the change trend of birth cohort effects, the annual percentage change in age-specific mortality was used in the APC model to calculate the time trend of mortality within each age group (i.e., local drift of mortality, percentage each year). The ratio of age-specific rates throughout every period (cohort) to the reference period (cohort) was used to calculate relative risk (16). The complete value of net drift is contained in both period (cohort) ratio curves. The reference period (cohort) was selected at random and therefore has no bearing on how the results should be interpreted.
The Wald chi-square test was used to determine whether the trend in annual percentage change was significant. We conducted two-way statistical tests, and values with P<0.05 were deemed significant. R software version 3.6.3 was used to perform analysis of the collected data (17).
Risk factor analysis
For the 3 main variable risk factors of CAVD (high sodium diet, high systolic blood pressure, and lead exposure) reported in the GBD 2019 study (18), the change trend over the past 30 years was depicted in terms of sex and SDI levels, respectively; measurement indicators were age-standardized DALYs and age-standardized mortality rates. Data were directly acquired from the GBD database.
Results
Leading causes of global mortality and DALYs in NRVD, 1990–2019
Globally in 2019, the estimated number of deaths from NRVD was 164,000 (95% UI: 140,000–180,000; Figure 1A). Among these, CAVD accounted for more than 77% (127,000; 95% UI: 106,000−141,000) of deaths. Globally during 1990–2019, the proportion of CAVD-related deaths relative to all causes of NRVD mortality in all age groups increased from 68.4% to 77.3%, with the largest relative decrease in high-middle-SDI regions (Figure 1B). The variation in DALYs was similar to that of mortality (Figure 1C,1D).

Global and regional trends of CAVD patient deaths and DALYs lost from 1990 to 2019
Table 1 and Figure 2 show the population, total deaths, age-standardized mortality, all-age mortality, and net mortality drift. In the past 30 years, the global population increased significantly by 44.6%, from 5.3 (95% UI: 5.2–5.5) to 7.7 (95% UI: 7.5–8.0) billion. In contrast, CAVD deaths increased from 53,300 (95% UI: 47,760–59,730) to 126,830 (95% UI: 105,600–1,413,900), an increase of 138%, more than 3 times the rate of population growth during the same period. In 2019, global age-standardized mortality rates ranged from 3.35 (95% UI: 2.75–3.74) per 100,000 in high-SDI regions to 0.7 (95% UI: 0.57–0.84) in low- and medium-SDI regions. However, from 1990 to 2019, the net mortality drift in the whole population ranged from −2.1% [95% confidence interval (CI): −2.39% to −1.82%] per year in high-SDI regions to 0.05% (95% CI: −0.13% to 0.23%) in low- and medium-SDI regions. Therefore, regions with higher SDI levels had higher age-standardized mortality rates overall, but most showed a decreasing trend. Regions with lower SDI levels showed no significant improvement or even an increasing trend for these indicators.
Table 1
| Indicators | Global | High SDI | High-middle SDI | Middle SDI | Low-middle SDI | Low SDI | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2019 | 1990 | 2019 | 1990 | 2019 | 1990 | 2019 | 1990 | 2019 | 1990 | 2019 | ||||||
| Population | |||||||||||||||||
| Number (×106) | 5,350 (5,239, 5,460) |
7,737 (7,483, 7,993) |
822 | 1,013 | 1,150 | 1,430 | 1,717 | 2,397 | 1,130 | 1,764 | 528 | 1,128 | |||||
| Percentage of global | 100.0 | 100.0 | 15.4 | 13.1 | 21.5 | 18.5 | 32.1 | 39.6 | 21.1 | 22.8 | 9.9 | 14.6 | |||||
| Deaths | |||||||||||||||||
| Number* (×103) | 53.30 (47.76, 59.73) |
126.83 (105.60, 141.39) |
36.02 (32.13, 39.86) |
80.21 (64.30, 90.10) |
8.36 (7.42, 9.21) |
24.44 (20.86, 27.26) |
4.27 (3.50, 5.17) |
10.48 (9.43, 11.74) |
3.12 (2.10, 4.20) |
8.17 (6.63, 9.99) |
1.50 (0.88, 2.20) |
3.46 (2.56, 4.39) |
|||||
| Percentage of global | 100.00 | 100.00 | 67.57 | 63.24 | 15.68 | 19.27 | 8.01 | 8.26 | 5.85 | 6.44 | 2.82 | 2.73 | |||||
| Percent change of deaths 1990–2019 (×100%) | 1.38 (1.13, 1.59) | 1.23 (0.97, 1.40) | 1.92 (1.57, 2.26) | 1.45 (1.10, 2.05) | 1.62 (1.16, 2.38) | 1.3 (0.81, 2.16) | |||||||||||
| All-age mortality rate | |||||||||||||||||
| Rate per 100,000 | 1.00 (0.89, 1.12) | 1.64 (1.36, 1.83) | 4.38 (3.91, 4.85) |
7.92 (6.35, 8.89) |
0.73 (0.65, 0.80) |
1.71 (1.46, 1.91) |
0.25 (0.20, 0.30) |
0.44 (0.39, 0.49) |
0.28 (0.19, 0.37) |
0.46 (0.38, 0.57) |
0.28 (0.17, 0.42) |
0.31 (0.23, 0.39) |
|||||
| Percent change of rate 1990–2019 (×100%) | 0.65 (0.48, 0.79) | 0.81 (0.60, 0.95) | 1.35 (1.06, 1.62) | 0.76 (0.50, 1.18) | 0.68 (0.38, 1.16) | 0.08 (−0.15, 0.48) | |||||||||||
| Age-standardized mortality rate | |||||||||||||||||
| Rate per 100,000 | 1.75 (1.55, 1.96) |
1.76 (1.45, 1.97) |
3.46 (3.06, 3.84) |
3.35 (2.75, 3.74) |
0.93 (0.81, 1.04) |
1.28 (1.08, 1.43) |
0.47 (0.39, 0.57) |
0.48 (0.43, 0.53) |
0.65 (0.44, 0.85) |
0.70 (0.57, 0.84) |
0.77 (0.47, 1.09) |
0.80 (0.61, 0.99) |
|||||
| Percent change of rate 1990–2019 (×100%) | 0.00 (−0.09, 0.08) | −0.03 (−0.12, 0.03) | 0.37 (0.21, 0.54) | 0.01 (−0.13, 0.25) | 0.07 (−0.10, 0.37) | 0.04 (−0.18, 0.39) | |||||||||||
| APC model estimates | |||||||||||||||||
| Net drift of mortality (% per year) |
−1.15 (−1.34, −0.95) | −2.10 (−2.39, −1.82) | −0.60 (−0.76, −0.45) | −0.39 (−0.53, −0.24) | 0.05 (−0.13, 0.23) | −0.27 (−0.51, −0.02) | |||||||||||
| DALYs | |||||||||||||||||
| Number (×103) | 975.89 (872.01, 1,109.79) | 1,837.75 (1,637.02, 2,031.85) | 553.75 (508.56, 609.84) | 913.67 (778.95, 1,005.2) | 178.05 (162.77, 197.28) | 395.65 (353.62, 437.85) | 121 (98.91, 146.12) | 251.02 (227.01, 281.66) | 81.11 (53.2, 111.59) | 187.23 (149.87, 235.31) | 41.39 (22.47, 63.11) | 89.08 (62.68, 119.76) | |||||
| Percentage of global | 100.00 | 100.00 | 56.74 | 49.72 | 18.25 | 21.53 | 12.40 | 13.66 | 8.31 | 10.19 | 4.24 | 4.85 | |||||
| Percent change of DALYs 1990–2019 (×100%) | 0.88 (0.72, 1.07) | 0.65 (0.50, 0.77) | 1.22 (0.96, 1.47) | 1.07 (0.74, 1.61) | 1.31 (0.90, 2.01) | 1.15 (0.68, 1.99) | |||||||||||
| All-age DALYs rate | |||||||||||||||||
| Rate per 100,000 | 18.24 (16.30, 20.74) |
23.75 (21.16, 26.26) |
67.37 (61.87, 74.19) |
90.16 (76.87, 99.19) |
15.48 (14.15, 17.15) |
27.66 (24.72, 30.61) |
7.05 (5.76, 8.51) |
10.47 (9.47, 11.75) |
7.18 (4.71, 9.88) |
10.61 (8.50, 13.34) |
7.84 (4.26, 11.95) |
7.89 (5.55, 10.61) |
|||||
| Percent change of rate 1990–2019 (×100%) | 0.30 (0.19, 0.43) | 0.34 (0.22, 0.44) | 0.79 (0.58, 0.99) | 0.49 (0.25, 0.87) | 0.48 (0.22, 0.93) | 0.01 (−0.22, 0.40) | |||||||||||
| Age-standardized DALYs rate | |||||||||||||||||
| Rate per 100,000 | 26.85 (24.07, 30.31) |
23.90 (21.10, 26.55) |
52.88 (48.59, 58.27) |
42.88 (37.50, 47.00) |
17.25 (15.73, 19.19) |
20.21 (18.01, 22.35) |
10.48 (8.62, 12.68) |
10.18 (9.21, 11.40) |
12.97 (8.69, 17.57) |
13.56 (10.90, 16.84) |
16.14 (9.28, 23.73) |
15.80 (11.57, 20.29) |
|||||
| Percent change of rate 1990–2019 (×100%) | −0.11 (−0.18, −0.03) | −0.19 (−0.25, −0.14) | 0.17 (0.03, 0.29) | −0.03 (−0.18, 0.21) | 0.05 (−0.13, 0.34) | −0.02 (−0.23, 0.34) | |||||||||||
| APC model estimates | |||||||||||||||||
| Net drift of DALYs (% per year) |
−1.01 (−1.11, −0.91) | −1.94 (−2.08, −1.80) | −0.43 (−0.49, −0.36) | −0.33 (−0.37, −0.29) | 0.07 (0.00, 0.13) | −0.27 (−0.31, −0.22) | |||||||||||
*, parentheses for all GBD health estimate indicate 95% UIs. All-age mortality = crude mortality rate. Age-standardized mortality rate and DALY rate is computed using direct standardization with global standard population in the GBD 2019. Parentheses for all GBD health estimates indicate 95% UIs; parentheses for net drift indicate 95% CIs. CAVD, calcific aortic valve disease; DALYs, disability-adjusted life years; SDI, socio-demographic index; APC, age-population-cohort; GBD, Global Burden of Disease; UI, uncertainty interval; CI, confidence interval.
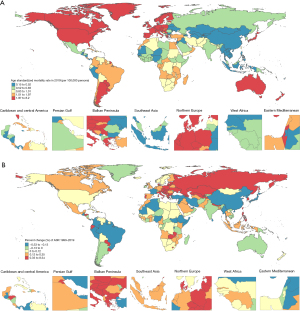
Table 1 and Figure S1 show the age-standardized rates and net drift of DALYs. Similar to mortality changes, in 2019, the global age-standardized DALY rates ranged from 42.88 (37.50, 47.00) per 100,000 in high-SDI regions to 13.56 (10.90, 16.84) in low- and medium-SDI regions. In contrast, the net drift of DALYs in the whole population ranged from −1.94% (95% CI: −2.08% to −1.80%) per year in high-SDI regions to 0.07% (95% CI: 0.00% to 0.13%) in low- and medium-SDI regions. In particular, the net drift of DALYs was most unfavorable for the male population in low- and medium-SDI regions, reaching 0.11% (95% CI: 0.03% to 0.18%). The change trend was essentially the same as that for mortality.
State-level change trends in CAVD patient deaths and DALYs lost from 1990 to 2019
In the 204 countries and territories worldwide, 99 showed a minimum of 50 deaths in 2019, among which the United States (deaths 25,000; 95% UI: 20,000–28,000), Germany (13,000; 95% UI: 11,000–15,000), Japan (13,000; 95% UI: 9,000–16,000), France (80 million; 95% UI: 6,000–9,000), and India (7,000; 95% UI: 5,000–9,000) were the 5 leading countries and territories, accounting for 51.9% of global deaths. Worldwide, 122 countries and territories showed increasing trends in mortality (net drift ≥0.0%) or stagnant declines (≥−0.5%), with 28 countries and territories showing significant upward trends in mortality (net drift ≥1.0% per year). An annual net drift increase of 1% indicated that the mortality rate in these countries and regions would increase by 10%, 18%, and 26% in the next 10, 20, and 30 years, respectively. Poland (6.85%; 95% CI: 5.75% to 7.96%), Estonia (6.02%; 95% CI: 0.93% to 11.36%), Georgia (5.91%; 95% CI: 1.68% to 10.32%), the Czech Republic (5.84%; 95% CI: 4.04% to 7.67%), and Slovakia (5.51%; 95% CI: 3.1% to 7.98%) had the fastest increases.
In terms of DALYs, the largest losses in 2019 were in the United States (288,000; 251,000–318,000), Germany (149,000; 129,000–168,000), India (149,000; 109,000–199,000), Japan (130,000; 99,000–153,000), and France (81,000; 67,000–91,000). In total, 130 countries and territories showed an upward or stagnant downward trend in DALYs lost, with 32 countries and territories showing a clear upward trend. Poland (6.56%; 95% CI: 6.26% to 6.87%), Estonia (6.29%; 95% CI: 5.51% to 7.07%), the Czech Republic (6.06%; 95% CI: 5.78% to 6.35%), Georgia (5.92%; 95% CI: 5.27% to 6.58%), and Slovakia (5.63%; 95% CI: 5.25% to 6.02%) had the fastest increase. The overall trend was the same as the mortality rate.
Overall, these results showed that most countries and regions with higher SDI levels generally have higher mortality and more DALYs lost but have shown a declining trend in recent years. Most countries and regions with lower SDI levels had relatively low mortality and fewer DALYs lost, but the burden of disease had not improved significantly over the past 30 years and had not shown an increasing trend. The distribution and changes in age-standardized mortality and DALYs in the 204 countries and territories with different SDI levels are shown in Figure 3 and Figure S2, respectively.

Time trends in the distribution of deaths and DALYs lost among patients with CAVD by different age groups
Figure 4 shows time trends in the age distribution of deaths in overall patients with CAVD, which is an indirect marker of patient survival. In the past 30 years, the number of CAVD deaths has shown a gradual shift globally toward older age groups (70+ years). There has been a shift in the age distribution of CAVD deaths toward older populations in high-SDI regions, except for Saudi Arabia, the United Arab Emirates, and Qatar, where mortality rates among people aged less than 60 years have remained constant or are increasing. However, the change was relatively insignificant in low-SDI countries and regions. It is important to note that in medium-SDI, low- and medium-SDI, and low-SDI countries and regions, patients under 70 years of age still accounted for approximately half of deaths, which may lead to future mortality increases in these countries and regions. DALY losses showed a similar trend (Figure S3).

Effects of period, age, and cohort factors on mortality and DALYs lost
Figure 5 shows the effects on mortality of local drift and age effects (described as longitudinal age curves representing age-related mortality changes), period effects (described as relative mortality risks for different periods, which can be used to track mortality trends over varying periods), and cohort effects (described as relative mortality risks for cohorts, which can be used to track mortality changes in varying birth cohorts) on CAVD mortality rates estimated using the APC model for the whole population and both male and female cohorts, for countries and regions at global and 5-category SDI levels.

On a global scale, CAVD mortality rates showed a downward trend in all age groups except for the group aged 85+ years. In particular, women aged 65–69 years in high-SDI areas experienced the largest decline (−2.98% per year; 95% CI: −3.27% to −2.68%), indicating that the overall mortality rate decreased by more than 50% in the past 30 years. However, in low-SDI regions, the largest reduction was only −0.497% (95% CI: −0.936% to −0.055%) among people aged 50–54 years, a stagnant decline demonstrating no improvement in mortality across all age groups in countries and regions with low SDI levels. This suggests a large difference between higher- and lower-SDI regions. Regardless of SDI level, mortality improvements in older age groups (80+ years) were very limited and even tended to increase.
Overall, a similar pattern of age effects was found in countries and regions at different SDI levels, with mortality risk increasing with age, and reaching the fastest rate of increase after age 80 years. Overall mortality was higher in all age groups in high-SDI and medium-high-SDI countries and regions compared with other countries and regions. No significant sex differences were seen in the age effects for countries and regions at all SDI levels.
The period effect differs in countries and regions with different SDI levels. In terms of global trends, mortality has gradually declined over time, but there has been little improvement in mortality since 2007. For countries and regions with lower SDI, the period effect has remained almost constant over the last 30 years, suggesting that mortality has no improvement. The high-SDI countries and regions showed the most significant period of risk reduction before 2007 and remained almost unchanged thereafter. In contrast, countries and regions with medium, medium-low, and low SDI even showed a worsening trend in the last 10 years.
Globally, the risk of death in successively younger birth cohorts also tends to vary between countries and regions at different SDI levels. Similar to the period effect, the risk of death across the world decreases gradually with younger birth cohorts, particularly the high-SDI countries and regions. However, there was no significant improvement in medium-low- and low-SDI countries and regions. The effects of period, age, and cohort factors on the trends in DALY and local drift changes were essentially the same as the above trends, see Figure S4 for details.
APC effects in representative countries and regions
To better describe the main trends of CAVD mortality and DALYs influenced by APC across the globe, a few representative countries and regions were selected among countries and regions with 5 different SDI levels. Figure 6 shows the age distribution of the CAVD mortality population and the net drift and APC effects of mortality in 7 representative countries (the United States, Italy, China, Brazil, South Africa, India, and Pakistan). The main trends of DALYs in these countries are shown in Figure S5. The United States is a typical representative country with a high SDI, with a shift in the CAVD mortality population toward the older (80+ years) age group, a trend that is particularly evident in the female cohort. The age-related risk of death after 70 years of age increased rapidly, but overall showed a favorable period and birth cohort trend. Italy stands out for its significant mortality transfer trends, with less than 10% of its mortality population under age 70 years in 2019, a 71.4% decline compared with 1990 (35%). Overall, the results show a favorable period and birth cohort trend. China has a huge population, and the distribution of deaths has shifted relatively slowly toward older age groups over the past 30 years, with 38.5% of the population aged 70 years or older dying in 2019, and deaths among those aged under 70 years falling by 15.1% relative to 1990. However, the overall mortality rate in China was lower, and the period and cohort risks showed a decreasing trend. Similarly, Brazil and South Africa showed a relatively slow shift in the distribution of deaths toward older age groups, with a gradual decline in period and cohort risks at the same time. In India, there was a small upward trend in mortality in the young to middle-aged cohort (aged 30–60 years), but a slow shift in the overall mortality population toward older ages (70+ years). No significant improvement was seen in concurrent period and cohort risks. Pakistan is one of the few countries where the distribution of deaths has shifted toward those less than 70 years of age, and period and cohort risks have shown a worsening trend. APC analysis (net drift) for all 204 countries and regions (with mortality and DALYs) is visualized in the tables (online: https://cdn.amegroups.cn/static/public/jtd-23-480-1.docx).

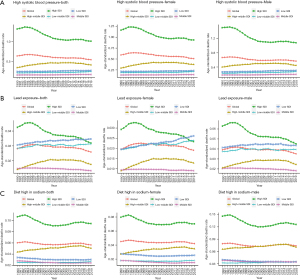
Analysis of variable risk factors
Figure 7 and Figure S6 show the change trends in the main variable risk factors of a high sodium diet, high systolic blood pressure, and lead exposure for CAVD mortality and DALY rates in the global and 5 SDI level regions (in the whole population and in men and women) from 1990 to 2019 (4,18). Mortality and DALY rates were more affected by these 3 risk factors in high-SDI areas than in areas with other SDI levels and the risk tended to decrease in all areas. This may partly explain the relatively high but decreasing trend in mortality rates in high-SDI areas. Risk factors of a high sodium diet and high systolic blood pressure in medium-low- and low-SDI regions showed almost no improvement whereas lead exposure showed an increasing trend.
Discussion
In this study, increases in CAVD deaths and DALYs far exceeded the growth rate of the global population, presenting huge challenges globally. Consistent with previous GBD publications and similar investigations, our study indicated that older populations worldwide are bearing an increasing burden of disease (1,4,18). We also noted that despite achievements in disease prevention and control over the past 3 decades, the health disparities regarding CAVD are widening globally and will likely increase the global disease burden. Analysis of GBD mortality and DALY data showed that countries and regions with higher SDI levels currently have higher age-standardized DALYs and age-standardized mortality rates, but most showed a decreasing trend. Countries and regions with lower SDI levels, particularly for men, showed no significant improvement or an increasing trend in these indicators. Furthermore, the analysis revealed unfavorable cohort and period effects in several countries and regions with different SDI levels over the last 30 years, especially in countries and regions with lower SDI levels. Expectations regarding mortality, increased DALYs, and shifts in the distribution of the mortality population in some countries and regions were not consistent with socioeconomic status at national level (e.g., Saudi Arabia, Qatar, and the United Arab Emirates), assuming that changes in efficacy of the health care system for this group are closely related to SDI. The above phenomenon raises questions as to whether health care is adequate for patients with CAVD in all age groups. Also, the main variable risk factors of CAVD tended to decrease only in countries and regions with high SDI and showed almost no change or even an increasing trend in countries and regions with low SDI levels, suggesting that countries and regions with lower SDI may need to strengthen the prevention and control of these factors to reduce the disease burden.
This was the first time that an APC model has been used to examine time trends in CAVD mortality and DALYs at global level, which enabled comparisons between 204 countries and territories. In comparison with earlier GBD studies (1,4,18), this study presented an in-depth analysis of disease trend, efficiently using these data to reveal public health insights. Time period and cohort effects could help in identifying the causes of mortality trends according to periods and birth cohorts in every country/region (3,19,20), thereby revealing information about the efficacy of CAVD-related health care services. Calculating local drift values, which enables recording of time trends in mortality for every age group and correcting the period effects, is another important area of development (13,16). Furthermore, use of overall rates to assess changes in mortality and DALYs would ignore important information about differences among age, period, and birth cohort. Therefore, the APC model was used to facilitate in-depth understanding of CAVD epidemic trends. Ours was also the first study to analyze trends of the main variable risk factors for CAVD in countries and regions at different SDI levels and by sex, which will help clarify the cause of changes in mortality and DALYs to develop targeted prevention and treatment strategies.
The global population has increased by 44.6% in the past 30 years (2,3). The number of deaths related to CAVD increased from 53,300 (95% UI: 47,760–59,730) to 126,830 (95% UI: 105,600–1,413,900), an increase of 138%. The burden of CAVD disease (deaths) has increased more than 3 times faster than the population growth rate. Although countries and regions with higher SDI levels currently have higher age-standardized DALY rates and age-standardized mortality rates, most showed a decreasing trend. In contrast, countries and regions with lower SDI levels (especially for men) showed no significant improvement or even an increasing trend for these indicators. In 2019, countries and regions with medium, medium-low, and low SDI accounted for 77% of the global population (2,3), which means that if CAVD prevention and treatment are not improved in countries and regions with lower SDI levels, this could result in a large disease burden in the future.
CAVD usually affects people with a normal trilobar aortic valve and occurs more frequently in patients with a congenital bilobar aortic valve (21). Clinically, CAVD is significant because a severe obstruction may result in symptoms and left ventricular failure and require surgery or a transcatheter valve replacement (4,21,22). Limited access to surgical or transcatheter valve replacement treatment and care appears to be an important reason some countries and regions have failed to make progress in reducing the disease burden. There have been studies that have reported that the mean number of cardiac operations in low-income countries and regions was seen to be only 0.5 per million, which was 1/1,000th of the average number of people in middle- and high-income countries and regions (23). For example, Pakistan, which is the second largest country in South Asia, with a population of 224 million, has only 4 medical institutions and a few specialists to perform cardiac surgery (24). Existing global efforts cannot meet the growing demand for CAVD surgery and care in low-income countries and regions. Although humanitarian medical assistance that provides nursing and surgical skills has long-term social benefits, many projects have failed to expand and implementation may even be reduced owing to limitations in medical volunteers, equipment, and funding (25,26). Additionally, control of risk factors cannot be ignored. The 3 risk factors mentioned above have been reported in previous studies (4,18), and the risk factors of a high sodium diet and high systolic blood pressure have remained nearly unchanged over 30 years in low- and medium-low-SDI regions; lead exposure has even shown an increasing trend. In contrast, high-SDI regions show an overall decreasing trend, which will further widen health disparities around the world.
This study serves as a detailed examination of illness patterns using GBD data. Use of the APC model to analyze disease trends by age, period, and population to determine additional causes of non-communicable diseases provides a more precise indication regarding efficacy of the health system response that goes beyond conventional epidemiological indicators and hence aids in monitoring progress toward the sustainable development goals in a particular country/region.
This study has several limitations. First, the analysis is subject to limitations derived from the GBD model owing to limited availability of original data from low- and middle-income countries and regions and the fact that estimated values are derived using data from high-resource environments. Better original data on disease deaths and DALYs lost are urgently needed in many low- and middle-income countries and regions (6,19). Therefore, further argumentation for the national context is needed before our views can be translated into public health policy. Second, GBD studies have used exclusive causes and specific causes of death. For middle-aged and older patients with multiple diseases at the same time, death may not be attributable to CAVD (4). Hence, the actual mortality rates in GBD studies could be underestimated and the actual situation may be more serious.
Conclusions
Globally, the number of CAVD patient deaths and DALYs lost have increased rapidly over the past 30 years. Currently, most countries and regions with higher SDI levels have higher age-standardized DALYs and mortality rates, but most show a decreasing trend. In contrast, countries and regions with lower SDI levels (especially for males) show no significant improvement or even an increasing trend for these indicators. Over the past 30 years, adverse period and cohort effects have been discovered in many countries and regions with different SDI levels, especially lower levels. The main variable risk factors of CAVD have shown a decreasing trend only in countries and regions with high SDI, with nearly no improvement or even an increasing trend in countries and regions with lower SDI. This suggests that health disparities between regions are expanding and could lead to a heavy burden of disease in the future. Health authorities and policy makers must consider improving the allocation of resources, increasing access to health care resources, controlling variable risk factors, and urgently improving efforts to curb growth of the disease burden.
Acknowledgments
This study benefits from the high-quality data of previous studies; the true generosity of such authors has advanced cardiovascular medicine.
Funding: This evaluation study was supported by the Fundamental Research Funds for the Central Universities (No. 2019PT350005), National Natural Science Foundation of China (No. 81970444), Beijing Municipal Science and Technology Project (No. Z201100005420030), National High Level Talents Special Support Plan (No. 2020-RSW02), CAMS Innovation Fund for Medical Sciences (No. 2021-I2M-1-065), and Sanming Project of Medicine in Shenzhen (No. SZSM202011013).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-480/rc
Peer Review File: Available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-480/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jtd.amegroups.com/article/view/10.21037/jtd-23-480/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Yadgir S, Johnson CO, Aboyans V, et al. Global, Regional, and National Burden of Calcific Aortic Valve and Degenerative Mitral Valve Diseases, 1990-2017. Circulation 2020;141:1670-80. [Crossref] [PubMed]
- Institute for Health Metrics and Evaluation. GBD Results Tool. 2019. Available online: https://ghdx.healthdata.org/gbd-results-tool
- Su Z, Zou Z, Hay SI, et al. Global, regional, and national time trends in mortality for congenital heart disease, 1990-2019: An age-period-cohort analysis for the Global Burden of Disease 2019 study. EClinicalMedicine 2022;43:101249. [Crossref] [PubMed]
- Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: Update From the GBD 2019 Study. J Am Coll Cardiol 2020;76:2982-3021. [Crossref] [PubMed]
- Yang C, Xu H, Jia R, et al. Global Burden and Improvement Gap of Non-Rheumatic Calcific Aortic Valve Disease: 1990-2019 Findings from Global Burden of Disease Study 2019. J Clin Med 2022;11:6733. [Crossref] [PubMed]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204-22. Erratum in: Lancet 2020;396:1562. [Crossref] [PubMed]
- Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study. Lancet 2006;368:1005-11. [Crossref] [PubMed]
- Knowles RL, Bull C, Wren C, et al. Mortality with congenital heart defects in England and Wales, 1959-2009: exploring technological change through period and birth cohort analysis. Arch Dis Child 2012;97:861-5. [Crossref] [PubMed]
- Rosenberg PS, Anderson WF. Proportional hazards models and age-period-cohort analysis of cancer rates. Stat Med 2010;29:1228-38. [Crossref] [PubMed]
- GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1160-203. [Crossref] [PubMed]
- GBD 2019 Risk Factors Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1223-49. [Crossref] [PubMed]
- Rosenberg PS, Anderson WF. Age-period-cohort models in cancer surveillance research: ready for prime time? Cancer Epidemiol Biomarkers Prev 2011;20:1263-8. [Crossref] [PubMed]
- Bell A. Age period cohort analysis: a review of what we should and shouldn't do. Ann Hum Biol 2020;47:208-17. [Crossref] [PubMed]
- Zou Z, Cini K, Dong B, et al. Time Trends in Cardiovascular Disease Mortality Across the BRICS: An Age-Period-Cohort Analysis of Key Nations With Emerging Economies Using the Global Burden of Disease Study 2017. Circulation 2020;141:790-9. [Crossref] [PubMed]
- Falcaro M, Castañon A, Ndlela B, et al. The effects of the national HPV vaccination programme in England, UK, on cervical cancer and grade 3 cervical intraepithelial neoplasia incidence: a register-based observational study. Lancet 2021;398:2084-92. [Crossref] [PubMed]
- Rosenberg PS, Check DP, Anderson WF. A web tool for age-period-cohort analysis of cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev 2014;23:2296-302. [Crossref] [PubMed]
- R Core Team R. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing, 2021. Available online: https://stat.ethz.ch/pipermail/r-announce/2003/000385.html
- Yi B, Zeng W, Lv L, et al. Changing epidemiology of calcific aortic valve disease: 30-year trends of incidence, prevalence, and deaths across 204 countries and territories. Aging (Albany NY) 2021;13:12710-32. [Crossref] [PubMed]
- GBD 2017 Congenital Heart Disease Collaborators. Global, regional, and national burden of congenital heart disease, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Child Adolesc Health 2020;4:185-200. Erratum in: Lancet Child Adolesc Health 2020. [PubMed]
- Wu W, He J, Shao X. Incidence and mortality trend of congenital heart disease at the global, regional, and national level, 1990-2017. Medicine (Baltimore) 2020;99:e20593. [Crossref] [PubMed]
- Kodra A, Kim M. Calcific Aortic Valve Stenosis with Aging and Current Development in its Pathophysiology. Int J Angiol 2022;31:229-31. [Crossref] [PubMed]
- Paolisso P, Beles M, Belmonte M, et al. Outcomes in patients with moderate and asymptomatic severe aortic stenosis followed up in heart valve clinics. Heart 2022; Epub ahead of print. [Crossref] [PubMed]
- Zilla P, Yacoub M, Zühlke L, et al. Global Unmet Needs in Cardiac Surgery. Glob Heart 2018;13:293-303. [Crossref] [PubMed]
- Khokhar RA, Gowa MA, Bangash SK, et al. The Spectrum of Pediatric Cardiac Procedures and Their Outcomes: A Six-month Report from the Largest Cardiac Facility in Sindh, Pakistan. Cureus 2019;11:e5339. [Crossref] [PubMed]
- Cardarelli M, Vaikunth S, Mills K, et al. Cost-effectiveness of Humanitarian Pediatric Cardiac Surgery Programs in Low- and Middle-Income Countries. JAMA Netw Open 2018;1:e184707. [Crossref] [PubMed]
- Nguyen N, Jacobs JP, Dearani JA, et al. Survey of nongovernmental organizations providing pediatric cardiovascular care in low- and middle-income countries. World J Pediatr Congenit Heart Surg 2014;5:248-55. [Crossref] [PubMed]
(English Language Editor: J. Jones)


